Introduction
Epistaxis is the most common emergency in ENT practice.Reference Petruson and Rudin 1 , Reference Schlosser 2 It is estimated that around 60 per cent of the population have epistaxis in their lifetime, and around 6–10 per cent of patients seek medical attention for it. A survey conducted in the USA in 2004 reported that approximately 30 per cent of households had one or more members who had experienced recurrent epistaxis in their lifetime.Reference Benninger and Marple 3
Recurrent epistaxis is defined as troublesome, repeated nasal bleeds, often arising from Little's area.Reference Schlosser 2 , Reference Burton and Doree 4 This area is situated at the central part of the anterior septum where four arteries (anterior ethmoidal, sphenopalatine, greater palatine and superior labial) anastomose to form Kiesselbach's plexus.Reference Burton and Doree 4 – Reference Chiu and Dunn 6 Most cases of epistaxis (80–90 per cent) are idiopathic in origin.Reference Burton and Doree 4 , Reference Pope and Hobbs 5 Once secondary causes (e.g. haematological disorders, hereditary haemorrhagic telangiectasia, hypertension, neoplasms) are excluded, it is thought that crusting, vestibulitis, digital trauma and age-related nasal mucosal atrophy,Reference Burton and Doree 4 , Reference Pinto and Jeswani 7 or a combination of these, act as predisposing factors. Epistaxis is generally classified into anterior or posterior, depending on the site of bleeding. Anterior bleeds are responsible for around 80–95 per cent of epistaxis cases.Reference Pope and Hobbs 5
Different methods have been used to treat recurrent anterior epistaxis, including chemical cautery (the commonest being silver nitrate cautery),Reference Schlosser 2 , Reference Burton and Doree 4 , Reference Pope and Hobbs 5 , Reference Calder, Kang, Fraser, Kunanandam, Montgomery and Kubba 8 , Reference Murthy and Laing 9 antibiotic ointments,Reference Schlosser 2 , Reference Burton and Doree 4 , Reference Robertson and Kubba 10 monopolar or bipolar diathermy,Reference Pope and Hobbs 5 septal suturing,Reference Pope and Hobbs 5 hot wire cautery,Reference Schlosser 2 , Reference Pope and Hobbs 5 and use of a Harmonic® scalpel.Reference Kodama, Yoshida, Nomi, Fujita and Suzuki 11 The most common treatments for recurrent anterior epistaxis in the UK are antiseptic cream (Naseptin®) application, silver nitrate cautery or a combination of the two. Whilst the short-term effectiveness of these treatments has been reported at between 50 and 90 per cent, the medium- to long-term effectiveness is poor.Reference Schlosser 2 , Reference Benninger and Marple 3 , Reference Pope and Hobbs 5 , Reference Calder, Kang, Fraser, Kunanandam, Montgomery and Kubba 8 – Reference Robertson and Kubba 10 , Reference Ruddy, Proops, Pearman and Ruddy 12 A Cochrane review published in 2004 concluded that the optimal management of recurrent epistaxis in children remains unclearReference Burton and Doree 4 and recommended that further studies be conducted to explore other possible interventions.
The neodymium-doped yttrium aluminium garnet (Nd:YAG) and potassium titanyl phosphate (KTP) lasers, delivered with a fibre, have been widely reported as effective in controlling epistaxis secondary to hereditary haemorrhagic telangiectasia.Reference Pope and Hobbs 5 , Reference Harvey, Kanagalingam and Lund 13 , Reference Werner, Baumler, Zietz, Kuhnel, Hohenleutner and Landthaler 14 The KTP laser produces an emerald green laser at 532 nm wavelength, which is within the absorption peak for haemoglobin,Reference Clark, Cameron, Moseley, Ferguson and Ibbotson 15 , Reference Gossner, May, Stolte, Seitz, Hahn and Ell 16 making it especially effective for the treatment of vascular lesions.Reference Harvey, Kanagalingam and Lund 13 , Reference Clark, Cameron, Moseley, Ferguson and Ibbotson 15 This treatment is not generally offered to epistaxis patients without hereditary haemorrhagic telangiectasia, largely because the single-use fibre that delivers the laser beam is not cost-effective.
We describe a new technique, using a reusable Dermastat® handpiece, for delivering KTP laser to treat anterior epistaxis. The KTP laser Dermastat has been successfully used in the treatment of vascular lesions on the skin of the face.Reference Clark, Cameron, Moseley, Ferguson and Ibbotson 15 This novel laser delivery system consists of a handpiece, a focal applicator tip which attaches to the end of the handpiece, and a cable unit that can be connected to the KTP laser source easily (Figure 1). The choice of handpiece, with differing focal applicator tip sizes (1, 2 and 4 mm), gives the operator the ability to photocoagulate appropriate size vessels precisely. These handpieces are reusable. The small focal applicator tip, which comes into contact with the patient, can be removed and autoclaved, or sterilised as required. The Dermastat system is therefore more cost-effective than the single-use laser fibre delivery system. This study evaluates our early experience using the KTP laser Dermastat in the management of recurrent anterior epistaxis.

Fig. 1 Laser delivery system, comprising handpiece, cable and potassium titanyl phosphate laser delivery source.
Materials and methods
This prospective study was carried out at Poole Hospital NHS Foundation Trust, a secondary referral centre for otolaryngology. Fifty-eight patients who presented with recurrent epistaxis were included in the study. All patients were clinically assessed with a focused history and a complete ENT examination. Any obvious secondary causes for epistaxis were documented. Patient demographics, co-morbidities and previous epistaxis-related attendances were recorded prospectively in a database, along with the site and settings of KTP laser photocoagulation.
Patients with prominent or dilated blood vessels on the anterior part of the nasal septum, and/or patients for whom attempted initial treatment with silver nitrate cautery had failed, were included in the study. These inclusion criteria were chosen with the aim of isolating a treatment-resistant population. All patients with hereditary haemorrhagic telangiectasia and bleeding diathesis were excluded, as the success and widespread use of KTP laser in this population are well documented.
The main outcome measure was complete resolution of symptoms (i.e. no recurrence of epistaxis) at two months from the date of the procedure. Patients who did not report complete resolution at two months were either offered further treatment with silver nitrate cautery (if deemed clinically appropriate) or no additional treatment and further clinic follow up. All procedures were performed by one surgeon (PKJ).
Ethical standards
The authors assert that all procedures contributing to this work complied with the ethical standards of the relevant national and institutional guidelines on human experimentation, and with the Helsinki Declaration of 1975, as revised in 2008.
Surgical procedure
The procedure was performed under local anaesthesia if the patient was sufficiently compliant; young children received a general anaesthetic. The area on the septum requiring treatment was anaesthetised and decongested with co-phenylcaine (a mixture of lidocaine hydrochloride 5 per cent and phenylephrine 0.5 per cent topical solution). The septal area was cleared of mucus with the use of suction, and bleeding or dilated blood vessels were identified.
The patient's face was covered with a thick wet cotton pad, leaving only the nose exposed. A small water-soaked cotton wool ball was placed in the nose, posterior to the area being treated. These measures were taken to minimise the risk of accidental laser injury to surrounding tissues and the eyes.
Once the approximate size of the vessel had been assessed, a 1 or 2 mm Dermastat handpiece was connected to the KTP laser source. The settings used were as follows: fluence of 4–8 J/cmReference Schlosser 2 , with a pulse width of 4–8 ms, at 4 pulses per second, starting with the minimum power setting to induce blanching of the blood vessels. The power intensity was increased in small increments as necessary until desired blanching of the blood vessels was achieved. Figure 2 shows a 2 mm Dermastat handpiece in use.

Fig. 2 A 2 mm Dermastat handpiece in use.
Patients were given Naseptin® cream on discharge, to be used for two weeks, and were followed up in clinic at two months. Naseptin was supplied to patients for the prevention of premature scab detachment and prophylaxis against infection, rather than as a supplementary treatment for epistaxis.
At two months' follow up, a complete treatment evaluation was performed; this included assessment of whether complete resolution had been achieved and documentation of the presence of any complication (e.g. septal perforation, crusting, persistent pain). Patients who did not report complete resolution were offered further treatment and follow up as described above.
Results
From 2004 to 2013, 58 patients were treated using a KTP laser, delivered with a 1 or 2 mm Dermastat handpiece. The age range of patients was 2–86 years (mean of 32 years). Twenty-seven patients were under the age of 18 years. All patients aged 12 years or under, with the exception of one 10-year-old, underwent general anaesthesia. All other patients, with the exception of two 16-year-olds, underwent local anaesthesia. Thirty patients had prominent blood vessels in Little's area; the remainder had obvious, distinct bleeding points. Thirty-one patients had undergone previous treatment with silver nitrate cautery. Three patients therefore met both inclusion criteria (Figure 3). Thirty-eight patients had treatment to the left Little's area, and 19 to the right. One patient had treatment to both sides (in a single procedure) (Figure 4). The mean energy used was 26 J (range, 4–111 J).

Fig. 3 Distribution of the 58 patients treated using a potassium titanyl phosphate laser Dermastat from 2004 to 2013, split by inclusion criteria. AgNO3 = silver nitrate
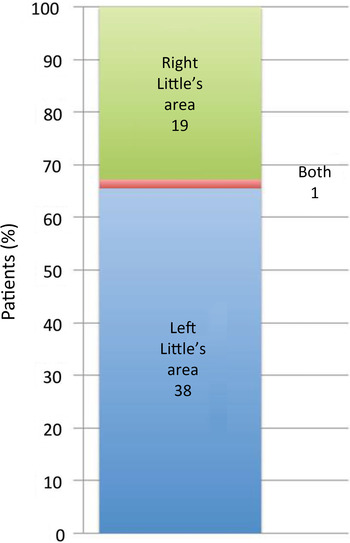
Fig. 4 Distribution of the 58 patients treated using a potassium titanyl phosphate laser Dermastat from 2004 to 2013, split according to side of treatment.
Fifty of the 58 patients (86 per cent) attended the follow-up appointment at 2 months (Figure 5). It is assumed that the 14 per cent of patients who did not attend the two-month follow-up appointment chose not to attend as they had not suffered any further epistaxis episodes (although this metric has not been included in our analysis and discussion). Thirty-seven of the 50 patients who did attend (74 per cent) reported complete resolution of symptoms (our main outcome measure).

Fig. 5 Summary of follow-up results, for patients who attended two-month follow up.
Of the 13 patients (26 per cent) who did not report complete resolution at 2 months, all reported a significant improvement in the frequency and intensity of bleeding. Seven of the 13 patients reported complete resolution at subsequent follow up (which took place at up to 6 months after treatment). Of these, two required no further treatment at all and five required a single further treatment with silver nitrate cautery to achieve complete resolution of symptoms. This resulted in a total of 78 per cent of patients reporting total resolution of the epistaxis, without any further intervention, at up to six months' follow up.
The remaining six patients who did not report resolution of symptoms at six months were offered further laser treatment and/or silver nitrate cautery at a later date. No complications were observed.
Discussion
Our results demonstrate that when a prominent vessel or bleeding point can be clearly identified in Little's area, and/or when previous treatment with silver nitrate cautery has failed, KTP laser delivered with a Dermastat handpiece gives good short- to medium-term results. It is well known that KTP laser has good haemostatic properties and is well absorbed by haemoglobin,Reference Clark, Cameron, Moseley, Ferguson and Ibbotson 15 , Reference Gossner, May, Stolte, Seitz, Hahn and Ell 16 and that the collateral damage caused is minimal compared to monopolar or bipolar diathermy and Nd:YAG laser.Reference Radosevich 17
Little's area, or Kiesselbach's plexus, is the commonest site of recurrent epistaxis.Reference Schlosser 2 , Reference Burton and Doree 4 The diameter of blood vessels in this area can vary from 0.8 to 2.1 mm. Pathological changes in these vessels (e.g. dissecting aneurysm, calcification, angiomas, loss of muscular tissue), particularly in the elderly, and weakening of the vessels as a result of inflammation, trauma and ischaemia, may act as predisposing factors to recurrent anterior epistaxis.Reference Schlosser 2 , Reference Pope and Hobbs 5 , Reference Chiu and Dunn 6
Silver nitrate cautery, with or without antiseptic cream (Naseptin) application, is the most common routine treatment for recurrent anterior epistaxis. Whilst the short-term effectiveness is generally reported at around 50–90 per cent, the medium- and long-term results are considered to be poor.Reference Schlosser 2 , Reference Benninger and Marple 3 , Reference Pope and Hobbs 5 , Reference Calder, Kang, Fraser, Kunanandam, Montgomery and Kubba 8 – Reference Robertson and Kubba 10 , Reference Ruddy, Proops, Pearman and Ruddy 12 The KTP laser Dermastat, in this case series, has proven to be more effective in the short- to medium-term than silver nitrate cautery.
KTP laser sources are already widely available in many centres, given their use in other areas of ENT practice and by other medical specialties. A single-use laser fibre, commonly used for laser delivery in other ENT procedures (such as vocal fold surgeryReference Yan, Olszewski, Hoffman, Zhuang, Ford and Dailey 18 ), costs between £120 and £150 (plus value added tax). A reusable Dermastat handpiece costs in the region of £2000 (plus value added tax) (as a one-off purchase), and therefore demonstrates a significant financial saving compared to disposable fibres. Whilst the handpieces themselves do not need to be autoclaved (the antiseptic wipes that are used to clean nasendoscopes are sufficient), the focal applicator tips do. The cost of this, however, is minimal.
Currently, the financial cost of using KTP technology with a single-use laser fibre does not justify its use as a first-line treatment for all patients with recurrent anterior epistaxis. However, our study demonstrates that the expense of the reusable KTP Dermastat system could be justified when used as either a first-line or alternative treatment, either in patients with prominent vessels around Little's area, and/or those for whom silver nitrate cautery fails. All our patients were treated as a day case in an operating theatre because of local laser safety protocols. However, the technique could easily be practised in a clinic or office environment in adult patients, if the correct equipment and a laser-safe environment are available.
-
• Recurrent anterior epistaxis forms a large part of out-patient ENT caseload
-
• The current most common treatments (silver nitrate cautery and/or antiseptic ointments) are lacking in efficacy
-
• Potassium titanyl phosphate laser, delivered by single-use laser fibre, is used in hereditary haemorrhagic telangiectasia epistaxis treatment and vocal fold surgery
-
• The reusable, clinic-safe Dermastat system is used by dermatologists for treating facial vascular lesions
-
• KTP laser Dermastat photocoagulation is a safe, effective, reliable treatment for recurrent anterior epistaxis in short- to medium-term
-
• It is cost-effective; the handpiece and applicator tip can be sterilised and reused
The Dermastat system is not currently used in ENT practice. In our opinion, KTP laser Dermastat photocoagulation is an economical, safe, reliable and effective treatment for recurrent anterior epistaxis. Although the short- to medium-term efficacy has been demonstrated in our small study, a further study with a larger series of patients is necessary to accurately assess the medium- to long-term efficacy of this treatment.
Acknowledgements
The authors would like to acknowledge and thank Dr Sarita Jain (dermatologist) for her contribution to the translation of the KTP Dermastat technique, from her dermatology practice to our ENT practice. Her expertise and advice was invaluable.







