Introduction
Providing high-quality cardiopulmonary resuscitation (CPR) can improve survival following cardiac arrest.Reference Kleinman, Brennan and Goldberger1 Conditions for high-quality CPR include ensuring chest compressions of adequate rate and depth, allowing full chest recoil between compressions, minimizing interruptions in chest compressions, and avoiding excessive ventilation.Reference Kleinman, Brennan and Goldberger1 Therefore, the recent CPR guidelines recommend the use of CPR prompt/feedback devices during CPR training because it can improve the quality of CPR.Reference Greif, Lockey and Conaghan2-Reference Spooner, Fallaha, Kocierz, Smith, Smith and Perkins6
Among the conditions for high-quality CPR, instructors of the present study’s medical school had tended to focus on enhancing chest compression depths in 2017 because the chest compression depth was significantly low in the CPR skill test of 2016. As a result of emphasizing chest compression depth during CPR training, the chest compression depth increased significantly in the CPR skill test of 2017. However, the ratio of full chest recoil decreased simultaneously.
To increase both the chest compression depth and ratio of full chest recoil, the present study’s medical school decided to introduce a visual feedback device during CPR training in 2018. This study investigated the effects of introducing a visual feedback device during CPR training by analyzing the results of CPR skill tests before and after introducing a visual feedback device during CPR training.
Materials and Methods
Study Design
The results of CPR skill tests from 2016 through 2018 were retrospectively reviewed. The study design was approved by the institutional review board (IRB) of the study site (Approval No. 1809-008-16202). The need for informed consent was waived by the IRB.
CPR Training and Skill Test
The present study’s medical school provides CPR training sessions and CPR skill tests to fourth-year medical students annually between March and April. The CPR training comprises two parts: a one-hour lecture and one hour of practice with a manikin. Because a basic science and theoretical lecture for CPR is conducted in the first semester for third-year students, only practical information for the CPR skill test is provided during the lecture for fourth-year medical students (eg, introduction of the scenario for the simulated adult cardiac arrest in the CPR skill test, instructions for using a manikin, and compositions of score on the CPR skill test). During the training sessions, a single instructor teaches eight students every hour using five manikins (four Little Annes [Laerdal Medical; Stavanger, Norway] and one Resusci Anne QCPR [Laerdal Medical]). The interval between the CPR training and skill test is seven days.
In 2017, the strategy of emphasizing chest compression depth was implemented during the CPR training to increase the chest compression depth. In 2018, a visual feedback device of Little Anne QCPR with SkillGuide (Laerdal Medical) was introduced during the CPR training to increase both the chest compression depth and ratio of full chest recoil.
The CPR skill test is comprised of five minutes of single-rescuer CPR from checking scene safety to completing five cycles of CPR (each cycle includes 30 compressions and two ventilations). The following scenario is provided just before the test: “A 60-year-old man suddenly collapses just before you when you are walking on the street. You should act out the role of first responder starting with checking the scene safety.” An instructor who oversaw grading ceased the CPR after five cycles of CPR (150 chest compressions and 10 ventilations) during the skill test. The mouth-to-mouth ventilation method was performed using a face shield.
A Resusci Anne QCPR was used as a simulated patient with cardiac arrest. The score of the skill test was calculated using a checklist composed of 13 key components. Among them, six components (ratio of correct location of chest compression, ratio of adequate chest compression rate, average chest compression depth, ratio of full chest recoil, number of ventilations and average ventilation volume, and chest compression fraction) were rated using the data recorded in the SimPad SkillReporter (Laerdal Medical). Any of the feedback signals from the device or instructor were not provided during the CPR skill test.
Among the data from the SimPad SkillReporter, the number of total chest compressions, ratio of correct location of chest compression, average chest compression depth, ratio of adequate chest compression depth, average chest compression rate, ratio of full chest recoil, number of total ventilations, and average ventilation volume were analyzed.
Statistical Analysis
All statistical analyses were performed using IBM SPSS Statistics, version 25.0 (IBM Corp.; Armonk, New York USA). Continuous variables were presented as mean (standard deviation) or median (interquartile range; 25th percentile-75th percentile) according to the normality of the data distribution, whereas categorical variables were expressed as frequencies and percentages. The normality of the data distribution was analyzed using the Shapiro-Wilk test or the Kolmogorov-Smirnov test. For normally distributed data, one-way analysis of variance was used for the comparison of data among the years; otherwise, the Kruskal-Wallis test was used. Multiple comparisons were conducted using Tukey’s multiple comparison test or the Mann-Whitney U test. A P value of less than .05 was considered statistically significant.
Results
In total, 159 medical students completed the CPR skill tests (74 in 2016, 37 in 2017, and 48 in 2018). The number of male students were 52/74 (70%) in 2016, 24/37 (65%) in 2017, and 31/48 (65%) in 2018. Average chest compression depth, the number of total ventilations, and average ventilation volume increased significantly after emphasizing chest compression depth during the CPR training in 2017 (Table 1). However, the ratio of full chest recoil decreased significantly in 2017. The ratio of full chest recoil increased significantly after introducing a visual feedback device in 2018. However, the number of total chest compressions, average chest compression depth, the number of total ventilations, and average ventilation volume decreased significantly in 2018.
Table 1. Changes in the Performances of Cardiopulmonary Resuscitation since 2016
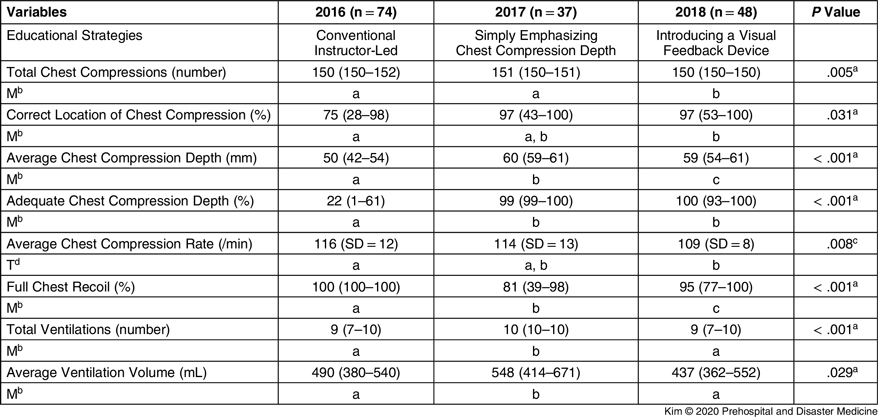
Note: Variables were presented as mean (standard deviation) or median (interquartile range: 25th percentile-75th percentile).
a Statistical significances were analyzed using the Kruskal-Wallis test.
b The same letters indicate non-significant differences between variables based on the Mann-Whitney U test.
c Statistical significances were tested using one-way analysis of variance.
d The same letters indicate a non-significant difference between variables based on Tukey’s multiple comparison test.
The students who did not achieve 50 mm of average chest compression depth decreased significantly since 2016 (47% in 2016, 5% in 2017, and 6% in 2018; P < .001; Figure 1). However, the students who did not achieve 80% of the ratio of full chest recoil remained significantly higher than in 2016 (1% in 2016, 49% in 2017, and 27% in 2018; P < .001). The students who did not achieve 80% of the ratio of correct location of chest compression tended to decrease since 2016 (53% in 2016, 43% in 2017, and 35% in 2018; P = .059).
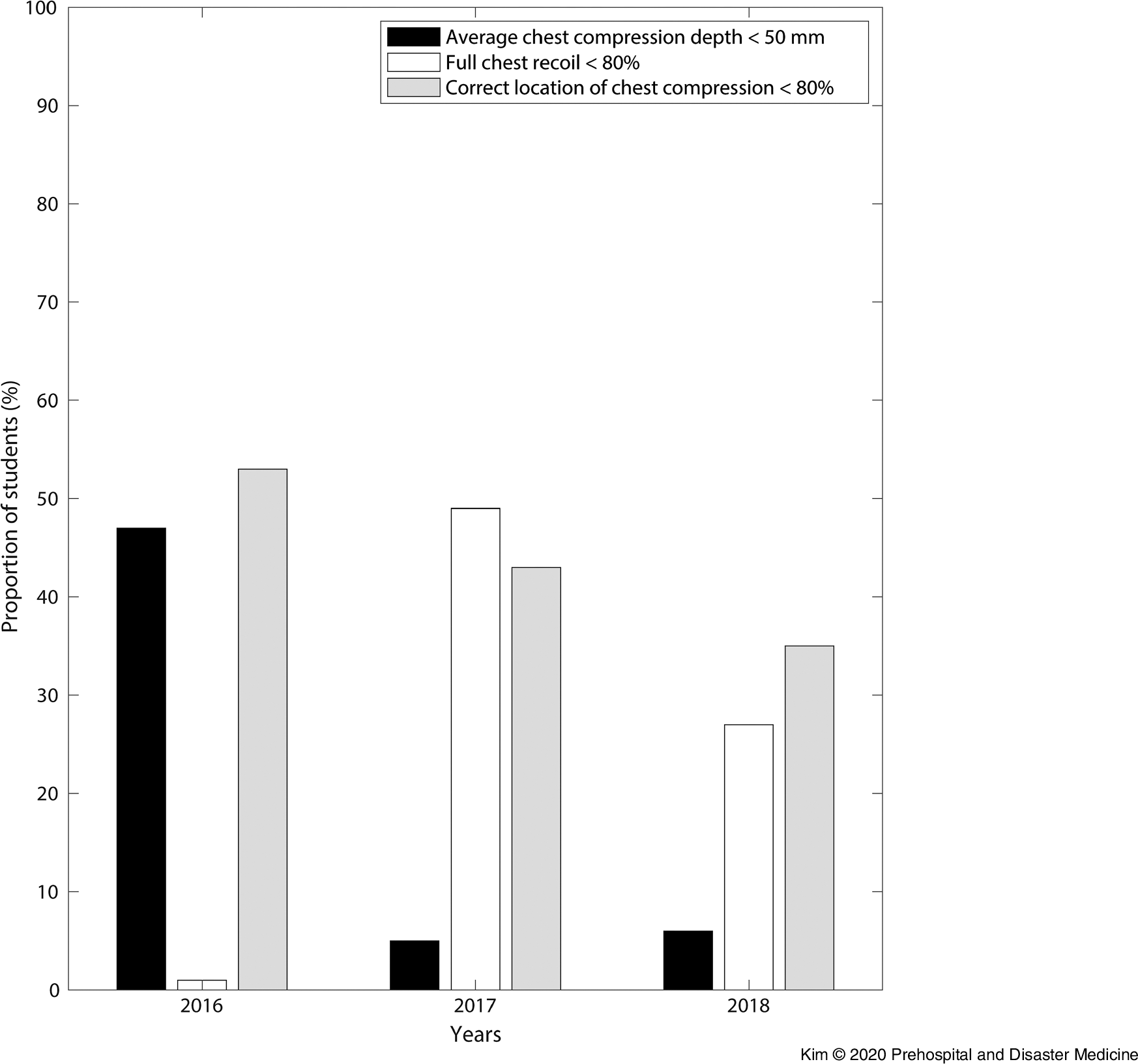
Figure 1. Qualities of the Cardiopulmonary Resuscitation among the Medical Students since 2016.
Discussion
A previous study comparing the results of skill tests after CPR training with or without using a visual feedback device showed that both the chest compression depth and ratio of full chest recoil were higher in the group that completed CPR training using a visual feedback device.Reference Baldi, Cornara and Contri7 Therefore, it was expected that introducing a visual feedback device to the CPR training could improve the chest compression depth and ratio of full chest recoil simultaneously. The ratio of full chest recoil improved after introducing a visual feedback device, as expected. Although the chest compression depth decreased significantly after introducing a visual feedback device, the interquartile range of the chest compression depth was adequate considering the recommended chest compression depth in the CPR guidelines (at least 50 mm). In addition, the adequacies of the chest compression depth were not different before and after introducing a visual feedback device. Therefore, introducing a visual feedback device during CPR training resulted in increasing the ratio of full chest recoil while maintaining the adequacy of chest compression depth.
The problem is that 27% of the students still did not achieve 80% of the ratio of full chest recoil. An additional educational strategy may be needed to achieve the conditions of high-quality CPR completely. Previous studies showed additional advantages of team coaching or just-in-time training (watching a five-minute standardized CPR training video), in addition to use of a visual feedback device compared with a non-feedback group or visual feedback-only group.Reference Cheng, Brown and Duff4,Reference Austin, Spalding and Landa8
As well-described previously, chest compression depth and full chest recoil shows a trade-off relationship.Reference Contri, Cornara and Somaschini9,Reference Oh10 Therefore, achievement of both targets (adequate chest compression depth and full chest recoil) simultaneously is a difficult task for CPR instructors. Various strategies or feedback methods had been tried previously.Reference Spooner, Fallaha, Kocierz, Smith, Smith and Perkins6,Reference Baldi, Cornara and Contri7,Reference Yeung, Meeks, Edelson, Gao, Soar and Perkins11-Reference Park, Hong, Shin, Lee and Hwang14 Each strategies or feedback showed its own advantages and limitations (Table 2). Using a visual feedback device during CPR training seems to be the most effective method for increasing the quality of CPR among various strategies, except for real-time feedback on chest compression depth or rate during CPR.Reference Skorning, Beckers and Brokmann15,Reference Wutzler, Bannehr and von Ulmenstein16 However, the present study’s results showed the advantages and limitations of introducing a visual feedback device during CPR training. The instructors of CPR should understand the mechanisms of CPR and be aware of the advantages and limitations of using a visual feedback device during CPR training.
Table 2. The Effects of Various Feedback Strategies for Cardiopulmonary Resuscitation Training

Note: The superscript number indicates the reference number.
a The results of the present study.
Limitations
The present study had some limitations. First, this study was not a prospective trial. The differences in the qualities of CPR might have originated not from the different educational strategies, but from the differences in the skill performance between the students of different years. Second, the study population was limited to medical students. Therefore, the applicability of the study results is limited. Third, the anthropometric data of the students could not be available because this study reviewed the results of CPR skill tests retrospectively. Therefore, the present study could not evaluate the characteristics of the students according to the years.
Conclusions
Introducing a visual feedback device during CPR training could increase the ratio of full chest recoil with maintaining the adequacy of chest compression depth compared to simply emphasizing the chest compression depth. However, 27% of the students still did not achieve 80% of the ratio of full chest recoil, even though they completed the CPR training using a visual feedback device. Another educational strategy should be considered to increase the qualities of CPR more completely.
Conflicts of interest/funding
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The authors received no financial support for the research, authorship, and/or publication of this article.





