Introduction
The Eustachian tube is passively closed, opening momentarily to maintain middle-ear function. Eustachian tube dysfunction is a common condition seen in ENT clinics, whereby the Eustachian tube may be obstructed or remain patulous, leading to impaired tubal function and resultant otological symptoms or sequelae. Dysfunction may be continuous, or individuals may only experience Eustachian tube dysfunction related symptoms such as fullness and pain during increased demand on Eustachian tube function, like rapid ambient pressure changes, such as those that occur during aeroplane travel or when diving.1
Despite an increase in the use of surgical techniques like balloon Eustachian tuboplasty, obstructive Eustachian tube dysfunction remains mostly managed through conservative and medical approaches. One medical treatment is the use of intranasal decongestants such as xylometazoline and oxymetazoline, both imidazoline derivatives. These are α2-agonists that act primarily on the postsynaptic terminals of sympathetic nerves of the nasopharyngeal mucosa, causing vasoconstriction in the venous sinusoids.Reference Corboz, Rivelli, Mingo, McLeod, Varty and Jia2 This leads to reduced nasal congestion by decreasing blood flow and increasing sinus emptying into capacitance vessels.Reference Hall and Jackson3,Reference Proctor and Adams4 These topical decongestants may also exert anti-inflammatory effects by inhibiting nitric oxide synthase and by acting as antioxidants.Reference Westerveld, Scheeren, Dekker, Griffioen, Voss and Bast5,Reference Westerveld, Voss, van der Hee, de Haan-Koelewijn, den Hartog and Scheeren6
Decongestant drugs may in theory serve to potentiate the opening of the Eustachian tube, but objective measurements of Eustachian tube function following their application are few and far between in the literature,Reference Ovari, Buhr, Warkentin, Kundt, Ehrt and Pau7,Reference Meyer, Mikolajczak, Korthäuer, Jumah, Hahn and Grosheva8 thus their efficacy may not be entirely robust. Despite limited evidence supporting decongestant use,Reference Jensen, Leth and Bonding9 the use of topical decongestants for short periods to treat symptoms of obstructive Eustachian tube dysfunction is common. For example, they are often used before a flight in otherwise asymptomatic individuals, to prevent the pain and other symptoms associated with baro-challenge-induced Eustachian tube dysfunction.10,11
There are many methods to objectively assess Eustachian tube function. Previously, our group has investigated the repeatability and correlation of several Eustachian tube function tests when applied in healthy subjects and individuals affected by Eustachian tube dysfunction.Reference Smith, Takwoingi, Deeks, Alper, Bance and Bhutta12,Reference Smith, Zou, Baker, Blythe, Hutchinson and Tysome13 We have also identified the optimal methods and patient manoeuvres for some of these tests.Reference Smith, Blythe, Baker, Zou, Hutchinson and Tysome14 Given the evidence gap regarding the effects of topical decongestants on Eustachian tube function, we apply our findings from previous work to this present study.
The current study aimed to investigate objective measurements of Eustachian tube function following the application of a topical nasal decongestant, xylometazoline hydrochloride, when sprayed in the anterior part of the nasal cavity. Our focus in this study was on individuals with milder forms of obstructive Eustachian tube dysfunction who were asymptomatic at the time of testing, and those without symptoms of Eustachian tube dysfunction.
It is known that a continuous spectrum of Eustachian tube function exists within the population, ranging from normal intermittent opening to permanently open or closed states. Most asymptomatic patients open their Eustachian tube 80–95 per cent of the time during function testing.Reference Smith, Blythe, Baker, Zou, Hutchinson and Tysome14 We wished to explore the effect of decongestant on Eustachian tube function in this group, and in those with baro-challenge-induced obstructive Eustachian tube dysfunction who have adequate Eustachian tube function in stable conditions. Nasal decongestants cannot be used for prolonged periods, and so are clinically of most interest in this cohort, based on their proposed ability to improve baseline Eustachian tube function in order to manage anticipated increased demand.
Materials and methods
Subjects
Written consent was obtained from all participants. A group of volunteers was recruited by advertisement from medical student and staff cohorts, including a mix of those without symptoms and those with symptoms of obstructive Eustachian tube dysfunction. Screening excluded those with a history of nasal obstruction or a recent upper respiratory tract infection. Volunteers were also excluded if the ear was otoscopically abnormal or associated with a Jerger type B tympanogram trace (226 Hz tone at 85 dB SPL, assessed using a Titan IMP440 device; Interacoustics, Assens, Denmark), as these can impact test results. All volunteers completed the Cambridge Eustachian Tube Dysfunction Assessment to screen for symptoms associated with Eustachian tube dysfunction, but this did not form part of the inclusion criteria.
Intervention
Eustachian tube function tests were conducted before and 15 minutes following the topical application of a nasal decongestant spray (xylometazoline hydrochloride 0.1 per cent, Otrivine; GlaxoSmithKline, Brentford, UK). Two sprays of decongestant were applied in the anterior part of the nostril on the test side, directed posteriorly towards the nasopharynx, with a further two sprays applied after a 5-minute interval. Volunteers were asked to confirm that they tasted the medication immediately following application.
Eustachian tube function tests
The following Eustachian tube function tests were used and have been described in summary. All tests were performed with the volunteer seated, conducted by one of two trained investigators working in a pair. Each volunteer had only one ear tested, with the side chosen based on either pre-existing Eustachian tube dysfunction symptoms (i.e. affected side was selected) or volunteer preference if asymptomatic. A schematic of the testing regimen is shown in Figure 1.
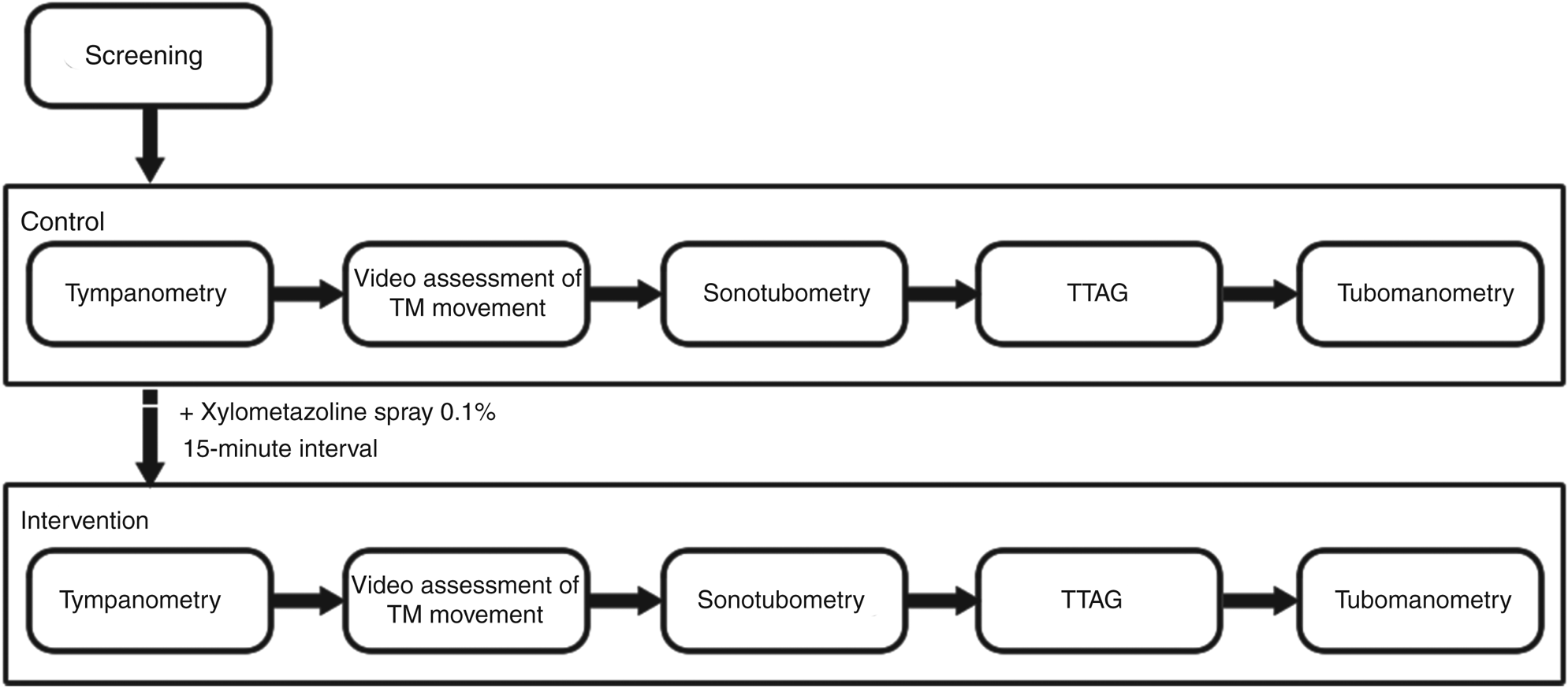
Fig. 1. Schematic of the testing regimen. Tests were carried out sequentially, with intra-test repeats carried out immediately. TM = tympanic membrane; TTAG = tubo-tympano-aerodynamic-graphy
Tympanometry
The tympanometer probe was inserted into the external auditory canal, and middle-ear pressure and compliance readings were recorded, repeated three times.
Video assessment of tympanic membrane movement
Volunteers performed a Valsalva manoeuvre under video otoscopic examination of the tympanic membrane (using a Teslong NTE100 digital otoscope; Shenzhen Teslong Technology, Shenzhen, China). Deflection of the pars tensa was recorded as Eustachian tube opening. Volunteers were asked to provide a subjective report of whether their Eustachian tube had opened during the manoeuvre based on perceived pressure change, pops or crackling sounds in the ear under test during the manoeuvre.
Tubo-tympano-aerodynamic-graphy
Ear canal pressure assessment during manoeuvres, known as tubo-tympano-aerodynamic-graphy, was conducted while asking participants to perform three Valsalva manoeuvres. Pressure measurements were obtained with a commercial Eustachian tube testing device (JK-05AD; Rion, Tokyo, Japan). Nasopharyngeal pressure was measured concurrently using a pressure meter (Testo 510; Testo, Lenzkirch, Germany) coupled to a sealed nasal probe. Tubo-tympano-aerodynamic-graphy used with Valsalva manoeuvres assesses passive Eustachian tube opening in isolation.
Sonotubometry
Sonotubometry was also conducted using the JK-05AD device mentioned above. A nasal speaker was held to the ipsilateral nostril of the ear under test and directed posteriorly towards the pharyngeal opening of the Eustachian tube. The speaker generated a 7 kHz full-octave band noise, to a maximum output of 123 dB. The system had been calibrated to the participant using a baseline of 50 dB SPL detected with a microphone in the external ear canal (typical speaker output after calibration was around 110 dB). The ear canal sound pressure level was displayed graphically after filtering, and peak and opening duration were recorded following five voluntary swallows without water. Sonotubometry used with swallowing assesses active Eustachian tube opening in isolation.
Tubomanometry
A nasopharyngeal pressure of 400 daPa was rapidly applied through a sealed nasal probe, with the timing of this automatically synchronised with deglutition by the tubomanometer (Spiggle and Theis, Overath, Germany). A pressure probe in the external ear canal under investigation allowed transmitted pressure changes in the middle ear to be recorded. The latency of Eustachian tube opening following the nasopharyngeal pressure increase, named the R value, was calculated through standard methods.Reference Schröder, Lehmann, Korbmacher, Sauzet, Sudhoff and Ebmeyer15 The test was repeated three times. Tubomanometry assesses combined active and passive Eustachian tube opening.
Statistical analysis
All data were analysed using IBM SPSS Statistics® software, version 25.0, and Microsoft Excel® spreadsheet software. The Shapiro–Wilk test demonstrated non-normality in some datasets; hence, the Wilcoxon signed-ranked test was applied to make pairwise comparisons between the control and intervention datasets.
Datasets were then dichotomised (using previously established thresholds for Eustachian tube openingReference Smith, Blythe, Baker, Zou, Hutchinson and Tysome14) to yield Eustachian tube opening rates. McNemar's test was applied to determine whether changes in Eustachian tube opening rates between the two groups were statistically significant.
Results
A total of 21 ears from 21 volunteers (13 males and 8 females; mean age of 23 years, range = 21–48 years) were examined. The median Cambridge Eustachian Tube Dysfunction Assessment score was 11, with a range of 10–18. Based on Cambridge Eustachian Tube Dysfunction Assessment scores, eight individuals had experienced obstructive Eustachian tube dysfunction related symptoms during situations of significant ambient pressure change (baro-challenge). With simple instruction, all participants were able to perform the required manoeuvres.
Effect on ambient middle-ear pressure
The median resting middle-ear pressure, as measured through tympanometry, was found to be −13 daPa before the intervention and −9 daPa following administration of the decongestant spray (p = 0.286, Wilcoxon's signed-rank test).
Effect on maximum nasopharyngeal pressures
In line with previously noted findings by our group, the maximum nasopharyngeal pressure attained during Valsalva manoeuvres differed between individuals; however, no significant difference in the maximum pressure was found before and after the intervention (p = 0.543, Wilcoxon's signed-rank test).
Effect on Eustachian tube opening rates
The Eustachian tube opening rates were in line with previously reported data.Reference Smith, Blythe, Baker, Zou, Hutchinson and Tysome14 With all Eustachian tube function tests, the intervention failed to demonstrate a significant effect on the rate of Eustachian tube opening in either the whole cohort (Table 1) or the subgroup affected by baro-challenge-induced aural symptoms (data not shown).
Table 1. Comparison of dichotomous Eustachian tube opening rates before and after xylometazoline application
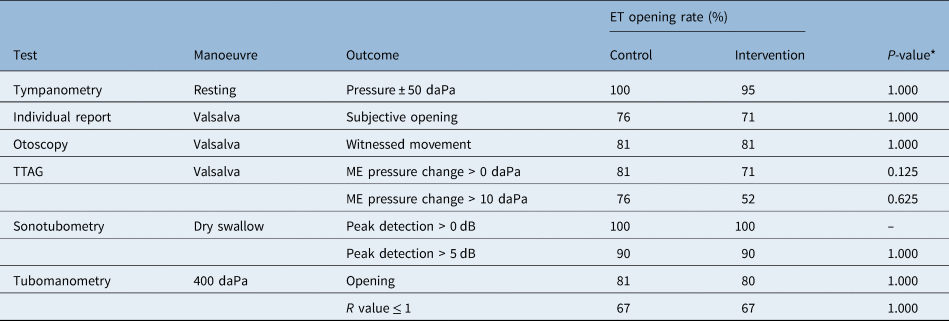
* P-values obtained through McNemar's test (n = 21). ET = Eustachian tube; TTAG = tubo-tympano-aerodynamic-graphy; ME = middle ear
Effect on Eustachian tube opening characteristics
Analysis of whether xylometazoline had an effect on continuous measures of Eustachian tube function was also performed, as shown in Table 2. A significant increase in the duration of Eustachian tube opening as measured through sonotubometry was found, but no differences were seen in the other continuous variables. For the subgroup experiencing baro-challenge-induced symptoms, there were no significant changes in continuous variables in response to xylometazoline spray administration (e.g. sonotubometry-measured opening duration, p = 0.944, Wilcoxon's signed-rank test).
Table 2. Comparison of continuous measures of Eustachian tube function before and after xylometazoline application

Data represent median values unless indicated otherwise.
* P-values obtained through Wilcoxon's signed-rank test (n = 21).
† P < 0.05
Discussion
Xylometazoline and other nasal decongestants are commonly suggested as a treatment for obstructive Eustachian tube dysfunction. Despite this practice, few studies have evaluated decongestants as treatments for Eustachian tube dysfunction, and even fewer have investigated their effects on objective measures of Eustachian tube function. Our study is novel in that we obtained measures of both passive and active Eustachian tube opening in adults using several of the available Eustachian tube function tests. As in previous work,Reference Smith, Blythe, Baker, Zou, Hutchinson and Tysome14 we found a spectrum of Eustachian tube function in those tested, with most asymptomatic participants demonstrating some intermittent failed Eustachian tube opening.
Xylometazoline is normally recommended for mild obstructive Eustachian tube dysfunction symptoms, particularly in individuals who are only symptomatic during rapid or significant changes in ambient pressure. We therefore wished to explore the effect of xylometazoline on Eustachian tube function in this cohort. We wanted to determine whether Eustachian tube opening rates in treated individuals can be potentiated, and approach a rate of 100 per cent during testing.
In an experimental rat study, Svane-Knudsen et al. showed that irrigation of the Eustachian tube with xylometazoline chloride 0.05 per cent led to a decrease in Eustachian tube opening pressure and lowered the steady-state pressure.Reference Svane-Knudsen, Kruse, Lildholdt and Madsen16 However, studies on human subjects have not shown such a clear effect on Eustachian tube opening or function. In one study, Jensen and colleagues applied topical xylometazoline chloride 0.1 per cent to the middle-ear ostium of the Eustachian tube in adult and adolescent patients with a dry tympanic membrane perforation.Reference Jensen, Leth and Bonding9 The rate of Eustachian tube opening with Valsalva manoeuvre significantly improved following the intervention, but the pressure equilibration test did not show a difference between the two groups; thus, the authors concluded that the decongestant's effects were only apparent at non-physiological pressures.Reference Jensen, Leth and Bonding9
In a more recent study, Ovari et al. evaluated the effects of intratympanic and nasal applications of xylometazoline 0.1 per cent on Eustachian tube opening, using pressure equalisation tests and tubomanometry.Reference Ovari, Buhr, Warkentin, Kundt, Ehrt and Pau7 Their results showed that nasal or intratympanic use of the decongestant had little to no effect on Eustachian tube opening. van Heerbeek et al. also found that topical nasal xylometazoline failed to improve Eustachian tube function in children with tympanostomy tubes inserted for otitis media with effusion, as measured through various tests (forced-response, pressure equilibration and sniff tests).Reference van Heerbeek, Ingels and Zielhuis17 Our study adds to a body of evidence showing that xylometazoline fails to improve Eustachian tube opening rates at normal atmospheric pressure, in either healthy individuals or those with a history of baro-challenge-induced obstructive Eustachian tube dysfunction.
Our study suggests that xylometazoline has a subtle effect on active Eustachian tube opening in healthy volunteers, increasing the duration of Eustachian tube opening as measured through sonotubometry. This, in part, correlates with a separate randomised, double-blinded study (published only in abstract form) of 34 adults with concurrent upper respiratory tract infection and normal Eustachian tube function, wherein the nasal application of xylometazoline had a positive effect on active Eustachian tube opening measured with sonotubometry.Reference Olen, Holmquist, Lim, Bluestone, Klein and Nelson18 The fact that a measurable change in Eustachian tube opening was registered suggests that the decongestant spray reached the pharyngeal opening of the Eustachian tube, which is something that has been questioned previously in the literature.Reference Ovari, Buhr, Warkentin, Kundt, Ehrt and Pau7,Reference Jensen, Leth and Bonding9 However, a change in Eustachian tube opening was only seen in one aspect of several tests applied, providing insufficient evidence on which to base this conclusion.
In our study, volunteers completed the Cambridge Eustachian Tube Dysfunction Assessment to identify those with symptoms associated with obstructive Eustachian tube dysfunction. Subgroup analysis of the data for the eight participants who experienced symptoms on baro-challenge revealed no improvement in either Eustachian tube opening rates or opening duration following xylometazoline treatment. The association between Eustachian tube function test results and symptoms associated with obstructive Eustachian tube dysfunction has been found to be limited,Reference Smith, Takwoingi, Deeks, Alper, Bance and Bhutta12 meaning that the effect of xylometazoline on symptoms should be considered separately. Interestingly, a previous qualitative randomised, controlled trial exploring the effect of topical nasal decongestant on symptoms during baro-challenge also found the decongestant little more effective than placebo.Reference Jones, Sheffield, White and Bloom19
Study limitations
Our mixed cohort contained only adults with healthy ears or limited symptoms of obstructive Eustachian tube dysfunction, in most cases based on symptoms on baro-challenge. However, previous work has also failed to demonstrate a clear effect of xylometazoline on Eustachian tube function in children or those with more pronounced obstructive Eustachian tube dysfunction.
Given the application method, there remains a question as to whether the dose of xylometazoline reaching the Eustachian tube orifice was sufficient for mucosal decongestion. Although our sonotubometry data suggest the drug may have reached the pharyngeal ostium, the dose may be too low to alter Eustachian tube opening rates to a significant degree at normal atmospheric pressure. However, in studies where topical xylometazoline has been more precisely directed at the Eustachian tube, the results are much the same, wherein xylometazoline fails to improve Eustachian tube opening at normal atmospheric pressures.Reference Jensen, Leth and Bonding9 While there are alternative methods for applying high-dose xylometazoline to the Eustachian tube mucosa that could be trialled in further work, techniques such as irrigation or middle-ear application methods are not practical for routine patient use.
• Eustachian tube dysfunction management often involves topical nasal decongestants, but objective evidence for their effect is lacking
• Several objective tests were employed to assess Eustachian tube function before and after xylometazoline application to the anterior nasal cavity, in healthy individuals
• Resting middle-ear pressures did not change following xylometazoline application
• Eustachian tube opening rate was not significantly altered following decongestant use, as measured by all tests used
• Sonotubometry data showed that xylometazoline spray increases Eustachian tube opening duration
• There is little to suggest that topical nasal decongestants affect Eustachian tube function in healthy individuals
Conclusion
Using a battery of tests to obtain objective measures of passive and active Eustachian tube function, our findings suggest that the baseline rate of Eustachian tube opening in healthy individuals and those reporting baro-challenge-induced obstructive Eustachian tube dysfunction symptoms is not altered following the application of xylometazoline to the anterior part of the nasal cavity. However, limited data suggest that the xylometazoline reaches the Eustachian tube, resulting in longer opening with swallowing. There remains little or no evidence that topical nasal decongestants improve Eustachian tube function, and clinicians should counsel patients about this when proposing treatment.
Acknowledgements
JRT and MES have received research funding from Spiggle and Theis, Overath, Germany. MES has received funding from the Cambridge Hearing Trust. The current research was carried out independently of this funding.
Competing interests
None declared





