The recreational use of illicit drugs remains an enormous and growing problem throughout the United States of America and around the world. The use of these compounds carries a social and financial price through many avenues including increased utilisation of healthcare services. Illicit drugs may lead to chronic illnesses requiring therapy, and there is the ever-present risk for sudden catastrophic events, frequently due to cardiovascular origin.
As Figure 1 shows, the use of illicit drugs among high-school seniors in the United States of America is roughly 40%. This number has been stable over the last 20 years.Reference Johnston, Miech, O’Malley, Bachman and Schulenberg 1 Figure 2 breaks down the drug use by individual drugs. 2 Although marijuana continues to be the most frequently used drug, the use of stimulant medications rises significantly during the course of high school. Not shown on these graphs is the recent explosion of heroin use. This appears to be linked to the increased use of prescription pain medications.
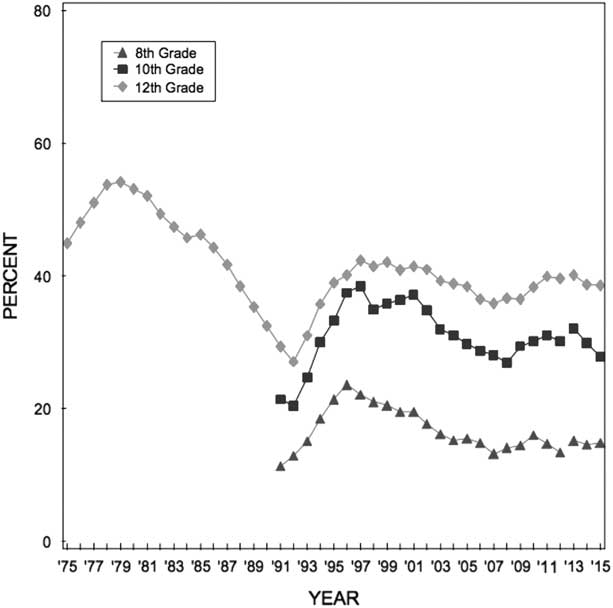
Figure 1 Trends in annual prevalence of use of an illicit drug in grades 8, 10, and 12. Retrieved from http://www.monitoringthefuture.org

Figure 2 Illicit and prescription drugs of abuse amongst middle- and high-school children. From the National Institute on Drug Abuse and retrieved https://www.drugabuse.gov/publications/drugfacts/high-school-youth-trends
As a cardiovascular provider, it is important to recognise the potential mechanisms that can be responsible for health problems created by these drugs’ use. This short review will outline some of the negative cardiovascular effects of the more common illicit drugs and in particular the mechanisms leading to sudden cardiac death.
Cocaine
Cocaine is most frequently thought of when considering the cardiovascular toxicity of illicit drugs. The association of cocaine use with sudden death due to myocardial ischaemia and infarction is well recognised. The differential diagnosis of all young patients, and even in older patients with no history of ischaemic heart disease, presenting to an emergency room with chest pain usually includes cocaine use. Certainly any adolescent presenting with evidence for myocardial ischaemia needs a full evaluation for potential cocaine intoxication. In a review of all non-traumatic sudden deaths occurring in southwest Spain, 3.1% were found to involve cocaine use.Reference Lucena, Blanc and Jurado 3
Cocaine is still used clinically as a local anaesthetic agent because of its ability to inhibit local electrical nerve transmission via blockade of sodium channels. When delivered systemically, cocaine can have direct effects on myocardial conduction and can lead to an electrocardiographic pattern mimicking Brugada syndrome.Reference Littmann, Monroe and Svenson 4 Clinically relevant systemic concentrations of cocaine can also inhibit the KCNH2 channel,Reference Ferreira, Crumb, Carlton and Clarkson 5 leading to a prolongation in the QT interval.
Cocaine is rapidly absorbed through all mucous membranes. It can be inhaled, injected, or smoked. Cocaine’s acute cardiovascular toxicity is due to activation of the autonomic nervous system leading to a supply-and-demand mismatch for oxygen. Cocaine acts by inhibiting the reuptake of catecholamines at sympathetic nerve terminals, the stimulation of central sympathetic outflow, and increased sensitivity of adrenergic nerve terminals to noradrenalin.Reference Lange and Hillis 6 , Reference Vongpatanasin, Mansour, Chavoshan, Arbique and Victor 7 This increases myocardial contractility, heart rate, and blood pressure. All of these contribute to increased myocardial oxygen demand. At the same time, cocaine use leads to coronary vasoconstriction and thrombosis via complex mechanisms including the inhibition of nitric oxide synthesis, enhanced release of endothelin-1, increased release of fibrinogen and von Willebrand factor.Reference Hobbs, Moore, Penkala, Bolgiano and Lopez 8 – Reference Mo, Singh, Arruda and Dunea 10 Laboratory studies have also shown that cocaine may decrease protein C and anti-thrombin 3 concentrations as well as increasing thromboxane production, all of which promote thrombotic coronary occlusion.Reference Mouhaffel, Madu, Satmary and Fraker 11 , Reference Togna, Tempesta, Togna, Dolci, Cebo and Caprino 12 This combination of actions can induce myocardial ischaemia and infarction even in individuals with no atherosclerotic disease.
Although individuals are at risk for a sudden catastrophic event with even a single use, chronic use has also been linked to cardiac pathological gross and ultrastructural changes and increased risk for sudden death. These include myocarditis, cardiac hypertrophy, dilated carding myopathy, and accelerated atherosclerotic disease.Reference Brickner, Willard, Eichhorn, Black and Grayburn 13 – Reference Willens, Chakko and Kessler 16
Cocaine is frequently used in combination with alcohol and cigarette smoking. Both of these appear to potentiate the risk for cardiovascular events due to cocaine. With the concurrent consumption of ethanol and cocaine, cocaethylene is produced in the liver. Cocaethylene slows down cardiac conduction and delays repolarisation through inhibition of sodium and potassium channels.Reference Wilson, Henning, Suttheimer, Lavins, Balraj and Earl 17 , Reference Xu, Crumb and Clarkson 18 Cocaethylene also inhibits the re-uptake of dopamine in the synaptic terminal.Reference Jatlow, Hearn, Elsworth, Roth, Bradberry and Taylor 19 Cocaine and cigarettes in combination increase myocardial oxygen demand to a greater degree than the two do individually.Reference Moliterno, Willard and Lange 20 Cigarette smoking by itself is known to cause endothelial dysfunction and platelet aggregation, which augments cocaine’s effects.
Stimulants
Amphetamine is a drug isolated from the plant Ephedra sinica and causes central nervous system stimulation. This drug has been used in Chinese medicine for over 5000 years and is known as ma huang. It was also used commonly in the United States of America as a nasal decongestant, bronchodilator, in the treatment for narcolepsy, and in that for hyperactivity in children. Methamphetamine, or crystal meth, is an amphetamine derivative that is easy to produce and may be taken orally, intravenously, or inhaled. Dextroamphetamine is another amphetamine derivative frequently used to treat attention deficit hyperactivity disorder.
Like cocaine, amphetamine and its derivatives lead to indirect stimulation of the autonomic nervous system through the release of norepinephrine, dopamine, and serotonin in nerve terminals of the central and autonomic nervous systems. Amphetamine lacks the ion channel-blocking properties of cocaine. The activation of the sympathetic nervous system leads to tachycardia and vasoconstriction, with pharmacokinetics and pharmacodynamics varying widely between individuals. Similar to cocaine, coronary artery spasm may be induced in individuals with or without atherosclerotic disease and may lead to myocardial infarction.Reference Bashour 21 , Reference Derlet, Rice, Horowitz and Lord 22
3,4-methylenedioxymethamphetamine (MDMA) or ecstacy is also a synthetic derivative of amphetamines and is produced in pill format. MDMA was first introduced into medicine by Merck & Co. as an appetite suppressant and was also found to be effective in treating alcoholism and depression. It became a popular street drug in the 1970s and grew in use during the late 1980s and 1990s, when it became associated with raves. Like other stimulants, it results in sympathetic stimulation leading to an increase in blood pressure and heart rate. Its metabolites may also result in vasospasm and thrombosis leading to myocardial infarction, ventricular arrhythmias, and sudden death.Reference Schifano, Oyefeso and Corkery 23 Unique to MDMA, it may also activate the 5-HT2B serotonergic receptors leading to pulmonary artery hypertension and valvular heart disease, similar to that seen with the now-banned appetite suppressant fen-phen.Reference Setola, Hufeisen and Grande-Allen 24
Cannabinoids
With the movement across the United States of America to legalise marijuana, or cannabis, for medicinal and recreational purposes, it is important to consider its potential deleterious effects. Marijuana has long been thought to have very few adverse effects with the exception of long-term dependence. There are, however, scattered reports of acute adverse events up to and including sudden death. These appear to be due to myocardial infarction.Reference Casier, Vanduynhoven, Haine, Vrints and Jorens 25
Cannabis has a biphasic effect on the autonomic nervous system. At low or moderate doses it causes tachycardia and hypertension due to increased sympathetic output and parasympathetic withdrawal, whereas higher doses inhibit sympathetic outflow and increase parasympathetic activity leading to bradycardia and hypotension. Cannabinoids have been shown to have limited direct effects on cellular electrophysiology, including shortening of the action potential duration and effective refractory period.Reference Miller, Dhingra, Kanakis, Amat-y-Leon and Rosen 26 This may predispose to atrial tachyarrhythmias.Reference Fisher, Ghuran, Vadamalai and Antonios 27 Myocardial ischaemia from coronary vasospasm has also been reported.Reference Fisher, Ghuran, Vadamalai and Antonios 27 This would be counter to Willie Nelson’s thoughts that marijuana “can only kill you if a bail of it falls on you”. The adverse effects of marijuana also appear to be potentiated with concomitant use of cocaine, alcohol, or amphetamines .
Over the last decade, there has been increasing use of synthetic cannabinoids such as “K2” and “spice”. These are synthetic compounds that are sprayed onto dried shredded plant material to smoke, or sold in liquid form. They were originally marketed as a safe and legal alternative to marijuana. The effects have been described as “cannabis like”. One advantage of these drugs for the user is that they do not show up on routine toxicology screening, though pharmacologically they act by activating the same receptors as the natural cannabinoids. Similar to marijuana, there have been isolated cases of myocardial infarction in otherwise healthy young persons that appear to be related to synthetic marijuana use.Reference Mir, Obafemi, Young and Kane 28 The effects of synthetic marijuana may in fact be more profound, as they may be significantly more potent than naturally occurring marijuana. Synthetic marijuana has been declared a controlled substance by the Food and Drug Administration.
Heroin
Heroine is a semi-synthetic analogue of morphine and acts directly on the vasomotor centre of the brain, increasing parasympathetic and decreasing sympathetic activity. Additionally, it activates mast cells to release histamine. In combination, the haemodynamic results are bradycardia and hypotension. Although accidental deaths due to heroin use are usually due to respiratory depression, an increase in cardiac automaticity is also observed with frequent ectopic atrial and ventricular beats, atrial fibrillation, and possibly ventricular tachycardia/fibrillation.Reference Lipski, Stimmel and Donoso 29 Of note for heroin addicts in methadone treatment programmes, methadone has been associated with QT prolongation and ventricular arrhythmias. This, however, is thought to be a rare event.Reference Anchersen, Clausen, Gossop, Hansteen and Waal 30
Conclusion
The recreational use of illicit drugs remains a significant problem around the world. The incidence of sudden death associated with the use of these drugs varies from rare in the case of marijuana use to not infrequent with some drugs such as cocaine. With all illicit drugs, their use is associated with an increase in risk for sudden death above that of the general population. It is important for care providers to recognise the potential for drug abuse when caring for a sudden cardiac arrest survivor or an otherwise healthy individual presenting with chest pain and electrocardiographic abnormalities suggesting ischaemia.
Acknowledgements
None.
Financial Support
This research or review received no specific grant from any funding agency or from commercial or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all referenced work contributing to this review complies with the ethical standards of biomedical or medicolegal investigation.




