Multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19 is a new entity that emerged with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak.1 MIS-C was first reported in the United Kingdom and was described as a severe Kawasaki-like illness. However, the phenotype of patients with MIS-C is expanding and now includes gastrointestinal, neurologic, haematologic, and renal manifestations.Reference Ramcharan, Nolan and Lai2,Reference Sood, Sharma, Sood, Sharma and Kaushik3 MIS-C usually occurs around 4–5 weeks after SARS-CoV-2 infection. Most patients with MIS-C are negative for nasopharyngeal swab but are positive for serum SARS-CoV-2 antibodies. These findings suggested that MIS-C is a post-viral inflammatory syndrome rather than a prolonged infection.Reference Capone, Subramony and Sweberg4,Reference Waltuch, Gill, Zinns and Whitney5
SARS-CoV-2 belongs to the Orthocoronavirinae subfamily of the Coronaviridae family, which exhibits tropism to myocardial and endothelial cells.Reference Lan, Ge and Yu6 Cardiac involvement is predominantly observed in patients with MIS-C. Left ventricular dysfunction, myocarditis, coronary artery abnormalities, mitral regurgitation, and pericardial effusion are the most common cardiac findings.Reference Haghighi Aski, Manafi Anari, Abolhasan Choobdar, Zareh Mahmoudabadi and Sakhaei7 Myocarditis is encountered in 51–90% of patients with MIS-C.Reference Haghighi Aski, Manafi Anari, Abolhasan Choobdar, Zareh Mahmoudabadi and Sakhaei7–Reference Whittaker, Bamford and Kenny9
Diagnosis of myocardial involvement by an objective measure tool remains a challenge in children. Standard echocardiography is primarily preferred as the imaging tool to assess cardiac involvement. However, its diagnostic accuracy is somewhat limited.Reference Chinali, Franceschini and Ciancarella10 Cardiac magnetic resonance may be an alternative imaging method, but it is also associated with some challenges in a paediatric population. The cardiac magnetic resonance process takes a long time and requires sedation in young children, it has high cost, and it is not feasible for recurrent evaluation.Reference Chinali, Franceschini and Ciancarella10 Speckle tracking echocardiography is a new method that has been reported to provide better data than conventional echocardiography for detection of subclinical left ventricular dysfunction and regional myocardial involvement. It was shown that speckle tracking echocardiography has better diagnostic and prognostic accuracy in patients with acute focal myocarditis than standard echocardiography.Reference Chinali, Franceschini and Ciancarella10 However, studies with speckle tracking echocardiography in MIS-C patients are limited.Reference Theocharis, Wong and Pushparajah11,Reference Kobayashi, Dionne and Ferraro12 A recent report of 20 patients with MIS-C showed that almost all patients had abnormal strain findings on admission. These findings suggested that speckle tracking echocardiography might be a good tool to assess and follow up myocardial function in patients with MIS-C.Reference Theocharis, Wong and Pushparajah11
Herein, we aimed to describe the early cardiac abnormalities and mid-term follow-up outcomes in patients with MIS-C evaluated by speckle tracking echocardiography.
Materials and methods
Patients and data source
This cross-sectional, single-centre study was conducted at the Division of Pediatric Cardiology, Kocaeli University. Patients diagnosed with MIS-C between November 2020 and April 2021 were enrolled in the study. The demographic, clinical and laboratory findings, treatments, and outcomes were collected prospectively with a standard proforma. Patients with pre-existing CHD or cardiomyopathy or in whom echocardiographic records were of too low a resolution to perform speckle tracking echocardiography were excluded from the study.
The diagnosis of MIS-C was made according to the World Health Organization and Centers for Disease Control and Prevention definitions.1,13 Acute myocarditis was defined in the presence of any of the following findings: elevated troponin; elevated N-terminal pro-B-type natriuretic peptide; ST segment elevation or depression on electrocardiogram; regional wall motion abnormalities; or decreased left ventricular function on echocardiography.Reference Dasgupta, Iannucci, Mao, Clabby and Oster14
Echocardiographic evaluation was performed at admission before any medical treatment. It was also routinely performed at discharge, 2 weeks and 2 months after discharge.
The control group consisted of 32 age- and gender-matched healthy children and adolescents who visited our hospital before the COVID-19 pandemic (pre-March 2020) for evaluation of heart murmurs or chest pain.
Patients were treated according to the following algorithm, which we reported previously.Reference Başar, Sönmez, Öncel, Yetimakman and Babaoğlu15 Patients were classified as mild, moderate, or severe according to the requirement for O2 support, vasoactive agents, or having organ dysfunction. All patients initially received intravenous immunoglobulin (2 g/kg) and enoxaparin (1 mg/kg). Intravenous corticosteroids (methylprednisolone) were given in patients with moderate and severe course. Anakinra was reserved for severe patients who were refractory to the standard therapy. All patients were discharged with acetylsalicylic acid (3–5 mg/kg) for 4–8 weeks.
Written informed consent was obtained from all patients and their parents. Ethical approval was obtained from the local ethics committee.
Laboratory investigations
Complete blood count, blood biochemistry, C-reactive protein, erythrocyte sedimentation rate, ferritin, procalcitonin, prothrombin time, activated partial thromboplastin time, D-dimer, fibrinogen, troponin-I, N-terminal pro-B-type natriuretic peptide, interleukin-6, and viral serology tests were performed on admission.
Conventional echocardiography
All patients underwent complete transthoracic echocardiography examination using a GE Vivid E9 ultrasound system (General Electric Healthcare, Horten, Norway) following recommendations for evaluation of cardiovascular imaging. B-mode and M-mode echocardiography images were obtained. Interventricular septal wall thickness, left ventricular posterior wall thickness, and left ventricular internal diameters were measured in all children. The systolic functions of the left ventricle were evaluated using fractional shortening, ejection fraction, and the left ventricular myocardial performance index. Cardiac chamber sizes and left ventricular systolic and diastolic functions were assessed in accordance with the guidelines of the American Society of Echocardiography.Reference Lang, Badano and Mor-Avi16 Ejection fraction >55% and fractional shortening >28% were considered normal. Mitral annular plane systolic excursion from the left ventricular apical four-chamber and tricuspid annular plane systolic excursion from the right ventricular apical four-chamber view was measured.
Coronary artery abnormalities were defined according to the American Heart Association guidelines for Kawasaki disease as follows: dilation (z-score = 2.0–2.49); small aneurysm (z-score = 2.5–4.9); moderate aneurysm (z-score = 5–9.9); and large/giant aneurysm (z-score ≥10).Reference McCrindle, Rowley and Newburger17
Pulsed Doppler measurements were obtained from all patients and the control group. The measurements included peak early diastolic filling (E) and late diastolic peak velocities (A). Tissue Doppler imaging was used to obtain peak systolic (Sʼ), early diastolic (Eʼ), and late diastolic (Aʼ) myocardial velocities at the lateral mitral annulus. To calculate the left ventricular myocardial performance index by tissue Doppler imaging, time intervals were measured from the septal mitral annulus. A value of myocardial performance index < 0.45 was considered as normal.
Speckle tracking echocardiography
Speckle tracking echocardiography examinations were performed offline on a dedicated workstation (Echocardiography PAC, Vingmed, General Electric, Horten, Norway) by one experienced paediatric cardiologist at presentation, discharge, and the second week and the second month after discharge, who was blinded to clinical and laboratory data. Grayscale images, which were obtained from the apical 4-chamber, 3-chamber, and 2-chamber views on three consecutive beats, were used to calculate regional and global longitudinal strain of the left ventricle. Parasternal short-axis views (at the level of the papillary muscle) were utilised to obtain circumferential and radial strain. Images of three consecutive cardiac cycles (60–90 frames/second) were uploaded to ECHO PAC, version 6.1.0 (GE Vingmed Ultrasound, Norway) software for analysis of speckle tracking–based myocardial mechanics. The software automatically split the images into six distinct segments, which were defined by the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association.Reference Capone, Subramony and Sweberg4 These segments were used to calculate longitudinal, radial, and circumferential strain values. Averages of the six segments in the four-, three-, and two-chamber views were taken to obtain global strain. A z-score of global longitudinal strain >−2 was considered normal and those with a z-score <−2 were abnormal, as previously described by Dallaire et al.Reference Dallaire, Slorach and Bradley18 Other important speckle tracking echocardiography derived parameters, such as left ventricular twist, and basal and apical rotation/twist were evaluated. Apical rotation was defined as a peak counterclockwise systolic rotation of the left ventricular apical short-axis cross-section, and basal rotation was defined as a peak clockwise systolic rotation of left ventricular basal short-axis cross-section level as viewed from the apex. Left ventricular twist was also calculated as the peak difference in systolic rotation angles obtained from the left ventricular apex and base.Reference Omar, Vallabhajosyula and Sengupta19
All segmental longitudinal strain, circumferential strain and radial strain, four-chamber longitudinal strain, two-chamber longitudinal strain, three-chamber longitudinal strain, global longitudinal strain, global longitudinal strain z-score, global circumferential strain, global radial strain, left ventricular twist, apical rotation and basal rotation values obtained from patients and controls were recorded. These parameters were compared between the patient group, both at admission and the second month of follow-up, and the control group. Additionally, we compared the baseline parameters at admission with those recorded at the second week and the second month after discharge in the patients. The association between cardiac findings and laboratory results was also evaluated.
Statistical Analyses
Statistical analysis was performed using IBM SPSS Statistics for Windows, version 20.0 (SPSS, Chicago, IL, USA). The study variables were investigated using visual (histogram and probability plots) and analytic methods (Kolmogorov–Smirnov and Shapiro–Wilk’s tests) to determine the normality of their distribution. Descriptive analyses are presented as frequency and percentage, mean and standard deviation or median and range, as appropriate. The parameters between patient and control groups were compared by Student’s t-test. Comparisons of follow-up parameters in patient group were carried out using the paired samples t-test, Wilcoxon test, repeated measures analysis of variance (ANOVA), or Friedman’s two-way ANOVA by Ranks, again, as appropriate. The associations between cardiac involvement, other clinical findings, and laboratory results were assessed by Spearman’s correlation analysis.
Results
Baseline clinical characteristics of patient and control groups
A total of 47 children and adolescents diagnosed with MIS-C were included in the study as the patient group. Among them, 30 (63.8%) were male and 17 (36.2%) were female. The mean age at diagnosis was 9.1 ± 4.3 (1.25–17) years. The mean body mass index was 18.93 ± 4.07 kg/m2.
Thirty-four (72.3%) patients had a history of contact with a SARS-CoV-2 infected patient at 40.6 ± 21 days before admission, while none of them had symptomatic infection. At diagnosis, SARS-CoV-2 polymerase chain reaction results were negative in all patients. Nineteen (40.5%) patients were positive for both SARS-CoV-2 IgG and IgM while 23 (48.9%) patients were positive for IgG only. The remaining five (10.6%) patients were negative for both COVID-19 polymerase chain reaction and antibody, while all of them had a positive history of contact with a symptomatic individual.
All patients were admitted to hospital with a complaint of fever lasting 4.4 ± 1.6 days. Beside fever, the most common clinical findings were gastrointestinal involvement in 43 (91.4%) patients; conjunctivitis in 24 (51.1%); and erythematous rash in 23 (48.9%). At admission, laboratory examination revealed lymphopenia in 33 (70.2%) and thrombocytopenia in 15 (31.9%) patients. All patients (100%) had elevated levels of C-reactive protein and procalcitonin, while erythrocyte sedimentation rate was elevated in 37 (78.7%) and ferritin in 14 (29.7%) patients. Forty (85.1%) patients had increased level of N-terminal pro-B-type natriuretic peptide, and 12 (25.5%) had elevated troponin-I levels.
The mean duration of hospitalisation was 8.9 ± 3.4 days. All patients were initially treated with intravenous immunoglobulin (2 g/kg). Two (4.2%) patients required a second dose of intravenous immunoglobulin. Nine (19.1%) patients received pulsed methylprednisolone for three consecutive days (15–30 mg/kg/day; maximum dose: 1000 mg/day) and then continued with a dosage of 2 mg/kg/day. Furthermore, 23 (48.9%) patients were treated with 2 mg/kg daily dose of steroid. Steroid treatment was tapered within 3 weeks. Five (10.6%) patients received anti-IL-1 (Anakinra), concomitantly. Five (10.6%) patients required intensive care. Of these five patients, three had normal ejection fraction at admission; subsequently, ejection fraction quickly depressed, and they needed inotropic agents. With the exception of one patient with mildly decreased left ventricular systolic function, all remaining patients were discharged free of symptoms and normalised laboratory findings. Demographic, clinic, and laboratory characteristics of the patient group are shown in Supplementary Table 1.
Thirty-two age- and sex-matched (20 male/12 female) children and adolescents who had attended for investigation of heart murmur or chest pain prior to the COVID-19 pandemic were enrolled as a control group. The mean age was 8.72 ± 3.85 (2.81–16.83) years. The mean body mass index was 17.35 ± 2.26 kg/m2. There was no difference between the MIS-C patients and the control group in terms of age, sex, and body mass index (p = 0.54, p = 0.90, and p = 0.16, respectively).
Conventional echocardiography findings
At admission, 25 (53.2%) patients had abnormal findings on conventional echocardiography. Among these, eight (32%) patients had left ventricular systolic dysfunction, eight (32%) had mild mitral valve insufficiency, five (20%) had myocarditis, three (12%) had pericardial effusion, two (8%) had coronary artery dilatation, one (4%) had moderate mitral valve insufficiency, and one (4%) had regional wall motion abnormalities. The mean ejection fraction and fractional shortening were 64.2 ± 1.15% and 34.6 ± 5.5%, respectively, in the patient group. However, ejection fraction was <55% in eight (17.1%) and fractional shortening was <28% in eight (17.1%) patients. Ejection fraction and fractional shortening were significantly lower in the patient group at admission compared to the control group (p = 0.013 and p = 0.010, respectively). There were no significant differences between the initial evaluation of the patient group and control group in terms of left ventricular M-mode values, pulse wave tissue Doppler, E waves, A waves, and E/A ratio, while the myocardial performance index was significantly higher in the patient group than in the control group (0.41 ± 0.14 vs 0.35 ± 0.05, p = 0.02). Mitral annular plane systolic excursion and tricuspid annular plane systolic excursion values were similar in both groups. In the patient group, ejection fraction (64.2 ± 1.15% vs 67.04 ± 3.31%, p = 0.045) and mitral annular plane systolic excursion (13.73 ± 2.83 mm versus 14.96 ± 2.28 mm, p = 0.037) were significantly higher at discharge than at admission. Other conventional echocardiographic findings were not significantly different at discharge compared to admission. Ejection fraction increased above 55% in 3.42 ± 0.53 days in seven of eight patients with left ventricular systolic dysfunction, but ejection fraction was 51% at discharge in one patient and left ventricular systolic dysfunction continued at the 6-month follow-up evaluation. There was no significant difference in the comparison of conventional echocardiography findings at admission and at the second month of follow-up in the patient group. M-mode values, pulse wave tissue Doppler values, E waves, A waves, E/A ratio, mitral annular plane systolic excursion, tricuspid annular plane systolic excursion, and the myocardial performance index were similar in the control group when compared with the second-month follow-up values in the patient group. Comparison of conventional echocardiography findings between patient and control group is shown in Supplementary Table 2.
When we compared the left ventricular M-mode and pulsed wave Doppler variables between the patient group at admission, at the second week and at the second month of follow-up, only ejection fraction was found to be statistically lower at admission than at the later two time points (64 ± 1.15% vs. 68 ± 3.3% and 67.55 ± 4.05%, p = 0.038).
Speckle tracking echocardiography findings
Global and segmental longitudinal strain, circumferential strain, and radial strain were examined. Except for the 4-chamber apicolateral, 3-chamber apicoposterior, and 3-chamber apical anteroseptal, all longitudinal strain parameters obtained with apical four-, three-, and two-chamber views were statistically impaired in the MIS-C group compared to the control group (Table 1). As detailed in Table 2, segmental longitudinal strain parameters of the patients at admission, at the second week and at the second month after discharge were compared. At admission, the 4-chamber apicoseptal, apical, mid and basal lateral, the 2-chamber apical, mid and basal anterior, the 3-chamber mid and basal anterior septal measures were statistically impaired compared to the second week and second month after discharge. At the second-month evaluation of the patient group in terms of the segmental longitudinal strain parameters, the 4-chamber mid and basal septal, 4-chamber basolateral, 2-chamber mid and basal inferior, 2-chamber mid and basal anterior, and 3-chamber mid posterior segments were still statistically impaired compared to the control group (p = 0.02, p = 0.003, p = 0.023, p = 0.001, p < 0.001, p = 0.001, p < 0.001, and p < 0.001, respectively). The remaining longitudinal strain parameters obtained from four-, three-, and two-chamber views were similar to the control group (Table 1).
Table 1. Comparison of left ventricle segmental longitudinal strains.

Data are expressed as mean ± standard deviation.
Table 2. Comparison of left ventricle segmental longitudinal strains in MIS-C patients at admission, at the second week, and at the second-month control visits.

Different lower case letters within the same line indicate statistical significance, while the same lower case letters indicate that there is no statistically significant difference. Data are expressed mean ± standard deviation.
Circumferential strain values in the anteroseptal and anterior region were found to be impaired in the patient group at admission compared to the control group (−16.5 ± 8.43% vs −20.6 ± 6.21%, p = 0.03 and −11.52 ± 8.11% vs −16.38 ± 7.6%, p = 0.02, respectively). Except for the septal region, all radial strain parameters were statistically lower in the patient group at admission compared to the control group. Anterior circumferential strain and radial strain in all regions were still significantly different between the control group and the second-month evaluation of the patient group (Table 3). The comparison of circumferential strain and radial strain parameters at admission, the second week and second month after discharge are shown in Table 4.
Table 3. Comparison of segmental circumferential strain and radial strain.

Data are expressed mean ± standard deviation.
Table 4. Segmental circumferential strain and radial strain in MIS-C patients at admission, at the second week, and at the second-month control visit compared to controls.

Different lower case letters within the same line indicate statistical significance, while the same lower case letters indicate that there is no statistically significant difference. Data are expressed mean ± standard deviation.
As illustrated in Table 5, there were statistical differences between the patient group (at admission and 2 months of follow-up) and the control group in terms of four-chamber longitudinal strain, two-chamber longitudinal strain, three-chamber longitudinal strain, global longitudinal strain, and global radial strain. Global circumferential strain measurements were similar between the values of the patient group at admission and the second month of follow-up and the control group. When we compared the global longitudinal strain, circumferential strain, and radial strain in the patient group at follow-up, we found significant difference in term of four-, two-, and three-chamber longitudinal strain, global longitudinal strain, and global longitudinal strain z-score. The mean global longitudinal strain value was −15.53 ± 4.89% at admission, and −17.23 ± 8.02% at the second month of follow-up. Global circumferential strain and radial strain were not different (p = 0.241 and p = 0.872) (Table 6). Global longitudinal strain z-scores were lower than −2SD in 29 patients at admission while 13 patients still had global longitudinal strain z-scores <−2SD at the second month.
Table 5. Comparison of global strains, twist, apical rotation, and basal rotation between MIS-C patients at admission, at the second-month follow-up of the patients and controls.

Data are expressed Mean ± standard deviation.
Table 6. Comparison of global strains, twist, apical rotation and basal rotation in MIS-C patients at admission, at the second week, and at the second-month control visit.

Different lower case letters within the same line indicate statistical significance, while the same lower case letters indicate that there is no statistically significant difference.
When we analysed the relationship between laboratory parameters and left ventricular myocardial deformation, there were no significant differences between patients with impaired global longitudinal strain and those with normal global longitudinal strain in terms of laboratory findings, with the exception of D-dimer (3.29 µg/mL versus 1.56 µg/mL, p = 0.04). IL-6 levels tended to be higher in patients with impaired global longitudinal strain than in those with normal global longitudinal strain, although this did not reach significance (median 197.6 pg/mL vs 32.4 pg/mL, p = 0.63). When we compared troponin levels with laboratory tests and echocardiography parameters, fibrinogen levels were significantly higher (6.03 ng/mL vs 4.63 ng/mL, p = 0.032) while lymphocyte counts (696 cell/µL vs 1142 cell/µL, p = 0.012), baseline ejection fraction (59.17% vs 66.11%, p = 0.006), and fractional shortening (31.6% vs 35.6%, p = 0.026) were lower in patients with high troponin levels compared to those with normal troponin levels. N-terminal pro-B-type natriuretic peptide levels tended to be higher in patients with high troponin levels compared to others (median 5350 ng/mL vs 699 ng/mL, p = 0.059) although this did not reach significance (Supplementary Table 3).
The examples of speckle tracking echocardiography images of patients are given in Figure 1.
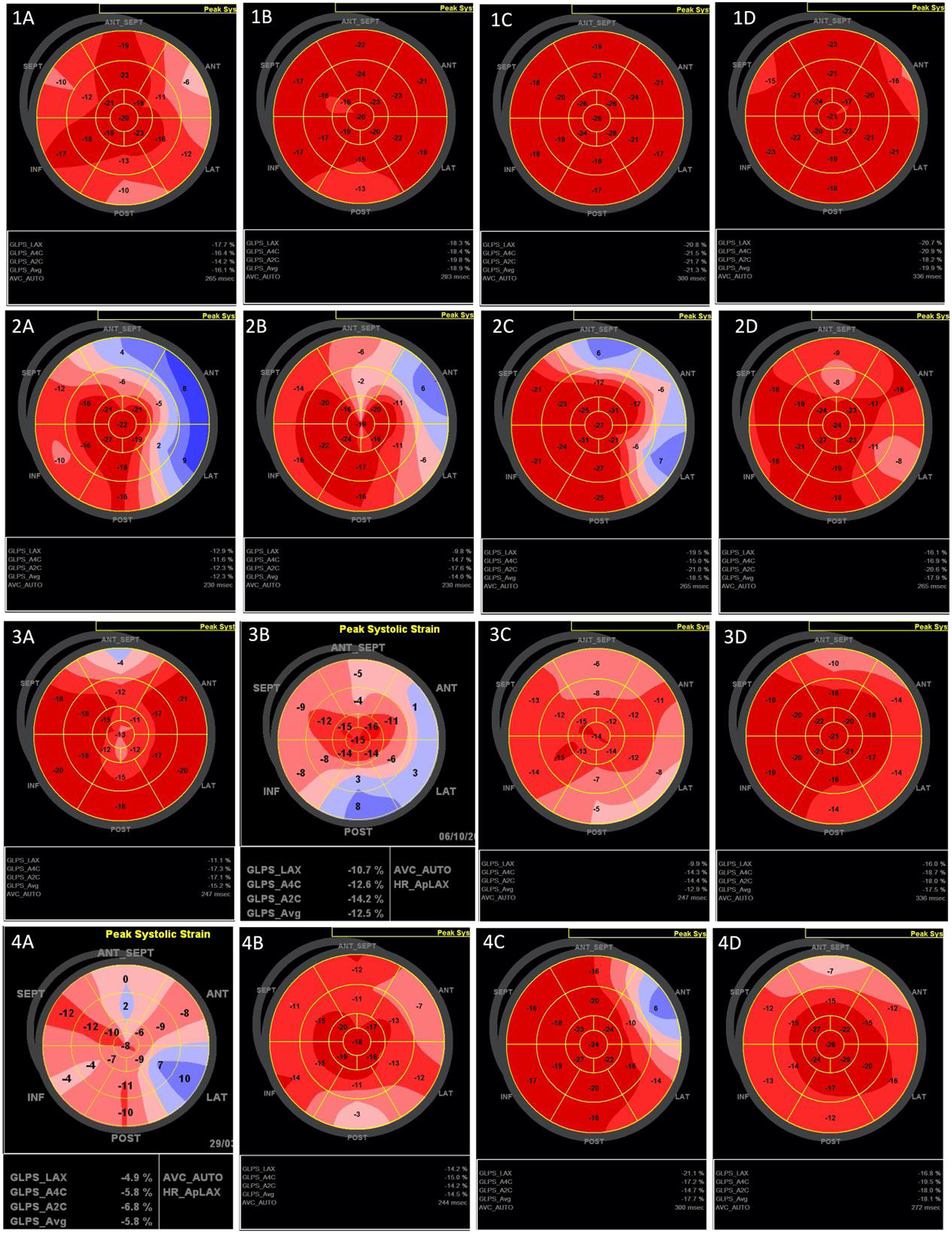
Figure 1. Patient 1: While the global longitudinal strain was mildly impaired (global longitudinal strain −16%) at admission ( 1A ), it increased during the follow-up and returned to normal limits at discharge ( 1B ). ( 1A : admission, 1B : discharge, 1C : 2 weeks of follow-up, 1D : 2 months of follow-up). Patient 2: The global longitudinal strain was impaired on admission ( 2A ) and still not in the normal range at discharge ( 2B global longitudinal strain: −14%). During the follow-up, global longitudinal strain increased and returned to normal limits at the end of the 2-month follow-up ( 2A : admission, 2B : at discharge, 2C : second week of follow-up, 2D : second month of follow-up). Patient 3: Global longitudinal strain −15.2% was detected in Patient 3 at admission. At the 12th hour of intravenous immunoglobulin treatment, the patient was taken to the ICU because of deterioration in his general condition. Figure ( 3B ) showed the bulls-eye plot of the patient in the ICU. At discharge ( 3C ), improvement in global longitudinal strain was observed. At the second month of follow-up ( 3D ), the global longitudinal strain was found to be within normal limits (3A: admission, 3B : second day of admission, 3C : second week of follow-up, 3D : second month of follow-up). Patient 4: While the global longitudinal strain was severely impaired (Global longitudinal strain −5.4%) at admission ( 4A ), it was observed that the global longitudinal strain showed rapid improvement during follow-up and returned to normal limits by the second month ( 4D ). ( 4A : admission, 4B : discharge, 4C : second week of follow-up, 4D : second month of follow-up).
Discussion
Cardiac involvement, such as left ventricular dysfunction, mitral valve regurgitation, pericardial effusion, and coronary abnormalities, is widespread in MIS-C and have prognostic significance. Our results confirmed that cardiac involvement is very common and therefore may be important in the management of MIS-C patients. Early detection of cardiac involvement is crucial in guiding treatment. In the present study, while in 17% of patients (8/47) ejection fraction was below 55%, the global longitudinal strain z-scores were abnormal in 61.7% (29/47) of patients. Furthermore, we found that the impaired left ventricular myocardial function continued at the second month following discharge when using speckle tracking echocardiography. Evaluating MIS-C patients with speckle tracking echocardiography in addition to conventional echocardiography may help early recognition of cardiac findings and improve follow-up too.
MIS-C is a rare complication of SARS-CoV-2. Although the exact incidence is unknown, in a previous study, the incidence of MIS-C in children with confirmed SARS-CoV-2 infection was reported as 2 per 100,000.Reference Dufort, Koumans and Chow20 Furthermore, Verdoni et al reported a 30-fold increased incidence of Kawasaki-like disease among children infected with SARS-CoV-2, and these children are at higher risk of presenting with macrophage activating syndrome and Kawasaki disease shock syndrome compared to classical Kawasaki disease patients.Reference Verdoni, Mazza and Gervasoni21 Cardiovascular findings have an important place in the prognosis of the disease in all patients. Like other betacoronaviruses, SARS-CoV-2 shows tropism to many cells, including endothelial and epithelial cells in the lung, gastrointestinal tract, and myocardium cells. Dolhnikoff et al. detected SARS-CoV-2 particles in the cardiac tissue of a child affected by MIS-C.Reference Dolhnikoff, Ferreira Ferranti and de Almeida Monteiro22 The autopsy of this patient showed pancarditis with tissue inflammation and necrosis of cardiomyocytes. The authors suggested that the presence of SARS-CoV-2 in heart tissue was the primary cause of myocardial inflammation. Nevertheless, besides the direct effect of the virus on the myocardium, many mechanisms such as systemic inflammation, hypoxia, stress cardiomyopathy, or coronary artery involvement are also suggested in the pathogenesis of cardiac dysfunction.
The majority of patients with MIS-C had cardiovascular involvements but the nature of cardiac involvement is quite different from Kawasaki disease, with a predominance of left ventricular dysfunction rather than coronary artery involvement.Reference Feldstein, Tenforde and Friedman23 A multicentre study from the United States of America, including 186 patients with MIS-C, showed that approximately 80% of them presented with cardiovascular involvements and half of them required vasoactive support. A recent study from Europe reported depressed left ventricular ejection fraction in 34.2%, regional wall motion abnormalities in 6.6% and reduced global longitudinal strain in 11.5% of patients with MIS-C.Reference Valverde, Singh and Sanchez-de-Toledo24 Therefore, it is important to examine cardiac function in MIS-C in more detail. Most recently, Kobayashi et alReference Kobayashi, Dionne and Ferraro12 evaluated cardiac function of 25 patients with MIS-C using speckle tracking echocardiography. They reported depressed left ventricular ejection fraction in 40% (n = 10) of the patients with MIS-C. Additionally, 27% (n = 4) of the patient whose initial ejection fraction was normal (n = 15) had a depressed peak systolic circumferential strain. Furthermore, higher levels of brain natriuretic peptide and procalcitonin were detected among MIS-C patients with abnormal systolic strain than those of patients with normal strain values. Based on these findings, the authors suggested that detection of left ventricular systolic dysfunction might be improved by using strain imaging. Matsubara et alReference Matsubara, Kauffman and Wang25 evaluated the cardiac function of 28 patients with MIS-C using speckle tracking echocardiography. They showed impaired global longitudinal strain, global circumferential strain, peak left atrial strain, and peak longitudinal strain values in MIS-C patients at diagnosis. They also reported that higher brain natriuretic peptide levels were significantly associated with lower peak systolic circumferential strain and longitudinal strain. Correspondingly, in the present study, left ventricular systolic dysfunction was detected in eight patients by conventional echocardiography while abnormal global longitudinal strain z-score was found in 29 patients. Furthermore, we showed depressed circumferential strain values in the anteroseptal and anterior region in the patient groups at admission compared to the control group. Interestingly, in segmental longitudinal strain assessment, mid and basal segments were predominantly impaired while the apical segment was less affected. MIS-C patients with abnormal strain values had higher IL-6 and D-dimer levels. However, we could not demonstrate any differences between patients with abnormal strain findings and those with normal strain values in terms of brain natriuretic peptide levels.
The myocardial performance index is a non-invasive assessment method to show both systolic and diastolic function that may be obtained easily by Doppler mode echocardiography. The myocardial performance index has been used to reflect global cardiac function in patients with varying diagnoses, such as dilated cardiomyopathy, hypertrophic cardiomyopathy, and congestive heart failure.Reference Tei, Ling and Hodge26–Reference Bruch, Schmermund and Marin28 Moreover, studies demonstrated that the myocardial performance index is a simple, sensitive, and accurate tool for estimating global myocardial dysfunction in patients with Kawasaki diseaseReference Matsubara, Kauffman and Wang 25 , Reference Ajami, Borzouee and Amoozgar 29 , Reference Song, Yoon and Cho 30 However, there is not enough data on the accuracy of myocardial performance index in MIS-C patients. At initial assessment, we found that the myocardial performance index was significantly higher in the patient group than the control group (0.41 ± 0.14 vs 0.35 ± 0.05, p = 0.02) while this difference had disappeared by the second month of follow-up. These results suggest that the myocardial performance index seems to be beneficial for assessing global left ventricular function in patients with MIS-C at diagnosis and is also beneficial for monitoring recovery during follow-up.
It is known that left ventricular twist plays an important role in the mechanical efficiency of the heart. Left ventricular twist may provide an easily assessable marker of subendocardial ischaemia in hypertrophic cardiomyopathy or aortic stenosis. The increased basal rotation may be explained by loss of counteraction of the subendocardial fibre helix, caused by endocardial ischaemia due to microvascular dysfunction. Previous studies in acute myocarditis using cardiac magnetic resonance documented that the subepimyocardial fibres are primarily involved. Khoo et al evaluated tissue deformation and twist to detect subclinical ventricular dysfunction in 28 patients with myocarditis. They suggested twist rate and earlier time to peak twist as a predictor of myocarditis. However, they found no change in peak systolic twist. They emphasised that deformation and twist parameter could improve the detection of myocardial involvement.Reference Khoo, Smallhorn, Atallah, Kaneko, Mackie and Paterson31 In the present study, there was no statistical significance between MIS-C patients and controls in terms of left ventricular twist, basal rotation, and apical rotation at the diagnosis and during follow-up.
Longitudinal follow-up is crucial to monitor cardiac outcomes. Left ventricular dysfunction may be persistent in some patients at follow-up. Even in patients with normal ejection fraction, strain assessment may indicate impaired left ventricular systolic and diastolic functions. Kobayashi et alReference Kobayashi, Dionne and Ferraro12 demonstrated that depressed left ventricular functions normalised in 80% of MIS-C patients at discharge while abnormal systolic strain patterns persisted in 36% of MIS-C patients. In the present study at the second-month control, it was shown that ejection fraction normalised in all patients except one with an ejection fraction of 51% but 13 (27.6%) patients had persistently abnormal global longitudinal strain z-scores of <−2 SD. Xu et alReference Xu, Ding and Lv32 investigated left ventricular systolic longitudinal strain in patients with Kawasaki disease, which has similarities to MIS-C. They reported the left ventricular systolic longitudinal strain decreased significantly in the acute phase of Kawasaki disease and recovered to normal at 6–8 weeks after disease onset. In line with this, Kayabey et alReference Kayabey, Tuncer, Deveci, Başar and Babaoğlu33 showed that left ventricular functions were similar between patients with Kawasaki disease and healthy controls in the late period of follow-up. They emphasised that cardiac function in children with Kawasaki disease are not affected in the long-term. Acute myocarditis is characterised by viral damage to the cardiac muscle, which might be either direct or mediated by an immune reaction. Chinalli et al.Reference Chinali, Franceschini and Ciancarella10 evaluated the acute and sub-acute period in focal myocarditis, and they showed impaired longitudinal strain in 58% of patients who had normal ejection fraction at presentation. Furthermore, they observed persistent global and regional impairment in 18.1% of patients at follow-up. These authors suggested that speckle tracking echocardiography might be more sensitive for the detection of subclinical left ventricular dysfunction in acute focal myocarditis.
However, the data on long-term cardiac function in patients with MIS-C is scarce. Gaitonde et alReference Gaitonde, Ziebell and Kelleman34 evaluated the follow-up cardiac function of 12 patients with MIS-C. They demonstrated depressed ejection fraction with reduced global longitudinal strain in eight patients and reduced global longitudinal strain in six patients at diagnosis. These authors also reported that ejection fraction was normalised in all except one at discharge, while six patients still had reduced global longitudinal strain values. Furthermore, Sanil et alReference Sanil, Misra and Safa35 reported that subclinical left ventricular dysfunction persisted up to the 10-week follow-up after discharge in patients with MIS-C and they emphasised that left ventricular global longitudinal strain and left ventricular apical four-chamber peak longitudinal strain were important parameters in monitoring long-term cardiac function. Similarly, we found that left ventricular apical four-chamber longitudinal strain and global average longitudinal strain were affected at admission and at the second-month control visit. Therefore, long-term cardiac evaluation is as crucial as acute cardiac evaluation in MIS-C patients. During the acute and convalescent phases of the disease, speckle tracking echocardiography is more sensitive than conventional echocardiography to evaluate global and regional myocardial deformation. Since MIS-C is a new disease, it is not known how its course will change from patient to patient. It is very important to determine the prognostic factors in order to personalise the treatment. In the present study, among five patients requiring intensive care, three had normal ejection fraction at admission while all had depressed global longitudinal strain. We suggest that even in the presence of normal ejection fraction, patients with depressed global longitudinal strain should be followed up closely, especially during the administration of intravenous immunoglobulin, to avoid volume overload.
In addition to echocardiographic findings, biochemical markers, such as brain natriuretic peptide and troponin levels, are important for describing cardiac involvement. Previous studies suggested that brain natriuretic peptide and troponin are the most important laboratory markers to indicate cardiac involvement in MIS-C patients.Reference McMurray, May, Cunningham and Jones36 Most recently, a study evaluating the acute cardiovascular manifestations in 286 patients with MIS-C showed that the majority of patients had significantly raised levels of NT-pro-BNP (94%) and troponin (93%).Reference Valverde, Singh and Sanchez-de-Toledo24 In contrast to this study, we found that 40 (85.1%) patients had increased levels of pro-brain natriuretic peptide while troponin levels were elevated in only 12 (25.5%) patients. Similarly, Belhadjer et alReference Belhadjer, Méot and Bajolle37 showed mildly to moderately elevated troponin levels among 35 MIS-C patients presenting with acute heart failure, in keeping with our findings. They suggested that the underlying mechanism of heart failure was not compatible with a classical course of myocarditis. Furthermore, we could not observe any correlation between longitudinal strain parameters and brain natriuretic peptide levels in our patients.
Our study is limited by its single-centre design, but including a large number of patients and evaluation of their long-term cardiac function strengthens it.
In conclusion, our main finding was that in patients with MIS-C, speckle tracking echocardiography is an important tool for the identification of a reduction in global or segmental longitudinal strain, circumferential strain, and radial strain. Since early treatment is very important in these patients, speckle tracking echocardiography should be used routinely. Our studies suggest that, despite any absence of clinical signs of heart failure, myocarditis may lead to subclinical mid- and long-term cardiac dysfunction in MIS-C. Speckle tracking echocardiography is more likely to detect subclinical myocardial damage compared to conventional echocardiography, and global and regional myocardial deformation should be evaluated during follow-up.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951122000646
Acknowledgements
The authors are grateful to Mr Jeremy Jones of the Academic Writing Department of Kocaeli University, Izmit, Turkey, for his assistance in editing the English used and for his help and advice concerning the contents of this manuscript.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
Written informed consent was obtained from all patients and their parents. Ethical approval was obtained from the local ethics committee.










