Introduction
Optic nerve glioma (OPG) is a rare tumour comprising 1–5% of central nervous system tumours.Reference Heideman, Packer, Albright, Freeman and Rorke1 Children and adolescent patients are most commonly affected.Reference Alvord and Lofton2 Depending upon the tumour extent, there are symptoms including endocrine dysfunction like vision loss, proptosis, hydrocephalous, focal neurological symptoms, precocious puberty and short stature.
OPG has been associated with neurofibromatosis 1 (NF1) gene in 50–60% of cases.Reference Campen and Gutmann3
It is a type of tumour where pre-treatment tissue diagnosis is not mandatory, radiological–clinical findings are suffice. Its treatment is challenging due to tumour location and treatment-related effects. We are reporting a case of bilateral OPG in a patient who was treated with intensity-modulated radiotherapy (IMRT) in our department.
Case Presentation
An 18-year-old female presented with gradually deteriorating vision in both eyes. NF1 was ruled out clinically in the patient. Clinically the right eye had finger-counting at 1 m, sluggish pupillary reaction, diffuse disc pallor and severely depressed fields. The left eye had the perception of light, severe ptosis, more disc pallor and visual fields that are not assessable due to ptosis. MRI findings were diffuse thickening with mild contrast enhancement of bilateral optic nerves predominantly near the optic foramina. The biopsy report did not show any tumour. She was planned for IMRT with treatment to both eyes.
For planning computed tomography (CT), patient was positioned supine and head was immobilised with an Orfit (Scan-O-Plan, Vadora, India) cast. For treatment planning, contrast CT images were taken with slice thickness of 3 mm. Images were transferred to contouring system. Gross tumour volume was delineated as evident on planning CT. A 1 cm margin was taken for the clinical target volume (CTV), which was edited in air with clinical discretion. A 3 mm margin was taken for the planning target volume (PTV). Bilateral eye balls, lenses, optic chiasma and hippocampus were delineated as organs at risk (OARs). The dose to the PTV was prescribed as 54Gy,/ 1.8 Gy/#,/ 30 # days/week for 6 weeks. D95 distribution in the PTV has been shown in Figure 1 in both axial (a) and sagittal view (b). The treatment plan was created on Monaco treatment planning system version 3.1 (Elekta Ltd, Crawley, UK). It was optimised with nine beams with angles 0–320° with an internal space of 40°. The collimator and couch angles were kept at 0°. The beam’s isocentre was placed at the geometrical centre of PTV. The treatment plan was optimised in two phases using the Monte Carlo algorithm. The treatment was delivered on an ELEKTA synergy 6 MV Linear accelerator (Elekta Ltd) having 40 pairs of multi-leaf collimator by using a step and shoot IMRT technique. Dose constrains to OARs were respected during radiotherapy (RT) planning. Weekly Cone Beam CT was taken for verification. The patient had complaints of mild irritation, watery discharge in bilateral eyes after 4 weeks of RT which resolved with symptomatic treatment. At 8 weeks follow-up, clinically the patient had visual acuity unchanged, her vision had been stabilised. At 12 weeks, she was planned for MRI, but the patient was lost to follow-up and communication was made with the patient but she did not turn-up.
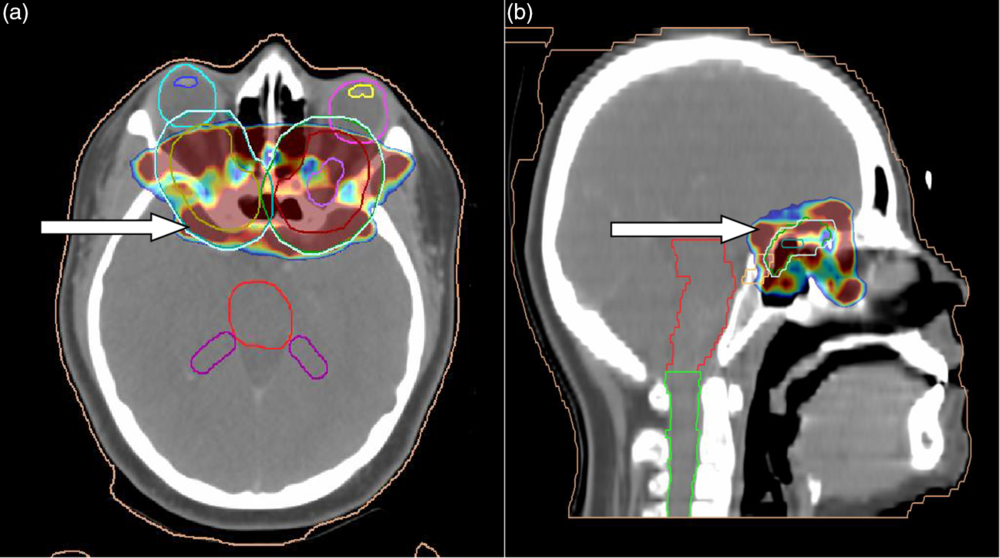
Figure 1. CT planning images (a) axial image: arrow indicating D95 coverage in colour wash; (b) sagittal image showing the same.
Discussion
OPG is a radiological and clinical diagnosis. A detailed ophthalmological examination including visual clinical examination, fundoscopy, Goldmann visual field and imaging studies (CT/MRI orbit and brain)Reference Tao, Barnes, Billett and Leong4 all are vital in knowing the tumour extent, response to treatment and prognosis.
Biopsy is not mandatory, but when feasible, a biopsy should be taken. Pilocytic astrocytoma is the most common variant. Usually, this tumour is an indolent type and can remain stable for years without evidence of disease progression. Rapid progression resulting in severe morbidity and death has been observed.Reference Nancy and Tarbell5
The aim of the treatment should be to preserve vision. However, the timing and selection of optimal treatment modality are always a clinical dialemma.Reference Jenkin, Angyalfi, Becker and Berry6 The treatment is to be initiated whenever there is deterioration in vision and/or increase in the size of tumour. The treatment modalities include surgery, RT and chemotherapy.
Surgery can be attempted for only optic nerve tumours,Reference Jenkin, Angyalfi, Becker and Berry6 advance OPGs with no vision and severe disfiguring proptosis. However, in the majority of cases, tumour extends to adjacent critical structures leading to unacceptable adverse effects and so surgery is avoided.
With early initiation of RT, vision loss can be minimised.Reference Flickinger, Torres and Deutsch7 Also, with RT, stabilisation of vision is possible. Studies have shown visual improvement in the range of 13–81% post-RT.Reference Tao, Barnes, Billett and Leong4,Reference Grabenbauer, Schuchardt, Buchfelder and Rödel8 Also, 10 years overall survival and progression-free survival have been 83% and 65·5%, respectively, with radiotherapy. However, caution should to be taken while selecting patients as in children less than 6 years, where risk of precocious puberty, growth hormone deficiency and cerebrovascular complications has been observed in studies.Reference Janss, Grundy, Cnaan and Savino9
Radiotherapy should be using a conformal technique. The patient’s MRI can be fused with the planning CT for better delineation of tumour. In centres, where fractionated stereotactic radiotherapyReference Combs, Schulz, Moschos and Thilmamm10 is available, the dose to the OARs can be minimised by smaller CTV margin of 1 mm and PTV of 3 mm.
Chemotherapy has been an effective treatment in young children with the aim of preservation and stabilisation of vision and delaying the radiotherapy.Reference Janss, Grundy, Cnaan and Savino9 Although chemotherapy shrinks the tumour, up to 60% of children have tumour progression after 5 years.Reference Kelly, Leary, Khanna and Weiss11 Various chemotherapeutic agents, for example, Vincristine, carboplatin, Etoposide and Temozolomide have been used.
Conclusion
OPG is a rare tumour. Its treatment is challenging due to tumour location and treatment-related effects. Improvement in vision and/or checking further progression should be the aim of selecting a treatment modality. Our patient had stabilisation of vision with IMRT. Radiotherapy using IMRT can be successfully used to treat OPG, and it checks tumour growth and prevents further deterioration.
Acknowledgements
We acknowledge the Radiation Oncology Department staff for their support in treatment of patient.
Financial Support
None.
Conflict of Interest
None.
Ethical Standards
The authors assert that this work comply with the ethical standards and has been approved by the institutional committee.




