Truncus arteriosus communis is a rare cyanotic CHD with an incidence of 6–10/100,000 live births, representing only 0.7% of all congenital heart lesions.Reference Reller, Strickland and Riehle-Colarusso 1 It is a conotruncal heart defect, where the embryological conotruncus is undivided with a lack of the aorticopulmonary septum; the developmental arrest occurs around the 32nd day (Carnegie State 14) of embryological development.Reference Yu and Hutchins 2 , Reference Van Praagh and Van Praagh 3 Other associated findings are common and usually include a ventricular septal defect and truncal valve (bicuspid/quadricuspid) and aortic arch abnormalities such as right, interrupted, and hypoplastic aortic arch. In addition, it is associated with coronary artery abnormalities, an aberrant subclavian artery, and a persistent left superior vena cava draining into the coronary sinus.
Cor triatriatum sinistrum is another rare cardiac malformation with a prevalence of 0.6/100,000 live births.Reference Samanek and Voriskova 4 There are two types of cor triatriatum, and the left-sided variant is more common than the right-sided variant. The membrane of cor triatriatum sinistrum separates the left atrium into an upper chamber – embryonic common pulmonary vein – containing the pulmonary veins and a lower chamber – embryonic left atrium – leading to the mitral inflow tract, thereby including the left auricular appendage. The separation occurs around the 33rd day (Carnegie State 14) of embryological development.Reference Goel, Saxena and Kothari 5 Associated cardiac lesions are seen in 75% cases, including anomalous pulmonary venous drainage, patent ductus arteriosus, ventricular septal defect, and coarctation of the aorta. In addition, cor triatriatum has been reported with tetralogy of Fallot, atrioventricular septal defect,Reference Hall, Hislop and Haworth 6 congenitally corrected transposition of great arteries,Reference Gupta, Saxena, Ramakrishnan, Juneja and Devagourou 7 and transposition of great arteries.Reference Litovsky, Ostfeld, Bjornstad, Van Praagh and Geva 8
In this case report, we present the combination of these two rare CHDs. To our knowledge, this combination has never been described before.
Case report
Patient
A 3-month-old female child presented to our hospital with mild cyanosis since early infancy. The mother denied former chest infections and feeding difficulties during early childhood; however, she noticed exertional shortness of breath during screaming episodes.
There was mild cyanosis and the saturation by pulse oximetry was 90%; there was mild tachycardia (heart rate at 158/minute), a normal loud first and second heart sound. A grade 3/6 systolic murmur was audible over the cardiac apex. Mild tachypnoea was present, but the lungs were normally ventilated, and there was mild hepatomegaly.
Diagnostics
The chest radiograph demonstrated moderate cardiomegaly and signs of increased pulmonary blood flow. An electrocardiogram showed normal sinus rhythm, QRS axis of −30°, and biventricular hypertrophy.
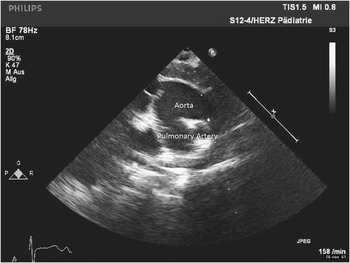
The transthoracic echocardiogram revealed situs solitus, levocardia, and atrioventricular and ventriculoarterial concordance. Furthermore, a typical cor triatriatum sinistrum was detected (Fig 1) with an opening of 3 mm, and a mildly obstructed blood flow of maximum 1.4 metres per second. At the level of the great vessels, a truncus arteriosus communis type A1 (Fig 2), with a main pulmonary artery arising from the left side of the truncal root, was seen. In addition, an anomalous pulmonary venous drainage of the upper right pulmonary vein to the right atrium could be diagnosed.

Figure 1 Echocardiographic sub-costal view at the artrial level: cor triatriatum sinistrum with moderately obstructed blood flow in the colour duplex mode.

Figure 2 Echocardiographic parasternal short-axis view: the truncal root with the origin of the aorta and pulmonary trunk, truncus arteriosus communis type A1.
Surgical management
The child underwent total surgical correction. The ventricular septal defect was closed using a bovine pericardial patch. The reconstruction of the right ventricular outflow tract was accomplished with a 12-mm bovine jugular vein. The cor triatriatum was confirmed intra-operatively and the membrane in the left atrium was resected. The upper right pulmonary vein was re-routed to the left atrium using an autologous pericardial patch.
The post-operative outcome was uneventful. Post-operative echocardiogram confirmed an excellent post-operative result. The child was discharged on the 10th post-operative day in stable condition.
Discussion
To the best of our knowledge, this is the first report of an association between the two rare cardiac malformations – truncus arteriosus communis and cor triatriatum sinistrum.
In the literature, there are many reports with the combination of truncus arteriosus communis and anomalies of the pulmonary veins.Reference Berdjis, Wells and Starnes 9 , Reference Van Praagh and Corsini 10 The cor triatriatum sinistrum may be regarded as a special embryological variation of the development of the pulmonary veins, as the membrane separating the atrium develops as an incomplete regression from the embryologic junction of the heart and the pulmonary veins.Reference Ma, Yang, Zhong and Xiao 11
In addition, there are only few reports about the association of cor triatriatum sinistrum with other conotruncal defects such as tetralogy of Fallot or transposition of the great arteries.Reference Gupta, Saxena, Ramakrishnan, Juneja and Devagourou 7 , Reference Litovsky, Ostfeld, Bjornstad, Van Praagh and Geva 8 , Reference Campbell and Hutchins 12 The truncus arteriosus is another conotruncal defect based on the absence of the pulmonary infundibulum.Reference Van Praagh and Van Praagh 3
To explain the embryological aspect and the development of this rare combination, we can assume that there is a disturbance in the conotruncal and the inter-ventricular septum in addition to a defect in the process of merging of the pulmonary veins to the left atrium. Both these developments occur around the 32nd day of embryological development, and therefore a timing coherence exists. In conclusion, this seems a remarkable coincidence without a known causative context.
Acknowledgement
None.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.