Introduction
Thyroglossal duct cysts are common congenital anomalies that are usually easy to diagnose, although they may present with unusual clinicopathological features. In this report, we describe cases of branching, polycystic thyroglossal duct cyst and giant thyroglossal duct cyst in two patients with no previous surgical history.
Case reports
Case one
An 11-year-old boy was referred to the Nagoya First Red Cross Hospital with a cervical mass. Examination revealed a left paramedian cervical mass over the hyoid bone and a paramedian cervical mass below the hyoid bone.
Computed tomography (CT) demonstrated two low density masses; radioisotope scanning showed no functioning thyroid tissue in the masses. Magnetic resonance imaging (MRI) showed high signal intensity masses on T1-weighted images. Sagittal, T1-weighted MRI scans suggested that the two masses were connected (Figure 1). This strongly suggested a polycystic thyroglossal duct anomaly.

Fig. 1 Patient one: sagittal, T1-weighted magnetic resonance imaging scan showing high signal intensities for, and continuity between, the two masses.
At surgery, a cyst measuring 20×20×20 mm was found in the midline between the hyoid bone and the thyroid cartilage. As the tract of the cyst was followed in the cephalad direction, another cyst measuring 40×55×40 mm was found over the hyoid bone. The tracts connecting these two cysts fused in the midline just below the hyoid bone (Figure 2). The residual hyoid bone was removed, along with a fibrous tract which extended into the muscles of the base of the tongue. The tract over the hyoid bone was divided at the point close to the hyoid bone, in the direction of the foramen caecum.

Fig. 2 Patient one: intra-operative photograph showing the two tracts fused in the midline just below the hyoid bone. The forceps pinch the end of the resected hyoid bone.
Post-operative recovery was uneventful.
Histological examination showed that the larger cyst was lined with squamous epithelium (Figure 3), with haemorrhage and chronic inflammation in the cyst wall. In contrast, the smaller cyst was lined with pseudostratified, columnar, ciliated epithelium, with scattered, colloid-containing thyroid acini (Figure 4).

Fig. 3 Patient one: photomicrograph showing the wall of the larger cyst lined by squamous epithelium (H&E; ×160).

Fig. 4 Patient one: photomicrograph showing the wall of the smaller cyst lined by pseudostratified, ciliated, columnar epithelium, with colloid-containing thyroid acini (H&E; ×160).
Case two
A 41-year-old man was referred to Nagoya University Hospital with the chief complaint of a cervical mass. He had ignored the mass for three years, but came to our hospital because the mass had gradually increased in size. Palpation revealed a left paramedian cervical mass (Figure 5). The tumour measured 90×95×90 mm by CT image.

Fig. 5 Patient two: clinical photograph showing large, left-sided, paramedian cervical mass.
Ultrasonography of the cervical portion of the mass revealed a cystic lesion. An enhanced CT showed a cystic mass 90 mm in diameter with clear boundaries and a contrasting cyst wall (Figure 6).

Fig. 6 Patient two: axial, enhanced computed tomography scan showing a 90 mm diameter, cystic mass with clear boundaries and a contrasting cyst wall.
Surgical removal of the mass followed the method of Sistrunk. The hyoid bone was cut away from the hyoid midline, from 3 cm to the left to 5 cm to the right. The tract was divided at a point close to the hyoid in the direction of the foramen caecum, and the cyst was removed. The cyst measured 95×85×75 mm and weighed 330 g. Dark brown liquid had pooled in the cyst.
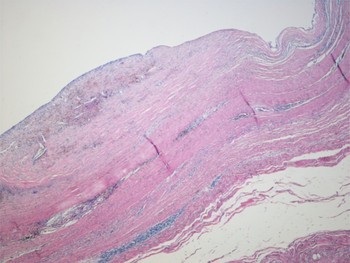
Microscopically, the cyst wall comprised mainly fibrous connective tissue with partially stratified squamous epithelium. No thyroid tissue or malignancy was evident. Most of the epithelium lining the cyst wall had exfoliated (Figure 7).

Fig. 7 Patient two: photomicrograph showing the cyst wall lined by fibrous connective tissue and partially stratified squamous epithelium. Most of the cyst wall epithelial lining has exfoliated (H&E; ×160).
Discussion
We describe two cases of thyroglossal duct cysts. One case involved a branching, polycystic thyroglossal duct cyst, which is very rare; this is only the sixth report, and the first to include MRIs and clear photographs (Table I).Reference Ward, Strahan, Acquarelli and Harris1–Reference Tovi and Eyal5 The other case involved a giant thyroglossal duct cyst, which is also rare. This giant thyroglossal duct cyst appears to be the largest described in the literature (Table II).Reference Keynes6–Reference Shahin, Burroughs, Kriby and Ali9
Table I Reports of multiple thyroglossal duct cysts

Pt = patient; y = years; HB = hyoid bone; ND = not described; M = male; F = female
Table II Reports of giant thyroglossal duct cyst

Pt = patient; y = years; M = male; ND = not described
Thyroglossal duct cysts occur most often in young patients, with an almost equal sex distribution.Reference Allard10 The sinuses are rarely involved.Reference Judd11 Almost 70 per cent of such cysts occur below the level of the hyoid bone, and only 25 per cent are found in a suprahyoid position.Reference Ward, Strahan, Acquarelli and Harris1 Thyroglossal duct cysts do not usually communicate with the skin. When they present with fistulous openings in the skin, there is always a history of infection and spontaneous drainage, or inadequate surgery.Reference Ward, Strahan, Acquarelli and Harris1, Reference Noyek and Friedberg3 The characteristic feature of multiple thyroglossal duct cysts, described in a previous paper, is that they almost always occur after attempted resection and seem to be residual tracts.Reference Ward, Strahan, Acquarelli and Harris1–Reference Noyek and Friedberg3, Reference Tovi and Eyal5 However, in our first case multiple thyroglossal duct cysts occurred in a patient with no history of resection.
Magnetic resonance imaging is useful for detecting thyroglossal duct cysts, because of its high resolution and ability to generate qualitative data about a mass, and because it does not involve radioactivity.Reference Blandino, Salvi, Scribano, Chirico, Longo and Pandolfo12 In our first case, sagittal, T1-weighted MRI scans showed high signal intensities for, and continuity between, the two masses. This case represents the first report of such continuity between two thyroglossal duct cysts viewed on MRI. These two thyroglossal duct cysts probably formed because the thyroglossal duct persisted as multiple tracts during hyoid bone development, and some portions then developed into cysts.Reference Bennet, Organ and Williams13
The method of Sistrunk is recommended for surgical removal of a thyroglossal duct cyst with a tract.Reference Sistrunk14 The tract usually runs up posteriorly and cranially at the inferior edge of the hyoid bone, then wraps around behind the hyoid bone and continues to course up anteriorly and cranially from the hyoid bone.Reference El-Silimy and Bradley15 Therefore, these tracts and cysts should be removed together, because a remaining duct may cause a recurrence. In cases of surgical removal without hyoid resection, the recurrence rate is more than 50 per cent.Reference Lawson and Fallis16 Moreover, following histological study of 10 specimens obtained from surgery following Sistrunk's method, Horisawa et al. recommended that the tract between the hyoid bone and foramen caecum should be removed at a point close to the hyoid bone.Reference Horisawa, Niinomi and Ito17 We used the methods of Sistrunk and Horisawa in treating our two patients. These patients' post-operative courses were uneventful, and neither showed any signs of recurrence.
• This paper discusses the management of branching polycystic and giant thyroglossal duct cysts, with reference to two cases
• Patients were operated upon according to the methods of Sistrunk and Horisawa; both had a satisfactory post-operative course
• The anatomy of the hyoid bone is key to successful surgery for unusual thyroglossal duct cysts
Common histopathological features of thyroglossal duct anomalies include a lining of ciliated columnar epithelium, although squamous, transitional or mixed epithelial forms may also be present. Islands of thyroid tissue or scattered thyroid acini are often seen along the tract or in the subepithelial layer of the cyst.Reference Ward, Strahan, Acquarelli and Harris1, Reference Sade and Rosen18 Cysts occurring above the hyoid bone are more often lined with stratified squamous epithelium, and those located below the hyoid bone are more commonly lined with columnar epithelium.Reference Lucas and Lucas19 During development of a thyroglossal duct cyst, the superior part of the tract sometimes degenerates, leaving behind only scattered islands of thyroid follicles.Reference Remy20
The histopathological findings of our first case were similar to those reported previously below and above the hyoid bone.Reference Lucas and Lucas19, Reference Remy20 In our second case, the cyst wall comprised mainly fibrous connective tissue and some stratified squamous epithelium, and most of the epithelium lining the cyst wall had exfoliated. This thyroglossal duct cyst grew to a large size, but did not involve the laryngeal portion. Exfoliation of the epithelium lining the cyst wall probably occurs when epithelial growth is extensive.
Conclusion
Surgical removal of an anomalous thyroglossal duct cyst should use a technique based on the anatomy of the hyoid bone region.