Event Identifiers:
a. Event Type: Flood
b. Event Onset Date: August 15, 2018
c. Location of Event: Kozhikode, India
d. Geographic Coordinates: 11.2588° N, 75.7804° E, Elevation 3.281’
e. Dates: August 15, 2018 to September 8, 2018
f. Response Type: Medical Relief
Introduction
In August 2018, India’s southern state of Kerala experienced its worst flooding in over a century.Reference Baynes1 Over a period of weeks, heavy rains, rising flood waters, and landslides left an estimated 483 dead and hundreds of thousands displaced.2,3 In response to the devastation, the National Health Mission (Ministry of Health and Family Welfare; New Delhi, India), the district administration, and the Active Network Group of Emergency Life Savers (ANGELS; Kozhikode, India) initiated Operation Navajeevan, a joint Private-Public Partnership (PPP) with health care facilities and nongovernmental organizations (NGOs) in the region to provide medical relief to flood victims. This report describes the relief efforts in Kozhikode, a coastal region of Kerala, where Operation Navajeevan was initiated.
The aim of this report is to describe the relief effort and the clinical profile of patients who presented to flood relief camps during the August 2018 floods in Kozhikode. As an especially flood-prone country, describing relief efforts and understanding the epidemiologic profile of patients will be important to improving future preparedness and response in India.
The Relief Effort
Medical teams consisting of a Chief Medical Officer (MO), a local health inspector, a team of physicians, volunteer Emergency Medical Care Technicians, as well as local volunteers were formed in each relief camp to ensure 24-hour medical services for flood victims. The district was divided into seven zones. High-level tertiary care centers, both public and private, were identified in each zone. Critically ill patients presenting to relief camps were transferred to the nearest higher-level facility in their zone. During this time, private hospitals agreed to provide free treatment to all patients presenting from the flood zone. A command center was established at the District Medical Office to supervise and coordinate logistics between camps. The MOs from each camp sent daily briefings to the command center detailing the number of patients, types of cases being seen, in addition to any logistical difficulties. Five mobile intensive care units (ICUs) and 40 ambulances under the supervision of the ANGELS were kept on standby throughout the district to respond to emergencies and provide additional surge capacity. A map of the relief camps can be found in Figure 1.
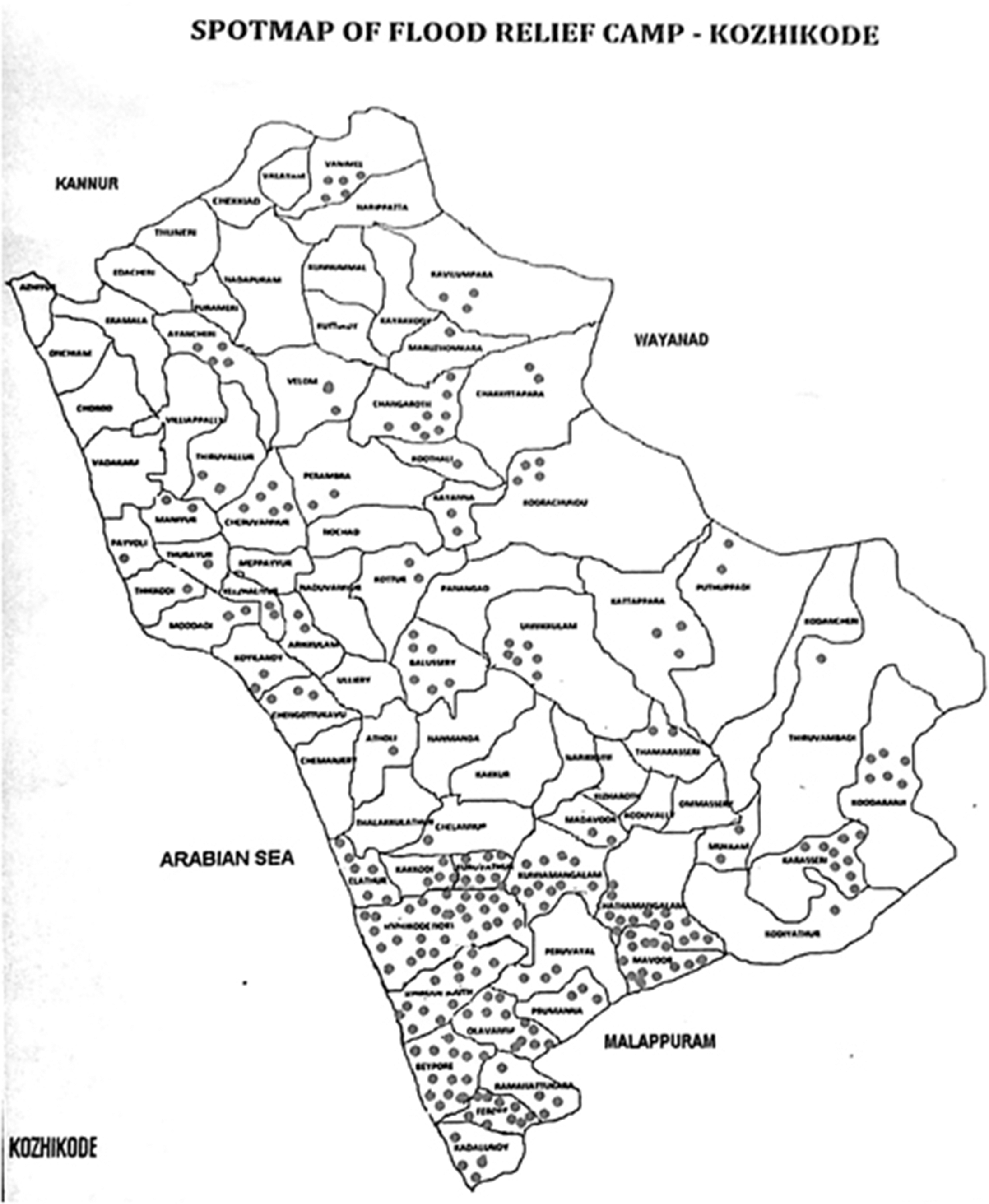
Figure 1. Spotmap of Flood Relief Camp – Kozhikode, India.
Along with providing direct medical care, camps partnered with local NGOs to provide public health education sessions which included training on personal hygiene, wound care, and clean water sources. Classes were also held on first aid and prevention for snake bites, control of vector-borne diseases, and avoidance of electrical injuries in flood affected areas.
During the sixth day of the relief effort, the first case of leptospirosis was confirmed in the camps. In anticipation of possible leptospirosis outbreak, doxycycline was made available in all relief camps at the outset of Operation Navajeevan. Daily meetings by camp MOs were held to track the spread of cases. Public education regarding sanitation was made available to prevent further spread of disease.
Sources
Data were collected from a centralized database at the command center in the District Medical Office as well as first-hand accounts from providers who participated in the relief effort.
Observations
From August 15, 2018 through September 8, 2018, 36,846 flood victims were seen at the 280 medical relief camps set up across Kozhikode. Patient demographics can be found in Table 1. By far, the most common cause for presentation to the relief camps was exacerbation of an on-going chronic medical condition (18,490; 50.2%). Other common presenting complaints included acute respiratory infection (7,451; 20.2%), traumatic injuries (3,736; 10.4%), and psychiatric illness (5,327; 14.5%). A breakdown of patient medical complaints can be found in Table 2. A total of 137 confirmed cases of leptospirosis were seen during Operation Navajeevan with seven deaths.
Table 1. Patient Demographics

Table 2. Medical Presentation

Analysis
Operation Navajeevan created a highly coordinated system to provide care for flood victims in Kozhikode. There were multiple organizational and structural components that made this system successful. This system utilized a hub and spoke model (HSM) to health care delivery in which patients are filtered from lower acuity peripheral health clinics to higher level tertiary care centers.Reference Elrod and Fortenberry4 The HSM is an established model for health care delivery and has been used in rural India for the provision of health care in the non-emergency setting; however, it has not been previously described for acute health care delivery in the disaster setting when regular health care infrastructure is not functioning.Reference Devarakonda5,Reference Wilson6 Operation Navajeevan included a central command center (hub) established at the District Medical Office to supervise and coordinate logistics between medical camps (spokes). Daily communications between the central command center and medical camps allowed for judicious use of resources and prevented duplication of services. The use of mobile ICUs on standby throughout the district provided additional surge capacity. Identifying tertiary care centers geographically and with a set protocol ensured access for transfer to higher acuity care when needed within the district.
The participation of governmental, private, and NGOs was also seen as a success in this operation. The collaboration of these groups helped to ensure proper utilization of resources to provide care at no cost to patients. The PPP model has been well-studied in the development of infrastructure across India in the last 30 years, and more recently in the health care sector.Reference Birla and Taneja7-Reference Raman9 There have been international recommendations to push for PPPs to collaborate for disaster management and disaster risk reduction with the significance of identifying clear objectives and tasks for these partnerships to succeed.Reference Raman9,10 These recommendations have not established PPP roles in disaster response and relief. Operation Navajeevan represents an example of how clear established roles for different entities can strengthen the execution of medical relief to victims.
Operation Navajeevan was also unique because of the epidemiology of cases. By far, the most common reason for presentation to the camps was for exacerbation or on-going treatment of chronic medical conditions. This represents a drastic shift from prior floods in India, and other low- and middle-income countries (LMICs), where relief efforts describe a predominance of infectious diseases.Reference Angeline, Azbazhagan, Surekha, Joseph and Kiran11-Reference Saulnier, Brolin Ribacke and von Schreeb13 Data consistently demonstrate that in the immediate aftermath of floods, the incidence of infectious disease increases; a change that may be attributed to a combination of factors including contaminated water, disrupted sanitation systems, and over-crowded shelters.Reference Saulnier, Brolin Ribacke and von Schreeb13,14 Prior studies in India have shown outbreaks of acute respiratory infections, gastroenteritis, cholera, and leptospirosis after flooding.Reference Sur, Dutta, Nair and Bhattacharya15,Reference Karande, Bhatt, Kelkar, Kulkarni, De and Varaiya16 These mirror a similar leptospirosis outbreak seen during Operation Navajeevan and highlight the continued importance of infectious disease management following disasters; however, the overall epidemiologic profile of patients seen during Operation Navajeevan represents a new phenomenon in India and other LMICs. The reasons for this shift may be multifactorial, arising from a combination of increasing access to primary care in LMICs, globalization, and an aging population.
In recent years, the prevalence of noncommunicable diseases (NCDs) and their risk factors have increased throughout South Asia, an observation attributed to population aging and globalization.Reference Engelgau, El-Saharty, Kudesia, Rajan, Rosenhouse and Okamoto17 At the same time, access to basic medical care has improved. India has made substantial effort over the past ten years to improve access to health care.18 Kerala in particular has an especially developed health care infrastructure and access to health insurance is increasingly common.19 Additionally, Kerala has one of the highest literacy rates in India.Reference Sauvaget, Ramadas, Fayette, Thomas, Thara and Sankaranarayanan20 This combination of access to primary care with high patient literacy has resulted in improved baseline management of chronic disease conditions than may be available in other parts of India.Reference Nabae21 With improved access to primary care, a greater proportion of the population has access to medications to control chronic medical conditions. When the health care system is disrupted, as during a natural disaster, individuals lose access to medication and primary care treatment options, resulting in severe exacerbations of the underlying illness. While disruption of the health care system will result in an increase in communicable and NCDs alike, the dramatically increased prevalence of NCDs observed in Operation Navajeevan has not been previously described in LMICs. Prior reports have focused on such disruptions occurring in high-income countries such as documented during Hurricane Katrina (2005; USA) and other disasters.Reference Ringel, Chandra and Leuschner22-Reference Miller and Arquilla26 As access to health care continues to improve in LMICs, consideration of this changing epidemiologic profile will be crucial to future preparedness and relief efforts.
During Operation Navajeevan, over 5,300 patients, roughly 14.5% of all cases, presented to the camps for treatment of mental health conditions. One-half of these patients had pre-existing psychiatric diagnoses, and their primary medical need was resumption of their regular medications, most of whom had lost access to them during the flood. In order to combat the strain on these patients, psychiatrists and clinical psychologists were made available at the relief camps to offer counseling and support. Prior disaster response efforts in India have reported increases in the burden of psychiatric morbidity in the immediate aftermath of a disaster, but none as substantial as that seen during Operation Navajeevan.Reference Math, John and Girimaji27,Reference Math, Girimaji, Benegal, Uday Kumar, Hamza and Nagaraja28 Sharp increases in the psychosocial needs of displaced peoples have been previously reported.Reference Goenjian, Molina and Steinberg29 In recognition of the importance of treating mental health emergencies, the World Health Organization (WHO; Geneva, Switzerland) updated its Interagency Emergency Health Kit to include guidelines on clinical management of neuropsychiatric conditions during humanitarian emergencies in 2015.30 Operation Navajeevan’s experience of a much higher proportion of psychiatric cases during the flood bolsters the need to include mental health in disaster planning, and in turn, apply disaster management principles to mental health deployment.
Finally, a series of recent United Nations reports highlighting the impact of climate change project that LMICs, and India in particular, are expected to bear a disproportionate burden of extreme weather events over the next century.31-33 Already a disaster-prone country due to interplay between high population density, rapid urbanization, and geographic susceptibility, India currently ranks first in number of people affected by natural disasters and fifth in damage costs globally.Reference Guha-Sapir, Hoyois, Wallemacq and Below34 As the pace of global climate change continues to accelerate, it is foreseeable that these trends may continue.
Limitations
While the numbers reported here are large, there are no detailed data about the specific chronic medical conditions presented or prevalence of such conditions across different demographic groups.
Conclusion
Operation Navajeevan represents one of the first successful PPP systems to be utilized in disaster relief in India. The centrally coordinated approach allowed for judicious use of resources and helped avoid duplication of services. The replication of this system in other parts of Kerala shows the success of the approach used and could be adapted in other regions of India and beyond. As global climate change continues to accelerate, it is likely that extreme weather events will become increasingly common. It will be important for countries prone to natural disasters to develop strategies to mitigate these effects.
Conflicts of interest/funding
This work was presented at the 2018 Society of Emergency Medicine in India (SEMI) Academic Assembly in Bangalore, India and at the 2019 World Association for Disaster and Emergency Medicine (WADEM) Congress in Brisbane, Australia. There is no grant support or involvement. There are no conflicts of interest.
Author Contributions
Drs. Haris, Venugopalan, and Naveen organized and participated directly in the relief efforts during operation Navajeevan. Drs. Haris, Venugopalan, Davey, and Douglass conceived the idea for the field report. Drs. Haris, Venugopalan, and Naveen gathered and organized data for the report. Drs. Haris, Noll, Ghatik-Roy, Dreyer, Naik, Blanchard, and Davey conducted relevant background research and drafted the manuscript. All authors contributed substantially to the manuscript and its revision. Dr. Davey takes responsibility for the paper as a whole.





