Abernethy malformation, also known as congenital extrahepatic portosystemic shunt, is a very rare condition where the portal system drains into the systemic circulation bypassing the liver completely or partially through the portosystemic shunt. Type 1 Abernethy malformation indicates a total shunt where the liver is not perfused with portal blood. It is further classified as type 1A, where splenic and superior mesenteric veins drain separately into inferior caval vein and type 1B, where splenic and superior mesenteric veins form portal vein that drains separately into the inferior caval vein. Type 2 Abernethy malformation indicates a partial shunt where the liver is perfused with portal blood. Reference Morgan and Superina1,Reference Azad, Arya, Sitaraman and Garg2 The clinical manifestations of Abernethy malformation are variable. The affected individual may be asymptomatic or presents with hepatic encephalopathy, multiple liver nodules/tumours, or symptoms due to pulmonary hypertension or hepatopulmonary syndrome. Reference Xie, Li, Jiang, Zhao and Xiao3 Abernethy malformation may also co-exist with systemic venous anomalies as their embryological development is closely related. Reference Sheth and Sivakumar4 In this report, we present a child with Abernethy malformation associated with inferior caval vein interruption, venous thrombosis, and multiple venous collaterals, in whom a percutaneous closure was successfully performed.
Case report
A 5-year-old boy was referred to us with symptoms of failure to thrive since early infancy. Examination revealed the presence of significant pulmonary hypertension with no evidence of arterial desaturation. Chest X-ray showed mild cardiomegaly with prominent pulmonary artery segment and ECG showed evidence of right ventricular hypertrophy. On echocardiography, he was found to have dilated right atrium and right ventricle. There was no tricuspid or pulmonary regurgitation to quantify the severity of pulmonary hypertension. A CT angiography was done as part of a workup for pulmonary hypertension. Chronic thromboembolic pulmonary arterial hypertension was ruled out on CT angiography. CT angiography of the chest revealed an abnormal communication between the main portal vein and intrahepatic inferior caval vein suggestive of Abernethy malformation type 2. Subsequently, a CT of the abdomen was done (Fig 1). The portal vein branches were normal in calibre. In addition, the intrahepatic inferior caval vein was interrupted and a dilated azygos vein was arising from the dilated left renal vein. The left internal iliac vein was thrombosed and the left common femoral vein was draining into the paraverterbral venous plexus. The right common iliac vein also showed some filling defects suggestive of non-occlusive thrombi, and this was draining into the inferior caval vein. There was no other venous anomaly noted on the CT abdomen. Ammonia level was not done in this patient.
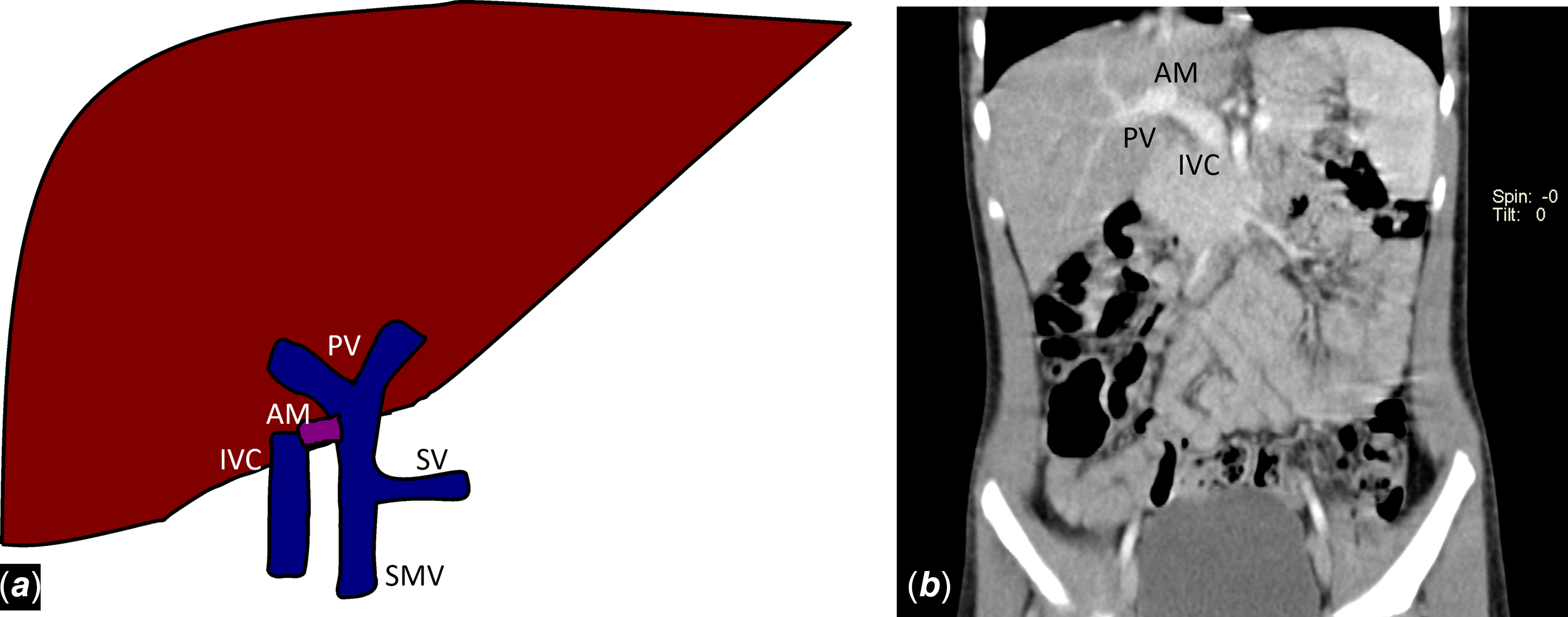
Figure 1. (a) Cartoon showing Abernethy malformation type 2 with interrupted IVC. (b) Abdominal CT angiogram coronal section showing Abernethy malformation with interrupted IVC. AM = Abernethy malformation; IVC = inferior caval vein; PV = portal vein; SMV = superior mesenteric vein; SV = splenic vein.
Patient was taken up for cardiac catheterisation for assessing pulmonary artery pressure and to occlude the Abernethy malformation with a device. Right femoral vein could not be cannulated initially and an angiogram from the left femoral vein sheath showed filling of paravertebral venous plexus. A discrete inferior caval vein could not be defined. A dilated azygos vein was seen draining into the superior caval vein and then into the right atrium (Fig 2). A right femoral venous access was successfully obtained a week later. A guide wire passed up to the infrahepatic part of inferior caval vein, went into the communication with the portal system through the portosystemic shunt. The shunt anatomy was defined further with angiography (Fig 3a and b; Supplementary video S1). It was a bulbous communication. The angiography also confirmed an interrupted intrahepatic inferior caval vein and filling of portal radicals through the shunt. The portal vein was selectively catheterised through the shunt and an angiogram showed filling of the good-sized portal radicals. A right heart study done through right internal jugular venous access revealed severe pulmonary artery hypertension with pulmonary artery pressure of 115/60 mmHg (mean 83 mmHg). Since the portal radicals were well formed, the balloon occlusion test was not done and we decided to go ahead with the closure of the portosystemic shunt.
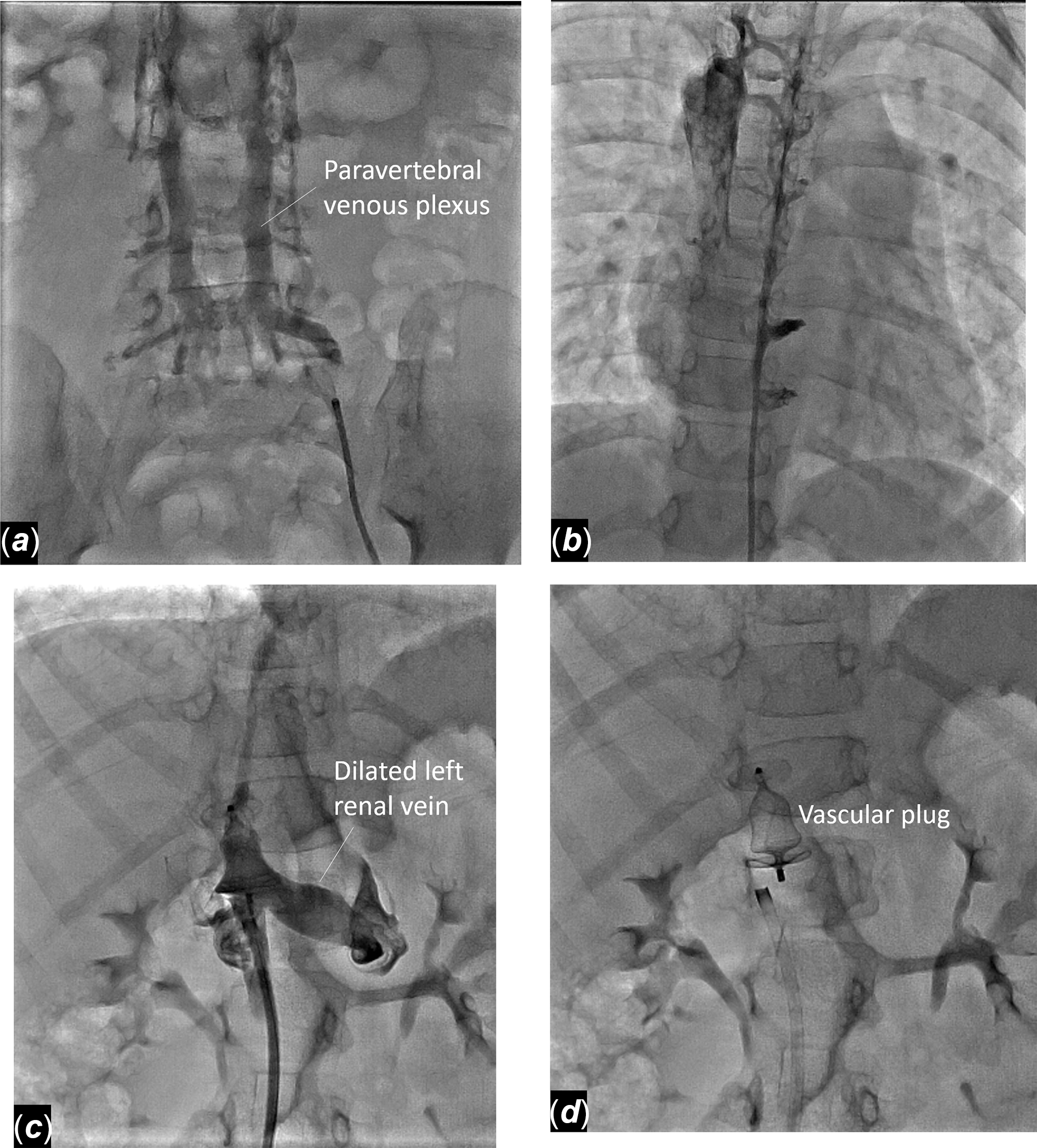
Figure 2. ( a ) Contrast injection in left common femoral vein showing filling of paravertebral venous plexus. ( b ) Contrast injection in paravertebral venous plexus showing drainage into superior caval vein through azygos vein.
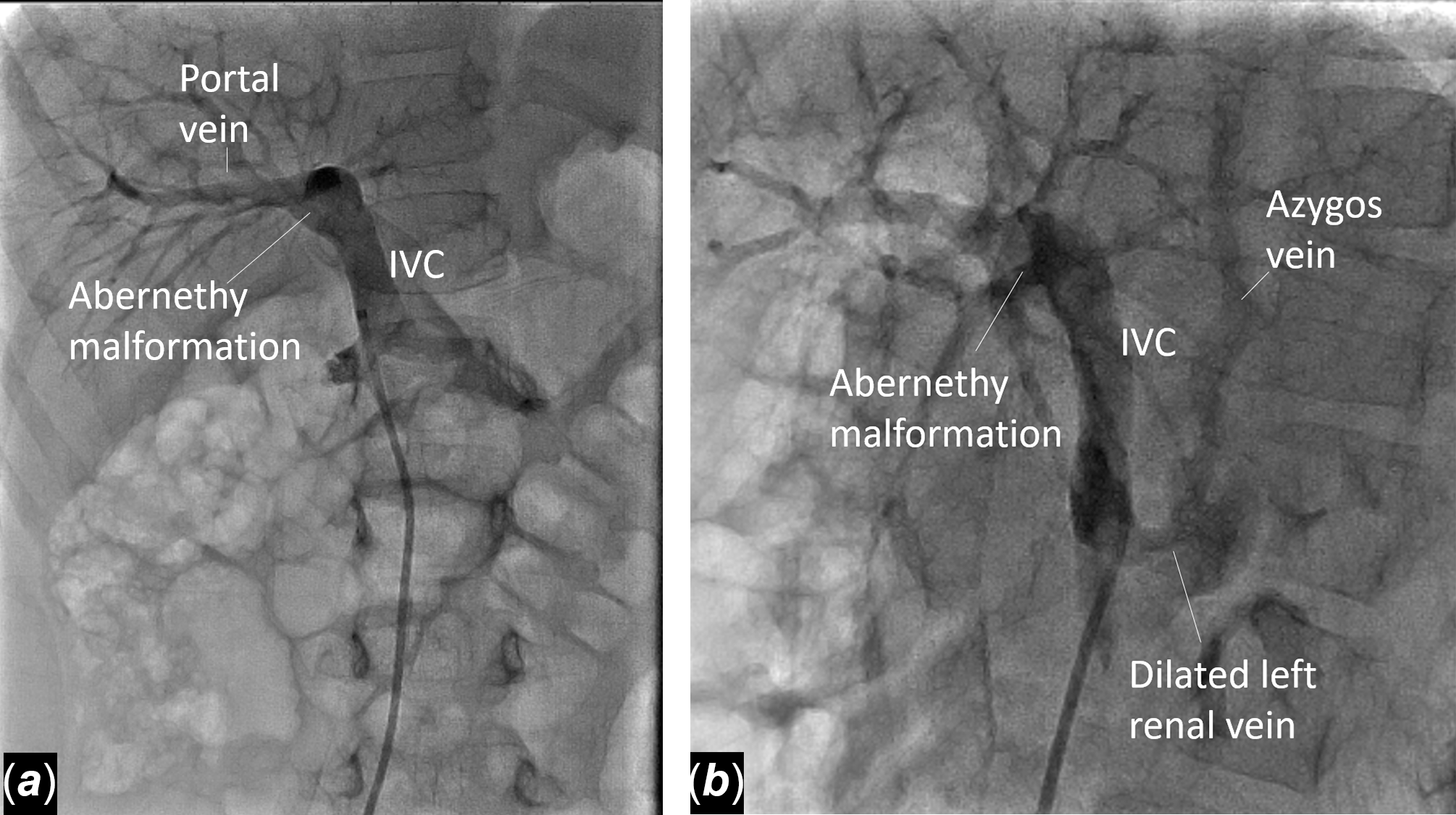
Figure 3. Angiogram in the infrahepatic IVC in AP ( a ) and lateral ( b ) views profiling the portosystemic communication and filling of portal radicals, which appear adequate even without balloon occlusion test. ( c ) Angiogram in the infrahepatic IVC with AVP-II 14-mm device in the Abernethy malformation showing absence of flow into portal system; device extends into the infrahepatic IVC; there is no filling of portal radicals. ( d ) Image following the release of vascular plug. AP= anteroposterior; AVP= Amplatzer vascular plug; IVC= inferior caval vein.
A 14-mm Amplatzer vascular plug-II was chosen since the dimension of the porto-caval communication was measured as 10 mm. The vascular plug was deployed through a 7Fr Mullins sheath. It was placed such that the distal lobe of the plug was in the bulbous communication and the other two lobes extended into the inferior caval vein, with the intent that the whole length of the plug stayed above the drainage of the left renal vein. However, the device eventually seemed to protrude slightly into the left renal vein without obstruction to flow into the left renal vein (Fig 3c and d; Supplementary video S2). The procedure was successful as the angiogram with the device in the intra-hepatic inferior caval vein showed no residual flow into the portal venous system. Post-procedure, the patient was kept on unfractionated heparin for 24 hours followed by oral anticoagulation with warfarin. He was planned for recatheterisation after 3 months to check pulmonary artery pressure and any obstruction in the flow into the left renal vein due to the device. However, due to the COVID-19 pandemic, follow-up has not been possible. On telephonic communication with the patient’s father, the patient is doing well without any symptoms of portal hypertension.
Discussion
Abernethy malformation has been described in association with inferior caval vein anomalies. Reference Xie, Li, Jiang, Zhao and Xiao3 Most such cases are associated with polysplenia syndrome. Reference Sheth and Sivakumar4 This report describes a child with this association in the absence of polysplenia and CHD. The embryological basis for this association is right-sided venous hypoplasia or agenesis involving both the vitelline (portal) and subcardinal (infrahepatic caval vein) venous systems. Right vitelline vein hypoplasia with poor portal arborisation in the liver leads to shunting of portal blood into the systemic vein. Right subcardinal aplasia results in inferior caval vein interruption. Reference Sheth and Sivakumar4 The right venous hypoplasia may occur as an isolated lesion or may be part of a more generalised left isomerism with co-existing cardiac malformations. Reference McElhinney, Marx and Newburger5
In the usual form of interruption of inferior caval vein, the infrahepatic inferior caval vein continues as the azygos vein. However, the systemic venous anomalies may be more complex. Absence of direct communication between the inferior caval vein and azygos system with a connection between the two systems via vertebral plexus and ascending lumbar veins have also been described. Reference van der Horst and Hastreiter6 In our case, the azygos vein arose from the left renal vein and coursed along on the right side. Apart from this, the left common femoral vein was draining into the vertebral venous plexus and there were multiple venous collaterals related to venous thrombosis. This unusual venous anatomy led to initial difficulty in reaching the communication from the left femoral vein approach. However, we could reach the inferior caval vein and the portosystemic shunt from the right femoral venous access. The demonstration of adequate portal vein hepatic ramification and normal portal pressure with balloon occlusion test before device closure of the portosystemic shunt is widely practised. Reference Venkateshwaran, Krishnamoorthy and Sivasankaran7 However, in our case, good-sized portal radicals were demonstrated on the initial angiogram without a balloon occlusion test. The intrahepatic interruption of inferior caval vein did not pose difficulty because the area of interest was below the level of interruption. In fact, due to the interruption of inferior caval vein above the portosystemic shunt, the device could protrude in part of inferior caval vein as long as it stayed above the dilated left renal vein. A similar case has been reported in a 5-year-old child, where a covered stent has been used to close Abernethy malformation associated with hypoplasia of inferior caval vein. Reference Sheth and Sivakumar4 Vascular plug, which is much less expensive and is not constrained by the growth of the child, was considered ideal for our patient.
Conclusion
Abernethy malformation may be rarely associated with interrupted inferior caval vein and other systemic venous anomalies in the absence of polysplenia and CHD. In such cases, the malformation can be successfully closed after defining the venous anomaly in detail.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951121002900.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.






