Case report
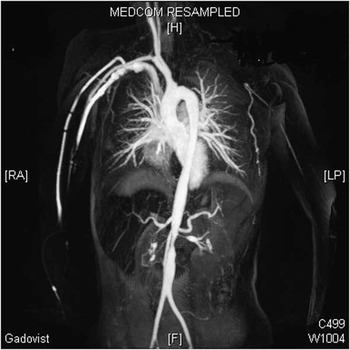
We report about a 12-year-old girl who was referred to Paediatric Cardiology with increasing exercise intolerance and massive arterial hypertension of the upper extremities. The systolic difference between the right and left arm was 120 mmHg. The initial suspicion was coarctation of the aortic isthmus, which was ruled out by echocardiography. The echocardiographic findings were a significant concentric hypertrophy of the left ventricle, a coarctation of the aorta abdominalis inferior of the origin of the renal arteries, a severe stenosis of the renal arteries, and a truncus coeliacus stenosis. An magnetic resonance angiography of the aorta was performed, where an additional occlusion of the proximal arteria carotis communis sinistra, arteria vertebralis, and arteria subclavia sinistra was shown (Fig 1). The laboratory test for C-reactive protein (7.46 mg/dl) and the erythrocyte sedimentation rate (120 mm/hour) were increased. Neutrophilia was also detected and anti-neutrophile cytoplasmatic antibodies were negative.

Figure 1 Magnetic resonance angiography of the aorta with stenosis of the aorta abdominalis, truncus coelicus, both the renal arteries, and occlusion of the proximal arteria carotis communis, arteria vertebralis, and arteria subclavia sinistra. (LP=linearly polarized; RA=rotational angiography).
To evaluate the cerebral perfusion with the total occlusion of the arteria carotis communis sinistra, we performed a cerebral angio-MRI that shows a normal perfusion over collaterals. There were no neurological symptoms or electrocardiogram abnormalities.
With the above results, the diagnosis of Takayasu arteritis was made. An immunosuppressive therapy with prednisolone, followed by methotrexate, as well as a thrombocyte aggregation inhibition with acetyl salicylic acid was initiated.
Treatment of persistent excessive arterial hypertension with systolic pressure above 200 mmHg and diastolic pressure above 100 mmHg was started with a combination of a β-blocker and a calcium antagonist. A low dose of an angiotensin-converting enzyme inhibitor was added owing to persistent high blood pressure and showed a good effect in lowering the blood pressure, but could not be further increased because of a rise in retention parameters.
A transcutaneous balloon angioplasty of the renal arteries with a paclitaxel-eluting balloon was performed owing to persistent arterial hypertension and repolarisation disturbances in the electrocardiogram (Figs 2 and 3).

Figure 2 Angiography with contrast of the both renal arteries before balloon angioplasty with a drug-eluting balloon (paclitaxel).

Figure 3 Angiography with contrast of the both renal arteries (arrows) directly after balloon angioplasty with a drug-eluting balloon (paclitaxel; SeQuent®, B Braun Melsungen AG).
The arteria femoralis dextra was accessed with a 6 F Terumo sheat. Then the angiography was performed with a 4 F pigtail catheter. After placement of a BMW Universal® guidewire (Abbott vascular®) in the arteria renalis sinistra, the pre-dilatation was performed using by a 3×15 mm drug-eluting (paclitaxel) balloon. (SeQuent®, B Braun Melsungen AG, Melsungen, Germany). This was followed by approximately dilating the longer and high-grade stenosis of the arteria renalis dextra with a 3×15 mm then with a 3.5×15 mm drug-eluting (paclitaxel) SeQuent® balloon. In both the arteries, the balloon was inflated for about 1 minute.
Afterwards, a successful elimination of the renal artery stenosis was achieved, and angiotensin-converting enzyme inhibitor (Lisinopril) was increased without any increase in retention parameters. After the procedures and the increase in medication, the systolic arterial pressure was reduced to about 130 mmHg.
There was no intervention concerning the other vessel stenosis; instead, we continued the immunosuppressive therapy. The treatment was monitored by regular duplex sonography.
We performed a catheter with angiography of the renal arteries after 3 months of treatment (Fig 4). Neither did we find restenosis nor regression of stenosis. The blood pressure stayed in the upper normal limits without further change in medication.

Figure 4 Angiography with contrast of both the renal arteries (arrows) 3 months after balloon angioplasty with a drug-eluting balloon (paclitaxel; SeQuent®, B Braun Melsungen AG).
Discussion
Takayasu arteritis is a rare granulomatous inflammatory disease of the large arteries in childhood with unknown incidence. Differential diagnosis includes fibro muscular dysplasia and secondary vasculitis in the context of systemic diseases – systemic lupus erythematosus and sarcoidosis. The cumulative incidence in all age groups is 2.6/1,000,000.Reference Brunner, Feldman and Tyrrell 1 The clinical appearance is variable. Main symptoms are arterial hypertension, headaches, abdominal and muscle pain, fatigue, weight loss, fever, and shortness of breath.Reference Stanley, Roebuck and Barboza 2 , Reference Aypar, Celebi-Tayfur and Keser 3 The diagnosis of Takayasu arteritis is made by the final EULAR/PRINTO/PRES c-TA criteria 2010.Reference Ozen, Pistorio and Lusan 4
Takayasu arteritis has a biphasic course. The symptoms of the acute early phase are unspecific. Diagnostic imaging show elongated stenosis (53%), occlusions (21%), and aneurysms (10%).Reference Creager 5
In the chronic phase, the aorta and its main branches of the neck, lung, and abdomen are included. Mainly affected are the arteria subclavia, arteria carotis communis, arteria vertebralis, arteria mesenteriales, arteria renalis, and more rarely, arteria femoralis and coronary arteries.
The therapy should be started as early as possible to avoid irreversible vessel disease and end-organ injuries. The therapy consists of an immunosuppressive medication, platelet inhibition with acetylsalicylic acid (3 mg/kg/day, per month), as well as a symptomatic antihypertensive therapy – medication and intervention.Reference Ramirez, Rivera and Reyes 6
Glucocorticoids (prednisolone 2 mg/kg/day) are the first-line medication in an active disease. In 60% of patients, a remission could be achieved with a monotherapy.Reference Brunner, Feldman and Tyrrell 1 After glucocorticoids, other immunosuppressants, such as methotrexate, azathioprine, and infliximab, are used in therapy-resistant cases.
The prognosis of Takayasu arteritis is dependent on the involvement of the vessels and the severity of the arterial hypertension.Reference Brunner, Feldman and Tyrrell 1 In childhood, the mortality rate of 10–30% has been reported on follow-up.Reference Kothari 7
In our case, the usually associated arterial hypertension was treated first with a combination of a β-blocker, bisoprolol, and a calcium-antagonist, amlodipine. An aldosterone antagonist, spironolactone, was added without any impact. Angiotensin-converting enzyme inhibitors are contraindicated with renal stenosis; however, under monitoring of renal retention parameters, a angiotensin-converting enzyme inhibitor (Lisinopril) was carefully added to the regime and showed a considerably antihypertensive effect. After the initial treatment the retention parameters increased, a further increase was not considered. When the normalisation of the inflammatory parameters under immunosuppressive therapy was observed, an intraluminal angioplasty of the renal arteries with a paclitaxel-eluting balloon was performed.Reference Kang, Han, Oh, Ahn and Shin 8
Paclitaxel belongs to the taxane group, which inhibits the cell separation in mitosis. Therefore, a local anti-inflammatory effect with resulting reduction in neointimal hyperplasia is promoted.
The complication rate of endovascular stenting compared with balloon angioplasty in the adult population is higher. Major complications of endovascular stenting are in-stent restenosis or stent thrombosis.Reference Agarwal, Vats, Raval, Yevzlin, Chan and Gimelli 9 Comparable studies in children are missing so far. In this case, balloon angioplasty was primarily performed. We kept open the option of stenting by restenosis or clinical worsening.
Angioplasty and stenting show initially good results, but the rate of restenosis is high. Several reports showed a rate of restenosis of 8–20% within a follow-up of 14–120 months.Reference Agarwal, Vats, Raval, Yevzlin, Chan and Gimelli 9 , Reference Park, Do and Park 10 Significant differences between children and adults are not obvious.
Park et al compared the long-term results after angioplasty versus stent placement in a small study. He showed a good technical success rate of both procedures. The restenosis rate was 8% in angioplasty versus 66% after stent placement by a follow-up of in the middle 20 months. He deduced that stent placement should be preserved for unsuccessful angioplasy.Reference Park, Do and Park 10
Acknowledgement
None.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None