Hypoplastic left heart syndrome is a spectrum of abnormalities characterised by underdevelopment of the left ventricular outflow tract with concomitant and variable degrees of hypoplasia of other left-sided heart structures.Reference May1 Hypoplastic left heart syndrome affects one in 5000 live births.Reference Dean and Hillman2 The Fontan procedure, initially described in 1971 by Fontan and Baudet as a surgical treatment for tricuspid atresia, was adopted in the 1980s as the final stage in the surgical palliation of hypoplastic left heart syndrome and other CHDs with single ventricle anatomy.Reference Dean and Hillman2 Since then, the Fontan procedure has been modified to improve post-operative morbidity and mortality.Reference Cava and Bevandic3,Reference Sunstrom, Muralidaran and Gerrah4 The modified Fontan procedure consists of surgically placing an external tubular conduit or internal lateral tunnel to passively redirect systemic venous return via the inferior caval vein to the pulmonary arteries.Reference May1 The passive redirection of the venous system leaves the single ventricle responsible only for supplying blood to the body.Reference May1 While the 10-year survival rate after extracardiac conduit and lateral tunnel Fontan repair is excellent at 97%, significant morbidity continues to be an issue and can considerably affect hospital length of stay.Reference Cava and Bevandic3,Reference d’Udekem, Iyengar and Galati5
Over the past several decades, standardisation has become an increasingly common method of developing and implementing specific processes and criteria for improving consistency, quality and safety in healthcare. The evidence-based practice movement promotes standardisation in healthcare through the use of clinical practice guidelines, pathways, protocols and checklists designed to improve quality and safety by reducing practice variations.Reference Mannion and Exworthy6 The concept of standardising care delivery for the post-operative cardiac patient emerged at the same time as other surgical services in the mid-1990s, with paediatric cardiology at the forefront of this movement.Reference Uzark, Frederick and Lamberti7,Reference Allen and Davis8 For the Fontan patient population, three published post-operative clinical protocols have demonstrated lower length of stay than the national average.Reference Cava and Bevandic3,Reference Sunstrom, Muralidaran and Gerrah4,Reference Pike and Okuhara9 With the Wisconsin protocol, mean hospital stay was reduced from 18 to 9 days.Reference Cava and Bevandic3 The PORTLAND protocol improved length of stay from 13 to 8 days.Reference Sunstrom, Muralidaran and Gerrah4 Pike et al. used a modified Wisconsin Fontan protocol, reducing median hospital length of stay from 8 to 6 days.Reference Pike and Okuhara9
At the study institution, there was no standard of care for the post-operative Fontan patient, and the institutional length of stay for this patient population has historically been longer than the national benchmark, indicating an area of potential improvement.Reference Dean and Hillman2 Without a defined and clear standard approach to care, treatment could be variable, especially when complications arose. These patients, in particular, are at a higher risk for developing complications related to continued pleural drainage, thus prolonging their length of stay.Reference Cava and Bevandic3,Reference Pike and Okuhara9,Reference Gupta, Daggett and Behera10 The purpose of the quality improvement project was to determine if implementing an evidence-based clinical pathway for post-operative management of the Fontan patient at our institution would standardise care and decrease length of stay.
Materials and methods
The project was classified as an evidence-based quality improvement study and categorised as non-human subjects research by the institutional review board of the study institution, Children’s Mercy Hospital in Kansas City, Missouri. Individual informed consent was waived.Reference O’Mathuna, Melnyk and Fineout-Overholt11
Study participants included all patients who underwent the extracardiac Fontan procedure and were discharged to home. Fontan revisions, those requiring an additional procedure (permanent pacemaker implantation), patients who were placed on palliative care, listed for transplant post-Fontan procedure, or who died prior to initial hospital discharge were excluded.
The clinical pathway was developed using the three published studies of Fontan clinical pathways as a guide, incorporating key components from each.Reference Cava and Bevandic3,Reference Sunstrom, Muralidaran and Gerrah4,Reference Pike and Okuhara9 Components of the clinical pathway implemented with this project for the post-operative management of the Fontan patient included (1) supplemental oxygen via nasal cannula until chest tubes are removed, (2) fluid restriction to 80% of daily maintenance fluids to be liberalised prior to discharge, a free water restriction, and a low-fat diet to be followed for 2 weeks after chest tube removal or 6 weeks if chylous drainage, (3) aggressive and standardised diuretic therapy while inpatient and a recommended minimal diuretic regimen for discharge and (4) central access via placement of a peripherally inserted central catheter line in interventional radiology 24–72 hours post-operatively for patient ease and comfort related to need for frequent laboratory draws and medication administration (see Fig 1 for Interventional Flow Diagram).
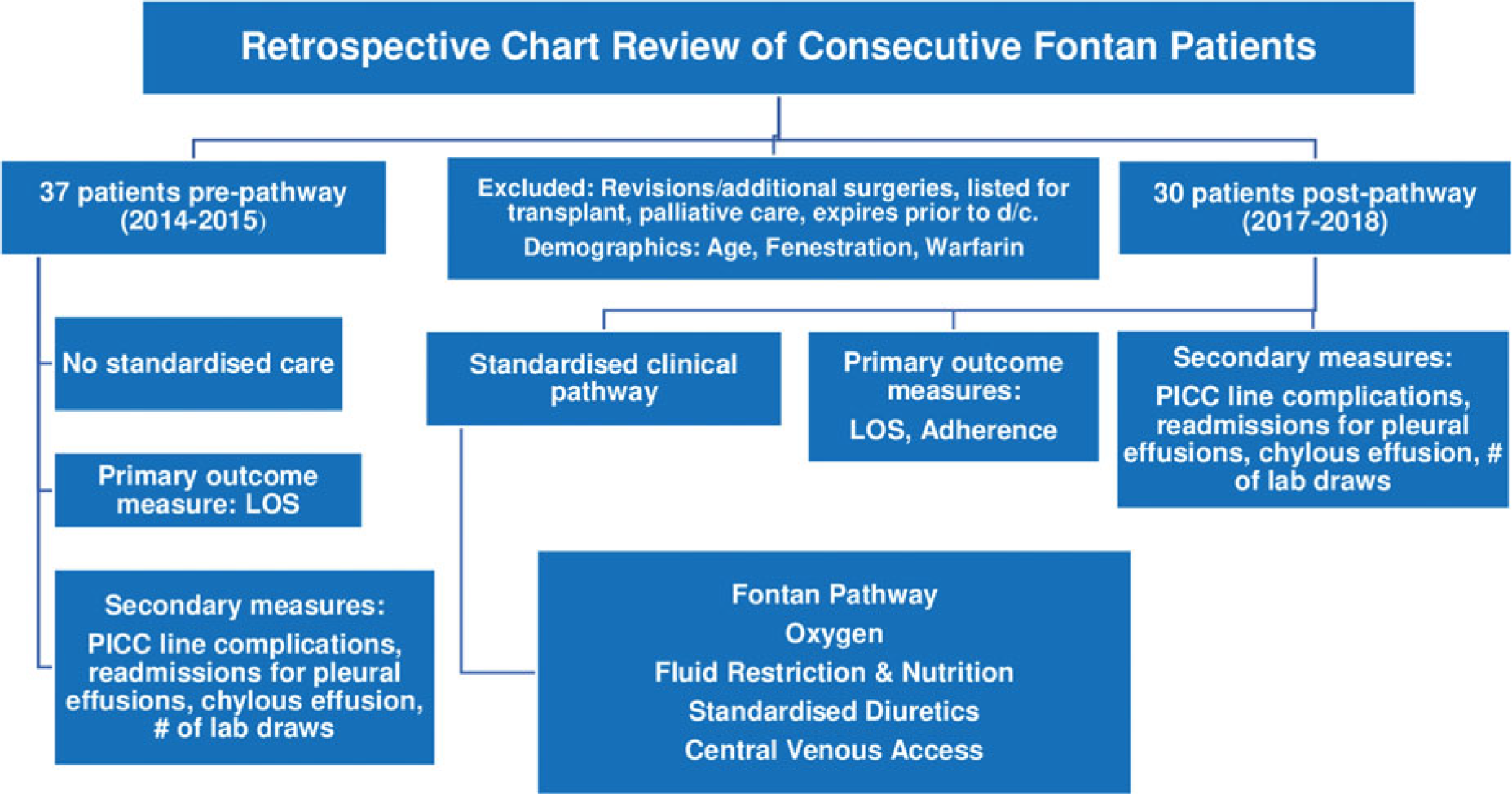
Figure 1. Interventional Flow Diagram.
In 2016, Plan-Do-Study-Act cycles were completed with three patients for each component: supplemental oxygen, fluid restriction and low-fat diet, aggressive and standardised diuretics, and a peripherally inserted central catheter line. Implementation in 2017 involved educating providers and nursing staff regarding the components of the pathway and tracking adherence. A student investigator led educational sessions with the paediatric ICU and inpatient unit nurses at quarterly unit educational updates. A copy of the clinical pathway and a bedside checklist was provided to each unit. The student investigator sent electronic communication to the inpatient providers in the paediatric ICU and on the floor as each patient underwent the Fontan. The clinical pathway interventions and a bedside checklist were included as a reminder and resource (see Figs 2 and 3 Educational Materials). An order set within the electronic medical record was also developed to aid in ordering each component in the pathway. Inpatient advance practice nurses championed the implementation of the clinical pathway by encouraging its use, tracking adherence and serving as an expert resource. They were also integral in sustaining the pathway from 2018 to 2019.

Figure 2. Educational Materials: Bedside Checklist.
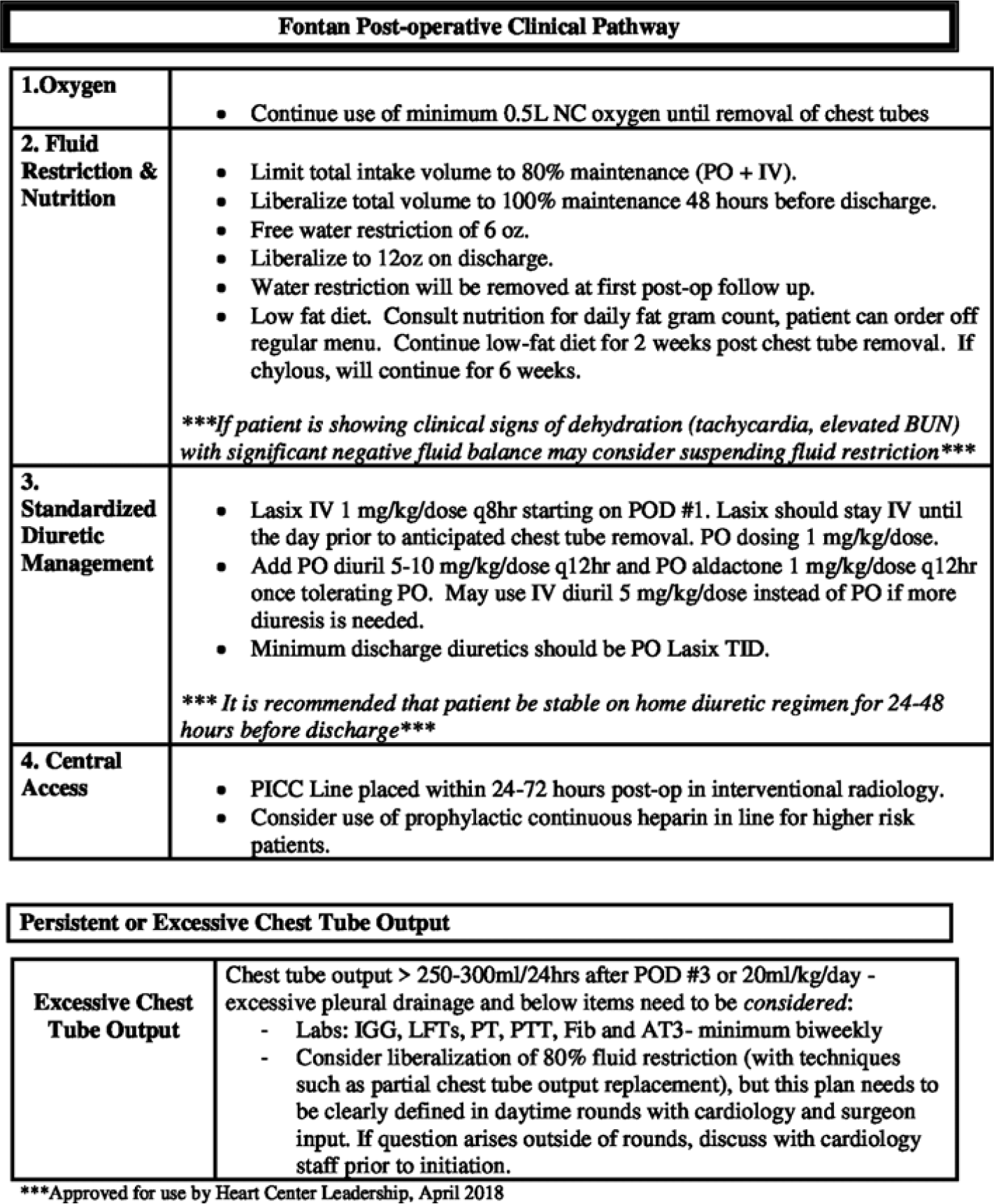
Figure 3. Educational Materials: Fontan Post-operative Clinical Pathway.
Study variables
Primary outcome measures included the percent adherence to each component of the pathway and length of stay in number of days. Secondary outcomes measures included incidence of chylous effusions, peripherally inserted central catheter line infections and/or thrombi (morbidity), number of patients readmitted within the first 30 days of discharge for treatment of reoccurrence of pleural effusions, and number of laboratory draws per patient. In addition to collecting data with regard to the primary and secondary outcomes, the following patient demographic information was also obtained: age, fenestration and use of warfarin for anticoagulation therapy (Fig 1).
Statistics
The Statistical Package for the Social Sciences was used to perform the data analysis. Descriptive statistics were used for both primary and secondary outcomes. A t-test was used to compare the groups on age, and Wilcoxon Rank Sum tests were used for length of stay and total laboratory draws as those variables were fairly skewed. Chi-square and Fisher’s Exact tests were used for comparing the groups on the categorical variables of readmissions, fenestration, use of warfarin, presence of chylous effusion, and peripheral inserted central catheter line complications of thrombus and/or infection. Percent adherence was reported descriptively as it is only a post-pathway measure.
Results
Pre-pathway data were collected on all 44 Fontan patients from 2014 and 2015, and post-pathway data were collected on all 36 Fontan patients from 2017 and 2018. The defined exclusion criteria were applied after all data were obtained.
Primary outcomes for the project were length of stay and percent adherence to the clinical pathway. The pathway had nearly 100% adherence as calculated by whether each patient followed each component of the pathway. Length of stay was significantly shorter post-pathway at 9 days versus pre-pathway of 12 days (p = 0.007) (Table 1).
Table 1. Statistical analysis results table and graphing of key findings

IQR = interquartile range; LOS = length of stay; PICC = peripherally inserted central catheter.
Secondary outcomes included incidence of chylous effusions, readmissions for pleural effusions, central line-associated thrombi and/or infections, and number of laboratory draws. Incidence of chylous effusions (3, 8.1% pre- versus 2, 6.7%; p = 1.00), readmissions (4, 10.8% pre- versus 5, 16.7%; p = 0.500) and number of laboratory draws were similar between the pre- and post-pathway cohorts (28 pre- and post-; p = 0.837). The number of Fontan patients who had a peripherally inserted central catheter line placed was significantly higher (13, 35.1% versus 22, 73.3%; p = 0.002), as this was one of the components of the pathway. However, line-associated complications were also greater (p = 0.006); this component of the pathway was suspended mid-way through the 2018 season.
No data were missing. Two patients post-pathway were ready for discharge from a post-operative standpoint but had longer stays related to the need for further social work evaluation and inpatient rehabilitation. Length of stay was therefore calculated from when patients met discharge criteria post-surgery. The number of laboratory draws for hospitalisation and any complications past that length of stay for these two patients were not included in the outcomes data calculations.
As for patient demographics, there was a statistically significant difference for age with mean age of 5.84 years versus 3.73 years (p < 0.001) of pre- versus post-pathway. The number of patients who had a fenestrated Fontan was similar (29.7% pre- versus 23.3% post-pathway; p = 0.557), but those who were started on warfarin for anticoagulation were statistically different with 32.4% pre- and 3.3% post- (p = 0.003) due to changes in surgeons and their anticoagulation preferences for warfarin versus aspirin for fenestrated Fontans.
Sustainability data were reviewed for all 21 patients who underwent the Fontan procedure in 2019. Adherence remained at 100% and length of stay at 9 days. Readmission rates also remained stable.
Discussion
Both of the primary outcomes or aims of the project were successfully met. Previously, care varied widely from attending provider to provider, particularly with regard to management of nutrition, fluids and diuretics in the post-operative Fontan patient. After we implemented the post-operative clinical pathway, care was successfully standardised. Additionally, a statistically significant decrease in length of stay without an increase in morbidity was evidenced by similar readmission rates and incidence of chylous effusions.Reference O’Brien12
When the project was initially started, the national benchmark for length of stay for post-operative Fontans was an average of 11 days, whereas the study institution’s average length of stay was 14 days for this patient population without applying the defined exclusion criteria.Reference Dean and Hillman2 From 2011 to 2014, the Society of Thoracic Surgeons tracked 4161 Fontan surgical outcomes and found the aggregate average length of stay to be 13.4 days.Reference Jacobs, Shahaian and Prager13 The implementation of the post-operative clinical pathway at the study institution resulted in a decrease in length of stay from 12 days to 9 days (with exclusion criteria applied; median length of stay reduced from 14 to 11 days for all comers), which exceeds the current national benchmark (2013–2016) of 13.6 days.Reference Jacobs, Shahaian and D’Agostino14This finding is similar to the other three paediatric institutions with published post-operative clinical protocols that also have lower length of stay than the national average.Reference Cava and Bevandic3,Reference Sunstrom, Muralidaran and Gerrah4,Reference Pike and Okuhara9
The intervention of implementing a post-operative clinical pathway for a specific subset of paediatric cardiac surgery patients was well supported by the organisational culture of the study institution, cardiology department, and provider and nursing staff in the ICU and the inpatient cardiology ward. The project hospital is a Lean institution and encourages evidence-based quality improvement projects by providing training and support to its employees. As one of the leading paediatric cardiac surgery programs in the United States, the Heart Center is always striving to meet or exceed the national benchmarks with regard to overall surgical outcomes. The providers and nursing staff recognised the Fontan patient population as uniquely challenging and likely to benefit from a standardised approach in care.
As anticipated, performing Plan-Do-Study-Act cycles prior to fully implementing the clinical pathway allowed us to identify and address potential barriers as well as promoted buy-in for the project from key stakeholders. Adherence during Plan-Do-Study-Act cycles was 100% for each component of the pathway except for fluid restriction, with only one out of three patients adhering to the 80% fluid restriction. More education was therefore provided to the physicians, advance practice nurses, and nurses regarding goal fluid status for each patient. It was also recommended that the decision to suspend and/or restart intravenous fluids be done only if there were clinical signs or symptoms of dehydration and with the approval of the attending or on-call cardiologist. Once these actions were fully implemented, adherence to the fluid restriction component improved greatly.
Limitations
A possible confounding factor for this project includes a change in the surgeons who were operating during the study period and subsequently a change in practice due to surgeon preference of using aspirin versus warfarin for anticoagulation on fenestrated Fontans. Achieving appropriate warfarin dosing for adequate anticoagulation can increase length of stay; therefore, a decrease in the use of warfarin post-pathway could contribute to the decrease in length of stay. There was a significant difference between the pre- and post-pathway cohorts with regard to age. Napolene and colleagues, however, found that age at the time of Fontan surgery is not a factor in post-operative outcomes.Reference Napolene, Oppido and Angeli15 The exclusion criteria used could introduce bias into the study; however, they were consistently applied to pre- and post-pathway patients. The tracking of adherence to each component of the intervention introduces bias as well, as adherence is a more subjective measure. Only the student investigator tracked adherence, thus limiting the variability in determining whether the pathway was followed or not.
Conclusions
Clinical pathways should be used for the post-operative management of certain patient populations, including the Fontan patient, as a means to standardise care and improve initial outcomes. The Fontan clinical pathway standardised care and significantly reduced length of stay during the post-operative pathway period. A similar clinical pathway could be implemented for post-operative Fontans at other paediatric hospitals with strong cardiac surgery programmes. Institutions that have project support from a leadership and system standpoint and that use advance practice nurses as the champions of pathway implementation and sustainability likely will be more successful in implementing this change in practice. If other paediatric institutions used evidence-based standardised pathways for post-operative Fontans, overall length of stay as tracked by the Society of Thoracic Surgeons, incidence of complications related to prolonged hospitalisation, and associated costs could be reduced for this complex patient population.
Acknowledgements
The student investigator would like thank Dr. Lisa Laddish, Ward Family Heart Center Advanced Practice Nurse inpatient manager and preceptor for doctoral practicum and clinical hours, Dr. Lyla Lindholm, doctoral of nursing practice faculty at University of Missouri-Kansas City, and Ashley Sherman, statistician at Children’s Mercy Hospital, for their support and guidance. We would also like to thank the Medical Writing Center at Children’s Mercy Kansas City for editing this manuscript.
Financial Support
The estimated cost of the project was $69,224 (Table 2). Financial support for the cost of the project was provided by the Heart Center at study institution given this was a practice change by a current employee with support from departmental and hospital leadership. This project received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Table 2. Project cost table

APRN = advanced practice registered nurse.
Conflicts of Interest
None.
Ethical Standards
Institutional review board approval was obtained to conduct this retrospective quality improvement study, and individual patient consent was waived.






