Introduction
The population of adolescents and young adults with congenital heart disease (CHD) is rapidly expanding due to advances in diagnosis and management over the last several decades. The estimated US population of adults with CHD is at least 1 million,Reference Hoffman, Kaplan and Liberthson1,Reference Warnes, Liberthson and Danielson2 most of whom require lifelong cardiology care. A substantial proportion of this population has moderate or complex CHD and remains at risk for significant long-term cardiac morbidity and premature mortality in adulthood. Consequently, follow-up with a cardiologist with adult CHD expertise at a regional CHD centre is recommended for most patients, although this care is not always achieved.
Many patients with CHD experience long gaps in cardiac care around the age that children would typically be expected to transition from a paediatric to adult care model.Reference Mackie, Ionescu-Ittu and Therrien3–Reference Gurvitz, Valente and Broberg5 Studies have found that 61–83% of young adults are either lost to follow-up or experience a gap in care after leaving a paediatric institution.Reference Mackie, Ionescu-Ittu and Therrien3,Reference Yeung, Kay and Roosevelt4,Reference Wacker, Kaemmerer and Hollweck6 One group reported a median gap in care of 10 years,Reference Yeung, Kay and Roosevelt4 and several studies demonstrate that “lost” groups do include many patients with complex CHD.Reference Mackie, Ionescu-Ittu and Therrien3,Reference Gurvitz, Valente and Broberg5 Patients with gaps in cardiac care are more likely to require urgent procedural interventions, exhibit untreated complications related to their cardiac condition, have more frequent visits to the emergency department, and require higher rates of hospitalisation.Reference Yeung, Kay and Roosevelt4,Reference Wacker, Kaemmerer and Hollweck6–Reference Gurvitz, Inkelas and Lee8 Identifying interventions aimed at decreasing gaps in care may improve clinical outcomes in these patients.
The American College of Cardiology/American Heart Association Guidelines on the “Management of Adults with CHD” have emphasised the need for transition programmes to facilitate smooth movement from paediatric to adult-oriented healthcare environments, ideally beginning at 12 years of age.Reference Sable, Foster and Uzark9 We aimed to determine the impact of an institutional CHD Transition Clinic intervention on patient follow-up rates and transition readiness self-assessments.
Materials and methods
Study design and setting
We conducted a retrospective case–control study within a prospective quality improvement project at The Children’s Heart Center at the Medical University of South Carolina. Our Heart Center is the tertiary referral centre for paediatric cardiology providers throughout the state of South Carolina and is the sole paediatric and adult congenital cardiothoracic surgical site in the state. At this centre, a standardised approach of transferring paediatric CHD patients to adult cardiac care does not exist. The centre has an Adult Congenital Heart Program which is the typical transfer destination when it occurs. The CHD Transition Clinic was developed in January 2016 as a monthly subspecialised paediatric cardiac clinic designed to evaluate and promote patients’ preparation and transition towards adult-oriented cardiac care as they age. This new clinic and related data collection were designed as a quality improvement initiative using a Plan-Do-Study-Act model for frequent and cyclical impact assessments to drive ongoing programme improvements. As such, this study was deemed exempt from Institutional Review Board (IRB) review.
Study population
Patients were electively referred to the CHD Transition Clinic by their outpatient paediatric cardiologist rather than automatic enrolment of all eligible patients. Eligibility criteria for this clinic were patients ages 11 years and older with known CHD currently being followed in a general paediatric cardiology clinic. Exclusion criteria for the Transition Clinic were significant developmental delay, acquired or non-structural cardiac conditions (such as arrhythmia without CHD), and patients followed exclusively by the Heart Failure/Transplant team. In this initial clinic intervention analysis, subjects were included if they had completed at least one CHD Transition Clinic visit between January 2016 and March 2018.
Transition clinic procedure
Transition Clinic visits were led by the Clinic Director (attending paediatric cardiologist), assisted by the Transition team paediatric cardiology fellow, and an adult CHD nurse practitioner. Elements of the transition intervention are detailed in Figure 1. The intervention was designed utilising transition resources and tools from the GotTransition© site,Reference Health10 including the recommended patient age of transition process initiation, selected self-assessment questionnaires, and formal clinic policy letter outlining expectations and policies regarding the transition and transfer process. Aspects from existing transition clinics were also considered in designing the clinic, specifically from review of the CHAPTER studies piloted by the Edmonton cardiology group.Reference Mackie, Islam and Magill-Evans11 Additionally, participants also underwent any routine cardiac surveillance tests due at time of clinic visit, such as echocardiogram or electrocardiogram, and these results were reviewed during the visit. Participants were considered for transfer to Adult CHD care if they were 18 years or older, lacked major concerns identified on self-questionnaire scores, and were without an upcoming cardiac intervention or acute symptoms. The patient and family’s input were also considered.

Figure 1. CHD transition clinic intervention components. ACHA = Adult Congenital Heart Association; ACHD = Adult CHD; PedsQL = Pediatric Quality of Life Inventory.
Transition Clinic participants were asked to complete two questionnaires at the beginning of their visit. The Transition Readiness Assessment Questionnaire is a 20-item patient-report instrument that uses five subscales to assess self-management, self-advocacy, and health care utilisation skills. The tool is designed to be used regularly for screening, can be applied in various chronic illness populations, and has demonstrated good internal reliability and criterion validity.Reference Wood, Sawicki and Miller12,Reference Sawicki, Lukens-Bull and Yin13 Questions are worded at a Flesch–Kincade Grade Level of 5.7. Participants reply to questions with a self-rating ranging from 1 (“No, I do not know how”) to 5 (“Yes, I always do this when I need to”). A total score is generated by averaging the sum of all ratings, and subscale averages are similarly be generated; higher scores indicate greater readiness. The Pediatric Quality of Life Inventory 3.0 Cardiac Module is a multidimensional, disease-specific patient- and parent-proxy-report instrument developed to measure health-related quality-of-life dimensions in children and adolescents. It has demonstrated feasibility, reliability, and validity to measure health-related quality of life in paediatric cardiology patients (note that this validation data included subjects to a maximum of 18 years).Reference Uzark, Jones, Burwinkle and Varni14 The questionnaire contains 27 questions within six scales related to symptoms, treatment barriers, perceived physical appearance, treatment anxiety, cognitive problems, and communication. Answers utilise a five-point Likert scale (ranging from 0 to 4), and items are reverse-scored for transformation to a 0–100 scale such that higher scores indicate better health-related quality of life. Both the Transition Readiness Assessment Questionnaire and Pediatric Quality of Life Inventory Cardiac Module were provided to participants at their initial Transition Clinic visit as well as any Transition Clinic follow-up visits with a minimum 6-month interval between reassessments.
An electronic registry was created on a protected network-storage drive to efficiently track participants’ progress and continuation of care, whether in a paediatric or adult CHD clinic. The registry was updated periodically regarding participant follow-up status and questionnaire scores and to identify gaps in cardiac care. If a participant was noted to have missed the intended cardiology clinic follow-up visit, a telephone contact attempt was made to offer scheduling assistance.
Usual care “Control Group”
The control cohort was identified retrospectively from all patients seen in paediatric cardiology clinics prior to the institution of the CHD Transition Clinic over a 3-month timeframe (December 2015 to February 2016) to generate a representative subset “convenience sample”. Inclusion and exclusion criteria were identical to Transition Clinic participants as noted above. Additional exclusion criteria for the cohort were documentation of care transfer to another centre and ineligibility of follow-up completion opportunity due to recommended time interval being a future date at time of chart review (e.g., recommended follow-up in 5 years). Each control patient’s recommended follow-up time was noted, and cardiac follow-up visits that occurred were recorded. Transition readiness and quality-of-life questionnaires were not available for control subjects.
Outcomes
The primary outcome was participant “lost to follow-up” rate. This rate was identified by chart review and defined as a persistent absence from cardiac care for at least 6 months beyond the recommended follow-up time stated in the most recent clinic note, and without an upcoming visit scheduled or documentation of external transfer of care.
Secondary outcomes included Transition Clinic participant self-questionnaire scores, self-rated health-related quality of life, as well as trends in Transition Clinic patient transfer to adult CHD care. The following independent participant variables were investigated for significance in trends: sex, age, surgical or catheter-interventional history, surgical complexity risk score (Risk Adjustment for Congenital Heart Surgery, “RACHS-1” for the patient’s most complex surgery), and univentricular or biventricular heart. The proportion of adult Transition Clinic patients who completed transfer to adult care was examined.
Statistical analysis
Differences between intervention and control patients were tested using independent t-tests, Mann–Whitney U-tests, or chi-square tests, as appropriate. The distribution of data was tested using the Shapiro–Wilk test. Multivariable logistic regression was used to identify risk factors for being lost to follow-up. Independent variables were CHD Transition Clinic participation, sex, age, biventricular versus single ventricle physiology, history of surgery, history of cardiac catheterisation, and surgical complexity (Risk Adjustment for Congenital Heart Surgery) score. A p value less than 0.05 was considered statistically significant. All statistics were performed using IBM SPSS Statistics software v. 24 (manufactured in Armonk, NY).
Results
Lost to follow-up rate
A total of 53 participants had completed at least one visit in the CHD Transition Clinic at time of results analysis (March 2018, 26 months after clinic start date). The control cohort consisted of 54 patients who met inclusion and exclusion criteria for primary outcome assessment. Baseline characteristics of each group are summarised in Table 1. Groups were similar in median age at visit, proportion of patients <18 years old, history of surgery, and proportion of low-risk surgical complexity score; the intervention group consisted of significantly greater females, patients with univentricular heart physiology, and history of cardiac catheterisation. Among the Transition Intervention cohort, 41 subjects either already completed or were eligible to have completed a recommended follow-up cardiology visit at point of data review based on recommendation stated in the most recent provider note (e.g., typically a 6- or 12-month follow-up visit). Only 3/41 of these participants (7.3%) were lost to follow-up, significantly lower (p < 0.01) than the 14/54 (26%) of patients lost to follow-up in the control group using the same chart review definition criteria. Multivariable logistic regression analyses revealed that participation in the Transition Clinic was the only factor independently associated with cardiac care retention (odds ratio = 0.20, 95% confidence interval = 0.04–0.98, p = 0.048). Sex, age, surgical complexity risk score, univentricular heart, and history of cardiac catheterisation were not associated with being lost to follow-up.
Table 1. Baseline characteristics of participants

Differences between groups were assessed using Mann Whitney U-tests or chi-square tests as appropriate. “Low-risk” RACHS-1 score refers to scores 1–3 on a 1–6 scale.
RACHS-1 = Risk Adjustment for Congenital Heart Surgery.
A p value < 0.05 was considered significant.
Questionnaire assessments
The proportion of participants who completed questionnaires at their first Transition Clinic visit was 91% (48/53) for both the Transition Readiness Assessment Questionnaire and the patient Pediatric Quality of Life Inventory Cardiac Module; 37/53 (70%) simultaneous parent-proxy Pediatric Quality of Life Inventory Cardiac Modules were completed at this visit. Questionnaire scores are summarised in Table 2, listed in order of highest (i.e., better) to lowest reported transition readiness subscale or quality-of-life subscale. The lowest self-rated transition readiness subscale was “tracking health issues”, and lowest quality-of-life subscale area was “cognitive problems”. Quality-of-life total scores and subscale scores did not significantly differ between patient- and parent-reported reports, although there was a trend towards greater perceived problems in communication and with treatment anxiety by parent reports in comparison to patient reports.
Table 2. Initial visit mean questionnaire subscale scores (from highest to lowest reports)
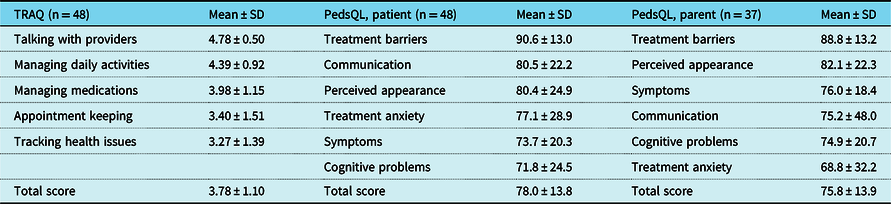
TRAQ, range 0–5 (maximum readiness = 5). PedsQL, range 0–100 (maximum quality of life = 100).
PedsQL = Pediatric Quality of Life Inventory; TRAQ = Transition Readiness Assessment Questionnaire.
Transition readiness, as measured by higher self-reported Transition Readiness Assessment Questionnaire scores, was significantly associated with older age (p = 0.01) but not sex, univentricular heart, surgical or catheterisation history, or surgical complexity score. History of cardiac surgery was the only variable associated with poorer total quality-of-life scores by patient report (p = 0.47) (Tables 3 and 4). Worse Pediatric Quality of Life “symptoms” subscale scores were significantly associated with history of cardiac surgery (mean score 68.8 ± 20.2 compared to 85.7 ± 15.0 in subjects without prior surgery, p < 0.01) and history of cardiac catheterisation (mean score 68.4 ± 20.6 compared to 82.5 ± 16.7 in subjects without prior catheterisation, p = 0.019).
Table 3. Differences in TRAQ total scores based on respondent demographic and clinical characteristics
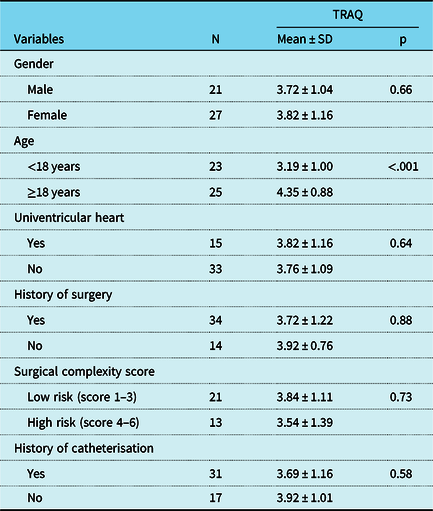
TRAQ, range 0–5 (maximum readiness = 5).
48 subjects within the intervention sample answered the TRAQ.
TRAQ = Transition Readiness Assessment Questionnaire.
Table 4. Differences in PedsQL 3.0 Cardiac Module total scores based on respondent demographic and clinical characteristics

PedsQL, range 0–100 (maximum quality of life = 100).
48 subjects within the intervention sample answered the PedsQL.
PedsQL = Pediatric Quality of Life Inventory.
At the time of data review, 23 participants (43% of the initial cohort) had completed a follow-up visit in the Transition Clinic. Mean time between visits was 11.6 months. Among these participants, 22 (96%) completed follow-up Transition Readiness Assessment Questionnaires and 20 (87%) completed follow-up patient Pediatric Quality of Life Inventory Cardiac Modules. Questionnaire scores and subscale scores did not significantly differ between initial visit and follow-up assessment.
Trends in transfer to adult congenital cardiac care
A total of 31 participants (58.5%) were of age 18 years or older at a Transition Clinic visit. Among these, chart review documented that 20 patients (65%) were offered transfer of care to an Adult Congenital Heart Disease clinic; 11 of these 20 patients (55%) completed transfer of care. Documented reasons for decline of transfer among this young adult cohort are listed in Table 5; not all patients had a specific reason cited in chart review. Of note, two of the three clinic participants who were lost to follow-up at chart review were over 18 years old at time of their Transition Clinic visit, and one had transferred to Adult Congenital Cardiac care.
Table 5. Reasons cited for lack of ACHD care transfer

Not all subjects had a cited reason in the clinic note available to chart review.
ACHD = Adult Congenital Heart Disease.
Discussion
Preparing youth with CHD for the transition from paediatric models of cardiac care to adult-oriented care is a challenging and ongoing clinical care issue. Contrary to some common patient misconceptions, many CHD conditions are palliated rather than cured and have important long-term implications for lifestyle, career choices, insurance, family planning, psychosocial issues, and other health comorbidities in adulthood necessitating longitudinal subspecialised follow-up. Transition of care involves a planned and continuous shift from paediatric family-centred care to adult patient-centred care. To do so successfully, patients must acquire and cultivate skills in self-management and self-advocacy, develop openness to independence and medical responsibility, and understand their condition including potential comorbidities. Clearly, this is a multi-faceted process requiring investment of the patient, family, and primary cardiology team at a minimum. There are many models used in clinical practice to attempt to improve the transition process for youth with CHD, with many examining structured CHD educational interventionsReference Ladouceur, Calderon, Traore, Cheurfi, Pagnon, Khraiche, Bajolle and Bonnet15–Reference Goossens, Fieuws and Van Deyk17 and others assessing interventions geared towards general health-management skills.Reference Acuña Mora, Sparud-Lundin, Bratt and Moons18,Reference Huang, Terrones and Tompane19 Measuring the short- and long-term impact of a transition program is challenging, and various goals and definitions of success exist. Improvement in patient medical knowledge is a frequently studied and quantifiable outcome.
To our knowledge, this is the first study to describe the success of a focused, clinic-based transition intervention in improving cardiology follow-up rates when compared to usual care alone. There is a growing body of literature about factors which seem protective against or predictive for lapses in care, though none have examined the impact of clinical interventions at improving overall cardiac care retention at this vulnerable broad age range (be this paediatric or adult CHD care). One similar intervention recently published by Mackie et al described the successful impact of a nurse-led educational intervention on timely transfer to adult CHD care.Reference Mackie, Rempel and Kovacs20 Mackie’s study differs from this described CHD Transition Clinic in the team’s assessment of a more narrow cohort (16- to 17-year olds with moderate or complex CHD) and in their more specific outcome of prompt transfer completion to adult CHD care. However, many paediatric cardiology clinics do not yet have a standardised approach in patient transfer to an adult team; additionally, evidence shows prevalent lapses in cardiac care for patients with mild forms of CHD and for younger age groups.Reference Mackie, Ionescu-Ittu and Therrien3,Reference Gurvitz, Valente and Broberg5,Reference Goossens, Stephani and Hilderson21,Reference Fernandes, Khairy and Fishman22 Therefore, our intervention broadened the outcome to examine overall maintenance of cardiac care in a wider patient cohort.
We theorise three primary contributors to the success of this transition intervention. One is the premise that the clinic’s focused education on CHD implications and health-management skills translates into better continuity of cardiac care. Many other groups are actively strategising and examining this focus on education with a similar assumption.Reference Sable, Foster and Uzark9,Reference Uzark, Jones, Burwinkle and Varni14–Reference Valente, Landzberg and Gianola16 The second potential contributor to care retention is the CHD Transition Clinic electronic registry database, which is specifically utilised by clinic team members to track and monitor participants’ recommended cardiology follow-up appointments as well as progression of self-reported transition readiness scores. This enables identification of a potential lapse in care continuity with a consequent reminder to the patient and/or family. This strategy can identify individual patient barriers to care maintenance at this vulnerable age period, such as financial difficulties, insurance changes or problems, transportation issues, or relocation. Lastly, we believe that the face-to-face introduction of a member of the Adult CHD care team emphasises the necessity and importance of lifelong care into adulthood and offers a personalised approach in preparation to transition to an adult model or transfer to adult team.
Participants’ baseline visit Transition Readiness Assessment Questionnaire scores suggest that our patient group would benefit most from strategies to improve skills needed for “Appointment-Keeping” (a self-management skill including scheduling appointments, following up on referrals for tests or labs, and managing health insurance coverage and finances) and “Tracking Health Issues” (a self-advocacy skill encompassing the ability to complete one’s medical history form, recall appointments and health questions, and obtain financial help with school or work). The finding that none of the transition readiness follow-up scores significantly changed on participants’ subsequent visits to CHD Transition Clinic highlights the probable need for improvement in implementing skills-based interventions. The low ratings in areas of cognitive problems and treatment anxiety by patients and parents on the Pediatric Quality of Life Cardiac Module support existing evidence regarding risks of neurocognitive deficits and psychosocial challenges that patients with CHD face. These concerns persist throughout adulthood and often affect overall quality of life and social roles.Reference Marino, Lipkin and Newburger23–Reference Karsenty, Maury and Blot-Souletie28 Impaired executive function and mental health issues can hinder self-management and advocacy skills necessary to independently navigate one’s health care needs, potentially impairing successful transition and maintenance of cardiac care. Early identification of such issues via transition clinic assessments can facilitate resource provision to improve care outcomes.
While physical transfer of patient care to Adult CHD subspecialist care was not the primary goal of this CHD Transition Clinic intervention in its initial stage, we identified interesting trends in referral and transfer to adult care. Although the majority of adult participants were offered transfer to adult CHD care, barely half (55%) of those offered pursued a transfer of care. One reason frequently described was a strong patient or family desire to remain with their paediatric cardiologist, which is a common theme among other studies and is related to patients’ attachment to the provider who has often known and managed the patient since infancy.Reference Lee, Bailey and Cullen-Dean29–Reference Gurvitz and Saidi31 We believe that incorporation of an Adult CHD team member early into transitional care planning may ameliorate this concern by bridging an introduction to a new care team and offering the opportunity to form a relationship prior to actual care transfer. Another frequently cited reason our adult patients forego transfer of care was a desire to complete an ongoing milestone such as post-secondary education or a potential relocation. This information may guide transition policies on timing for care transfer, such as upon the conclusion of schooling or by around age 22 years as suggested in other guidelines about adolescent health care transition policies.Reference Health10
Our study and results have several limitations. Its generalisability has inherent limits given the study design, including small sample size from a single centre. Subject information such as socioeconomic status and race was not recorded, so it is unknown if some populations were underrepresented in our cohort. The intervention cohort was predisposed to selection bias, as patients were enrolled solely by referral from their paediatric cardiologist who may possess reasons for referring or not referring patients of variable functioning levels. As the CHD Transition Clinic was developed as a quality improvement project, there was not a predefined prospective control cohort. Identification of a retrospective control cohort for this study with identical inclusion and exclusion criteria approximates similarity in the two groups and their characteristics, although there were significant differences in baseline characteristics (Table 1) which may introduce bias to our primary endpoint results. Additionally, identifying the primary outcome of “lost-to-follow-up” status by chart review may not reliably account for transfers of care to other centres if documentation does not occur, which would certainly impact results but is difficult to circumvent. Our centre does have the ability to view encounters for all paediatric or adult congenital cardiologists within a 2-hour radius of our centre, which helps capture many follow-up encounters. There are limitations of the interpretation of surrogate outcomes (questionnaires) rather than objective behaviours as outcomes. There was some variability in participants’ intervention “protocol” as the Transition Clinic team would also address issues typically discussed within a routine cardiology visit, which may at times identify more pressing disease-related concerns. It is not possible to discern the impact of the actual visit procedure on the primary outcome from the impact of the intentional contact attempt made to patients identified by registry as due for follow-up; we suspect both contribute to the unique success of this intervention compared to control group treatment. The available follow-up duration of transition intervention progress was limited to just over 2 years in order to assess preliminary pilot intervention progress and to describe results, and this relatively short timeframe limited total sample size. Lastly, while a transition intervention database registry holds powerful potential to impact care continuation and track patient outcomes, its upkeep and continuous management may be challenging with larger, and growing, participant cohorts.
In summary, this is the first study to our knowledge to demonstrate that an integrative clinic-based transition intervention can result in lower lost to follow-up rates among adolescents and young adults with CHD. The intervention protocol could be easily replicated by other programmes without requiring extensive resources. The self-report questionnaires to assess transition readiness and areas of cardiac health-related quality of life have good usability to track participant progress and to tailor interventions and resource provision. Utilisation of a database registry to identify lapses in care before they occur and offer patient assistance has tremendous potential to serve as a care tool. Future studies may investigate additional motivations and barriers for patient care continuation, development of an “app” to improve transition and communication between adolescents and the cardiac care team, and prospective assessments of additional clinic interventions to promote specific transition readiness skills or resource provision (such as mental health referrals or education-system collaboration). We would also be interested in testing the success of transition clinic policies influenced by these findings and to further evaluate the feasibility of maintaining an extensive patient database registry during this vulnerable time period where patients with CHD are at risk of significant interruptions of care.
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. As previously noted, IRB review was not required.








