Hypoplastic left heart syndrome occurs between 0.016 and 0.036% of live births and traditionally has accounted for a disproportionate number of cardiac deaths during the first weeks to months of life.Reference Morris, Outcalt and Menashe1 Fortunately, a combination of fetal diagnosis, improved pre-operative care, early repair with improved surgical experience, and increased monitoring both while inpatient and outpatient have made a substantial impact on survival, with recent centres reporting survival to stage 2 palliation between 85 and 96%.Reference Sathanandam, Philip and Gamboa2,Reference Hoque, Richmond and Vincent3 For the 5–10% of patients who have an intact or severely restrictive atrial septum, however, morbidity and mortality remain unacceptably high.
In the setting of hypoplastic left heart syndrome, an atrial septal communication allows for decompression of blood returning from the lungs. In contrast, an intact septum allows no outlet for blood from the left side of the heart, which leads to significant elevation in pulmonary arterial and venous pressures, severely dilated lymphatics and “arterialisation” of pulmonary veins.Reference Graziano, Heidelberge and Ensing4,Reference Rychik, Rome and Collins5 If present, dilated lymphatics can be effectively identified using fetal MRI. The limited reports thus far suggest that patients with prenatally diagnosed pulmonary lymphangiectasia have nearly universal mortality.Reference Seed, Bradley and Bourgeois6,Reference Saul, Degenhardt and Iyoob7 At worst, these changes contribute to the common postnatal presentation of severe hypoxemia, haemodynamic instability, and death. At best, they may cause permanent changes to the pulmonary vasculature that put these patients at higher risk for early mortality compared to their counterparts with adequate atrial mixing.
The purpose of this retrospective study is to add our centre’s experience to the growing body of literature describing the diagnosis and management strategies for patients with hypoplastic left heart and intact atrial septum and to describe our experience with both pulmonary venous Doppler flow patterns on fetal echocardiography and fetal MRI as predictors for morbidity and mortality.
Materials and methods
Study population
Approval of this study was obtained through the Indiana University School of Medicine Institutional Review Board. By searching our surgical and echocardiographic databases, we retrospectively identified all patients that presented to Riley Hospital for Children at Indiana University Health with a diagnosis of hypoplastic left heart syndrome between 1 January, 2009 and 6 October, 2017. In accordance with other recently published experiences, hypoplastic left heart syndrome was defined as having mitral atresia and aortic atresia, aortic atresia and mitral stenosis, or aortic stenosis and mitral stenosis associated with hypoplasia of the left ventricle. Patients with additional cardiac defects, including unbalanced atrioventricular canal, double-outlet right ventricle, or isolated critical aortic stenosis were excluded, as were patients with underlying chromosomal syndromes or non-cardiac malformations that could potentially affect outcomes. We divided our cohort into two groups. Group 1 included patients with an adequate inter-atrial communication, while Group 2 included patients with an intact or severely restrictive inter-atrial communication. The foramen ovale was considered intact if there was a) no visible defect in the atrial septum by two-dimensional fetal echocardiography and b) no colour flow across the atrial septum using Doppler colour flow mapping. It was considered restrictive if the infant required left atrial decompression within the first 24 hours of life, regardless of gradient across the atrial communication obtained by echocardiography. The primary outcome was survival to stage 2 palliation. Death was defined as true death of the patient or any patient who received heart transplantation secondary to haemodynamics or poor heart function that prohibited continuation of the palliative surgical pathway.
Postnatal intervention
Postnatal intervention was defined as any surgical or catheterisation-based intervention completed in the first 24 hours of life aimed at decompressing the left atrium to allow for unobstructed blood flow to the right side of the heart. Left atrial decompression was planned if there was concern for an intact atrial septum or concerning pulmonary vein Doppler pattern on fetal echocardiography. Unplanned postnatal intervention was performed for those patients who had clinical signs or symptoms of cardiac failure and an inadequate atrial level shunt. The decision to proceed with left atrial decompression was based on clinical judgement of the team and took into consideration systemic oxygen saturation, lactate levels, pH, chest x-ray findings, need for respiratory support, postnatal echo findings including the size of the atrial septal defect and gradient from left to right atrium, and clinical exam findings suggestive of low cardiac output despite adequate medical intervention.
Re-intervention
Re-intervention was defined as any unplanned surgical or catheterisation-based procedure between stage 1 palliation and stage 2 palliation, including intervention to improve patency of an atrial septal defect, patent ductus arteriosus, Blalock–Taussig shunt, or aortic arch.
Fetal imaging
Fetal echocardiogram
Fetal echocardiograms were performed using accepted standards and included two-dimensional, colour flow, and Doppler assessment. The atrial septum was carefully evaluated for evidence of an atrial septal communication by two-dimensional and colour Doppler. The Doppler flow pattern in the pulmonary vein was obtained with the sample volume placed at the insertion of either the left or right pulmonary vein into the left atrium, as described previously.Reference Better, Apfel and Zidre8 The ratio of the forward to reverse velocity time integral was calculated (Fig 1). Pulmonary vein Doppler patterns were classified based on previously described reportsReference Taketazu, Barrea and Smallhorn9 (Fig 2). If multiple fetal echocardiograms were obtained, only the most recent pulmonary vein Doppler pattern prior to delivery was used.

Figure 1. A normal pulmonary vein Doppler pattern is demonstrated. The S wave occurs during early ventricular systole and is caused by the “sucking effect” of atrial relaxation. The D wave occurs during the early diastolic ventricular phase and represents forward flow across the mitral valve. The A wave occurs during atrial systole and there is typically cessation of flow or very mild flow reversal. The second panel shows a sample tracing of forward velocity time integral (FVTI) and reverse velocity time integral (RVTI).

Figure 2. Types of fetal pulmonary vein Doppler patterns. Type A pattern consists of primarily forward flow with a forward/reverse VTI > 3. Type B pattern maintains primarily forward flow but with an increased A-wave velocity, and therefore a forward/reverse VTI < 3. Type C pattern consists of loss of primarily forward flow and a “to-and-fro” flow pattern with minimal or no early ventricular diastolic flow.
Fetal MRI
At the time that these patients were born, there was no specific protocol for the use of fetal MRI. The decision to obtain an MRI was based on the suggestion of the medical care providers on the team. MRI was performed on a 3-T Skyra MR scanner (Siemens Healthineers, Erlangen, Germany). The women were positioned the supine position with a partially full urinary bladder. Half-acquisition single-shot fast spin-echo, steady-state free precession, T1-spoiled 3-D gradient, and gradient echo images were obtained of the fetal thorax in the axial, sagittal, and coronal planes. The scanning time/slice was less than 1 slice/image, and the entire MRI study was completed within 45 minutes. No contrast media was used. MRI images were reviewed by two independent paediatric radiologists. The presence of lymphangiectasia was defined as serpiginous, branching hyperintense dilated lymphatics radiating out from the hilum, as seen in Figure 3.
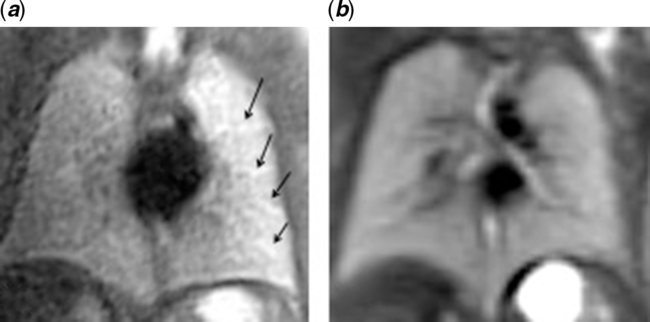
Figure 3. (a) Demonstrates MRI imaging of fetal lungs at 25 weeks in a patient with known hypoplastic left heart syndrome/IAS and (b) demonstrates the lungs from an unrelated, normal fetal MRI at 25 weeks.
Statistical analysis
Group 1 and Group 2 were compared for differences using Fisher’s exact tests for categorical variables and Wilcoxon rank-sum tests for continuous variables. Comparisons among the three fetal pulmonary vein Doppler patterns were made using Fisher’s exact tests for categorical variables and Kruskal–Wallis tests for continuous variables. A 5% significance level was used for all tests. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Demographics
Over a 7.9-year period, there were 81 neonates that met our inclusion criteria with hypoplastic left heart syndrome. Twelve (15%) had an intact or severely restrictive atrial septum and 69 (85%) had an adequate atrial septal defect. Prenatal diagnosis was available for 47 (68%) of those born with an adequate atrial septal defect. All 12 patients with an intact/restrictive atrial septum were diagnosed prenatally. For one neonate in Group 2, the parents initially chose to undergo comfort care without planned intervention at their local hospital. At 10 hours of life, however, the mother requested that the patient be transferred to the tertiary care centre and that all measures be attempted to maintain life. Another neonate in Group 2 did not have surgical intervention secondary to parental choice to undergo comfort care. The demographics of the patients in both groups as well as the interventions and outcomes are detailed in Tables 1 and 2. A detailed look at each patient in Group 2 can be seen in Table 3. Patients in Group 1 were significantly more likely to have fetal pulmonary vein Doppler pattern A (p < 0.001), significantly less likely to have a fetal MRI (p = 0.008), and had significantly higher forward/reverse velocity time integral.
Table 1. Outcomes and demographics of patients with hypoplastic left heart syndrome and adequate versus intact atrial septum.

DKS = Damus–Kaye–Stansel; ECMO = extracorporeal membranous oxygenation
p-Values are comparing trends between Group 1 and Group 2. For example, when comparing Group 1 and Group 2, there is a statistical difference in the number of patients with type A and type C pulmonary vein Doppler pattern.
Table 2. Outcomes and demographics of patients with hypoplastic left heart syndrome and adequate versus intact atrial septum.

LOS = length of stay; SD = standard deviation; VTI = velocity time integral
Table 3. Outcomes and demographics for patients with hypoplastic left heart syndrome and intact septum.

AA-MA = aortic atresia/mitral atresia; AA-MS = aortic atresia/mitral stenosis; AS-MS = aortic stenosis/mitral stenosis; ball arch = balloon aortic arch; BT = Blalock–Taussig; D = death; DKS = Damus–Kaye–Stansel; Hemi = hemi-Fontan; mPAP = mean pulmonary artery pressure; M = months; N = no; PFO = patent foramen ovale; PVR = pulmonary vascular resistance; sept = septostomy; TV = transvenous; VTI = velocity time integral; Y = yes
No postnatal data are available for the 12th patient who had a type C pulmonary vein Doppler pattern and pulmonary lymphangiectasia on fetal MRI because the parents chose palliative treatment instead of surgical intervention
* PFO gradient for patient 1 appears low, however had a poor Doppler angle and tracing for measurement. The PFO gradient for patient 2 was thought to be small secondary to severely diminished flow across the atrial septum. A Fontan was attempted in patient 4 but needed to be taken down secondary to elevated pulmonary artery pressures post-operatively and Fontan failure
Anatomy
Overall, 41 patients had aortic and mitral atresia, 12 had aortic atresia and mitral stenosis, and 28 had aortic stenosis and mitral stenosis. There were no cases of ventriculo-coronary connections among any anatomical description. The patient that chose palliative care and did not have surgical intervention did not have a postnatal echocardiogram, so confirmation of her exact anatomical diagnosis cannot be reported.
Fetal pulmonary vein Doppler findings
Forty-two of the 81 neonates had at least 1 fetal echocardiogram with adequate pulmonary vein Doppler assessment to review. Overall, 27 patients had a type A pattern, 8 had a type B pattern, and 7 had a type C pattern. No patients with a type A pattern had evidence pulmonary lymphangiectasia, while two patients with a type C pattern had evidence of pulmonary lymphangiectasia by fetal MRI. No patient in Group 2 had a type A pulmonary vein Doppler pattern, while no patient in Group 1 required immediate postnatal intervention. Patients with type A pattern were more likely to have adequate septum (p < 0.001) and more likely to have a standard Norwood operation as their stage 1 palliation rather than a Hybrid procedure (p < 0.001). Patients with type C pattern were less likely to undergo re-intervention (p = 0.023) and had significantly higher age at stage 1 palliation (p = 0.020). Details of demographics and outcomes organised by pulmonary vein Doppler pattern are seen in Tables 4 and 5.
Table 4. Outcomes by pulmonary vein Doppler pattern.

DKS = Damus–Kaye–Stansel; ECMO = extracorporeal membranous oxygenation
Table 5. Outcomes and demographics by pulmonary vein Doppler pattern

LOS = length of stay; mm = millimetres; VTI = velocity time integral
Fetal MRI findings
Only seven patients in this cohort underwent a fetal MRI for interpretation. Five showed no evidence of pulmonary lymphangiectasia, compared to two which did show evidence of lymphangiectasia. Both patients in whom the MRI showed evidence of lymphangiectasia had a type C pulmonary vein Doppler pattern on fetal echocardiogram. Of these two, one family opted for comfort care after birth and the child died. The other patient had a prolonged hospital course consisting of 306 days in the ICU, prolonged intubation, chronic pleural effusions, severe pulmonary hypertension, and eventual demise secondary to pulmonary failure and cardiac arrest. His most recent catheterisation at 6 months of age showed mean pulmonary artery pressure of 32 mmHg and pulmonary vascular resistance of 3.74 units × m2.
Postnatal interventions
Of the 12 patients in Group 2, 4 underwent a planned procedure immediately after delivery. These neonates were all scheduled for a C-section at Riley Hospital for Children at IU Health, underwent immediate postnatal resuscitation, and were transferred to the adjacent operating room for combined intervention with the surgical and catheterisation teams. Three patients underwent limited vertical sternotomy by cardiothoracic surgery, which then allowed for puncture of the atrial septum with a needle and subsequent placement of an atrial septal stent by the cardiac interventionist, as described by Hill et alReference Hill, Fudge and Barker10 One patient had the same procedure completed; however, access was obtained via a subxiphoid approach to avoid having to complete a full sternotomy. Seven patients were born at an outside hospital and were transferred to Riley after being medically stabilised. Six patients underwent a transvenous approach by the cardiac interventionist, of which five had a balloon atrial septostomy and one patient underwent atrial stent placement. One patient had an intact septum but with an unobstructed decompressing vein, which allowed adequate drainage of his pulmonary veins to the right side of his heart and therefore did not require immediate intervention. One family elected to not undergo surgical intervention and instead chose comfort care.
Outcomes
No patient in either group underwent orthotopic heart transplantation as a means for primary treatment. Patients in Group 1 were significantly more likely to have a standard Norwood operation as opposed to a Hybrid procedure (p < 0.001). Overall survival to discharge for Group 1 was 83% compared to 58% for Group 2 (p = 0.116). Survival to stage 2 palliation was 71% for Group 1 compared to 50% for Group 2 (p = 0.186). To date, only 4 of the initial 12 patients from Group 2 are alive, which is an overall survival of 33%.
Discussion
Advances in fetal echocardiography have improved prenatal recognition of the restrictive or intact atrial septum by assessing the morphology of the atrial septum, documenting the gradient across the atrial shunt, and by identifying pulmonary venous Doppler flow patterns that accurately predict severe postnatal pulmonary hypertension and need for emergent atrial septoplasty.Reference Better, Apfel and Zidre8–Reference Javois, Van Bergen and Cuneo12 Early identification allows for proper prenatal counselling and novel multidisciplinary approaches to postnatal management that allow rapid left atrial decompression.Reference Marshall, Levine and Morash13,Reference Tanem, Hill and Rudd14 In addition, it allows for the possibility of early, prenatal intervention and prevention of long-term pulmonary abnormalities. Centres have reported fetal techniques for atrial septoplasty, aortic valvuloplasty, and atrial stent placement with promising but varying results.Reference Donofrio, Moon-Grady and Hornberger15–Reference Chaturvedi, Ryan and Seed18
As the rates of survival for hypoplastic left heart syndrome have increased over the years, more parents are choosing to continue with pregnancy and pursue surgical options. Unfortunately, our institutional experience shows that for those children who have an intact or clinically restrictive atrial septum, survival remains extremely poor. This holds true even for those children who had prenatal diagnosis and planned multidisciplinary intervention to allow atrial decompression immediately after birth. While some studies report improving survival for this population,Reference Tweddell, Hoffman and Mussatto19–Reference Vida, Bacha and Larrazabal22 caution must be taken in interpretation of these results given the wide variation in the definition of “restrictive atrial septum” as well as variation in the definition for “survival.” At the National American Academy of Pediatrics conference in 2018, Tanem et alReference Tanem, Hill and Rudd23 presented their experience with survival after Norwood procedure in high-risk patients, including those with an intact or restrictive septum. They defined a restrictive septum as having a mean echo gradient of >8 mm Hg. However, of the 14 patients that met these criteria, only 3 (21%) needed emergent intervention prior to their initial palliative surgery. If a patient has a gradient across their septum but is clinically stable enough that they do not need an intervention in the first hours of life, then this is likely a different substrate/population than those patients with intact septum or those who are clinically decompensating secondary to lack of cardiac output, and the survival outcomes for these patients should be compared separately. We believe that the currently published data, as well as our data, show that fetal pulmonary vein Doppler patterns can accurately separate these groups of patients. Even within our substrate of patients in Group 2, there appears to be a survival difference between those with type B and type C pulmonary vein Doppler patterns. Only one of six patients with a type C pulmonary vein Doppler pattern is currently alive (now post-Fontan), but he also had a decompressing vein. In contrast, three of the four patients with a type B pulmonary vein Doppler are alive, all of which are now post-Fontan procedure. We believe that with a larger number of patients, these differences would attain statistical significance. The use of MRI to assess for pulmonary lymphangiectasia is novel but exciting. Given the small sample size and lack of consistency with which patients received an MRI, it is difficult for us to draw definitive conclusions on the usefulness of MRI as an adjunct to fetal echocardiography. That being said, our data do suggest and support previous findings that pulmonary lymphangiectasia on MRI may be an ominous sign for patients with hypoplastic left heart syndrome. At the time of this paper, our institutional policy is to obtain a fetal MRI on all single-ventricle patients, especially those who have obstructive left-sided lesions such as an intact or restrictive atrial septum.
Our experience with fetal pulmonary vein Doppler patterns and fetal MRI strengthen the available data for use of these modalities in the risk stratification of patients with hypoplastic left heart syndrome. If a patient has a type A pulmonary vein Doppler pattern and normal lungs on fetal MRI, then he/she will not need emergent atrial decompression, and a standard delivery plan can be implemented. On the contrary, patients who have a type C pulmonary vein Doppler pattern should have multidisciplinary arrangements made so that atrial decompression can be accomplished immediately after birth. While survival for this population is extremely poor and this risk should be relayed to the family prior to surgical intervention, it can be accomplished as long as there is no evidence of pulmonary lymphangiectasia on fetal MRI. Although small, our experience with patients who have a type C pulmonary vein Doppler pattern and pulmonary lymphangiectasia is universally fatal and is consistent with previous reports referenced above.
Patients with a type B pattern remain a challenge for planning postnatal management, as some patients with a type B pulmonary vein Doppler pattern will need emergent septostomy and some will not. In our experience, no patient with a forward/reverse velocity time integral greater than 3.30 on their last fetal echocardiogram needed emergent intervention, suggesting that this may be an appropriate cut-off for planning immediate postnatal intervention (Fig 4). This is also consistent with the American Heart Association statement on the diagnosis and treatment of fetal cardiac disease, which suggests using a forward/reverse cut-off value of less than 3 to modify delivery plans and prepare for urgent intervention on the atrial septum.Reference Donofrio, Moon-Grady and Hornberger24 The difficulty lies in the fact that small changes in measurements of velocity time integral may alter values to be just above or below these cut-off recommendations, making definitive conclusions and decisions challenging. With the addition of other modalities such as fetal MRI and even maternal hyperoxygenation,Reference Szwast, Tian and McCann25 these decisions may become clearer. Additional prospective study of this approach is warranted.

Figure 4. Proposed approach to patients with hypoplastic left heart syndrome. Abbreviations: ASD = atrial septal defect; GA = gestational age; PVD = pulmonary vein Doppler; q4w = every 4 weeks; VTIF/VTIR = velocity time integral forward/velocity time integral reverse.
Three of our four patients who had planned delivery at Riley with immediate atrial decompression passed away during the first year of life and only one patient had adequate lung development and pulmonary artery pressures to attempt stage 2 palliation. Some have suggested that the Hybrid strategy be completed as the initial surgical intervention in this population because it allows time to stabilise the patient, correct any other non-cardiac anomalies, and provide more time for the reactive pulmonary vasculature to recover prior to cardiopulmonary bypass during the Norwood procedure.Reference Venugopal, Luna and Anderson26 In our experience, this strategy did not lead to better survival. While this may be in part due to the infrequency with which we perform the Hybrid procedure, we cannot ignore the possibility that the maldevelopment of the pulmonary vasculature secondary to an intact atrial septum in utero makes any heroic intervention unlikely to succeed, especially if pulmonary lymphangiectasia is present. The Mayo clinic recently reported an attempted ex utero intrapartum treatment procedure to surgical septectomy, while the fetal-placental circulation was maintained for a patient with hypoplastic left heart syndrome/intact atrial septum (IAS) and fetal hydrops.27 While this avoided the need for extracorporeal membranous oxygenation and allowed for successful septectomy prior to the neonate’s first breath, the infant did eventually need extracorporeal membranous oxygenation secondary to severe pulmonary hypertension and passed away on the 9th day of life.
In conclusion, pulmonary venous Doppler patterns on fetal echocardiogram can be used effectively to determine which patients with hypoplastic left heart syndrome will need emergent atrial decompression. Fetal MRI can be done safely and effectively and adds prognostic information that is useful for both parents and practitioners when deciding on management strategies. Although more data are needed, offering surgical treatment for the population of patients with both type C Doppler pattern and pulmonary lymphangiectasia may be futile, and we feel that comfort care should be discussed with the family and strongly considered.
Financial support
No funding was received for this study.
Conflict of interest
Ryan Serrano declares that he has no conflict of interest. Sabena Hussain declares that she has no conflict of interest. Brandon Brown declares that he has no conflict of interest. Eric Ebenroth declares that he has no conflict of interest. Anne Farrell declares that she has no conflict of interest.
Ethical approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees.











