Introduction
Although most individuals who sustain a concussion or mild traumatic brain injury (mTBI) make a rapid and complete recovery, a small subset present with incomplete and/or prolonged recovery (Iverson, Reference Iverson2005). The persistence of cognitive, physical, and/or emotional symptoms following mTBI has been described as post-concussion syndrome (PCS), but there has been debate regarding the validity of this diagnosis. PCS symptoms are non-specific to head injury, particularly after the acute recovery period (e.g., Ponsford et al., Reference Ponsford, Cameron, Fitzgerald, Grant, Mikocka-Walus and Schonberger2012; McNally et al., Reference McNally, Bangert, Dietrich, Nuss, Rusin, Wright and Yeates2013), and occur frequently in trauma control, psychiatric, and healthy populations without mTBI (e.g., Boake et al., Reference Boake, McCauley, Levin, Pedroza, Contant, Song and Diaz-Marchan2005; Donnell, Kim, Silva, & Vanderploeg, Reference Donnell, Kim, Silva and Vanderploeg2012; Garden & Sullivan, Reference Garden and Sullivan2010; Julien et al., Reference Julien, Tinawi, Anderson, Frenette, Audrit, Ferland and De Guise2017; Meares et al., Reference Meares, Shores, Taylor, Batchelor, Bryant, Baquley and Marosszeky2011; Wäljas et al., Reference Wäljas, Iverson, Lange, Hakulinen, Dastidar, Huhtala and Öhman2015).
Research has reinforced the importance of non-injury factors in predicting mTBI recovery, with psychological functioning particularly implicated in the maintenance of and resilience against chronic mTBI symptoms (e.g., Silverberg et al., Reference Silverberg, Gardner, Brubacher, Panenka, Li and Iverson2015). For example, prolonged mTBI symptom recovery has been linked with pre-injury psychiatric history (Meares et al., Reference Meares, Shores, Taylor, Batchelor, Bryant, Baquley and Marosszeky2008; Ponsford et al., Reference Ponsford, Cameron, Fitzgerald, Grant, Mikocka-Walus and Schonberger2012), acute emotional distress after injury (Meares et al., Reference Meares, Shores, Taylor, Batchelor, Bryant, Baquley and Marosszeky2008, Reference Meares, Shores, Taylor, Batchelor, Bryant, Baquley and Marosszeky2011; Dischinger, Ryb, Kufera, & Auman, Reference Dischinger, Ryb, Kufera and Auman2009), and concurrent emotional distress at follow-up (Lange, Iverson, & Rose, Reference Lange, Iverson and Rose2011; Lange et al., Reference Lange, Brickell, French, Ivins, Bhagwat, Pancholi and Iverson2014). Broshek and colleagues’ (Reference Broshek, De Marco and Freeman2015) review of PCS and psychological correlates further highlights the influence of anxiety sensitivity, coping style, cognitive misattributions, and injury expectations in mTBI recovery. PCS has also been described as resembling somatoform disorder (e.g., Donnell et al., Reference Donnell, Kim, Silva and Vanderploeg2012; McCrea, Reference McCrea2007) and pre-injury somatization has been shown to predict mTBI symptom recovery indirectly through enhancement of acute post-concussive symptoms (Nelson et al., Reference Nelson, Tarima, LaRoche, Hammeke, Barr, Guskiewicz and McCrea2016). Additionally, emerging work in positive psychology has identified associations between resiliency, positive coping, and better outcomes following diverse acquired brain injuries (Neils-Strunjas et al., Reference Neils-Strunjas, Paul, Clark, Mudar, Duff, Waldron-Perrine and Bechtold2017). This trend holds for mTBI specifically (Sullivan, Kempel, Edmed & Bonanno, Reference Sullivan, Kempel, Edmed and Bonanno2016), including research demonstrating that resiliency is inversely associated with chronic mTBI symptoms (Losoi et al., Reference Losoi, Silverberg, Wäljas, Turunen, Rosti-Otajärvi, Helminen and Iverson2015; Merritt, Lange, & French, Reference Merritt, Lange and French2015).
Moreover, despite general consensus among researchers and clinicians that personality appears important to mTBI recovery (e.g., Kay, Newman, Cavallo, Ezrachi, & Resnick, Reference Kay, Newman, Cavallo, Ezrachi and Resnick1992; Evered, Ruff, Baldo, & Isomura, Reference Evered, Ruff, Baldo and Isomura2003), personality aspects of psychological functioning have been investigated minimally in mTBI research (e.g., Broshek et al., Reference Broshek, De Marco and Freeman2015). Few studies have evaluated a comprehensive set of personality and psychiatric dimensions in a single sample, thus enabling a head-to-head comparison of the independent versus overlapping predictive value of distinct constructs. There is also sparse research addressing the potential for moderating relationships between maladaptive and resilient personality traits and/or establishing how personality affects symptom duration through mediating variables, such as acute emotional response to injury. Broad personality dimensions, such as those in the Five Factor Model (FFM), are attractive prognostic variables because they are widely identified across cultures (McCrae, Costa, del Pilar, Rolland, & Parker, Reference McCrea, Costa, del Pilar, Rolland and Parker1998; Yamagata et al., Reference Yamagata, Suzuki, Ando, Ono, Kijima, Yoshimura and Jang2006), can be measured efficiently and reliably, have strong predictive value for other health and life outcomes (Israel et al., Reference Israel, Moffitt, Belsky, Hancox, Poulton, Roberts and Caspi2014; Smith, Reference Smith2006), and provide a behavioral window into someone’s underlying neurobiology. As the structure and neurobiological underpinnings of personality traits are increasingly understood (DeYong & Gray, Reference DeYong, Gray, Corr and Matthews2009; Perez-Rodriguez, Zaluda, & New, Reference Perez-Rodriguez, Zaluda and New2013), identifying which traits predict mTBI outcomes may help develop hypotheses around the neurobiological mechanisms by which pre-injury factors effect response to injury, providing a steppingstone toward a more comprehensive biopsychosocial model of individual differences in mTBI outcomes.
The aim of this study was to evaluate to what extent self-report measures of diverse personality dimensions predict chronic mTBI symptoms in a civilian trauma sample. Patients with mTBI were recruited acutely post-injury during hospital admission and completed standardized measures of personality traits and acute injury symptoms. Following a common convention in research (e.g., Meares et al., Reference Meares, Shores, Taylor, Batchelor, Bryant, Baquley and Marosszeky2011) and clinical practice (e.g., DSM-IV postconcussional disorder; American Psychiatric Association, 1994), we defined “chronic” mTBI symptoms as symptom severity at 3 months post-injury. Our primary hypotheses were that (1) maladaptive personality traits (e.g., negative affect) are negatively associated with mTBI symptom recovery and (2) adaptive personality traits (e.g., positive emotionality) are positively associated with mTBI symptom recovery, perhaps moderating the relationship between maladaptive traits and recovery. Interested in gaining insight into how pre-injury personality influences mTBI recovery, we also compared indirect (mediation) and conditional effects (moderated mediation) models to test the preliminary hypothesis that (3) personality traits predict symptom recovery indirectly via effects on acute injury response. Because “post-concussive” symptoms are not unique to individuals with mTBI, path models were secondarily evaluated in an orthopedic trauma control (OTC) sample to inform the degree to which personality-outcome associations are specific to brain-injured patients.
Method
Participants
Patients were screened for study inclusion/exclusion criteria using a real-time list of all hospitalized trauma patients. Reasons for admission were unavailable, but typical reasons in this setting included positive head CT (in the case of mTBI) and/or sufficient peripheral injury to warrant admission. Of the 1419 screened between April 2015 and March 2016, 464 appeared eligible and were approached for further screening; 155 met study inclusion criteria and consented to participate (75 mTBI and 79 OTC without mTBI). The current study focuses on data from the mTBI group for primary analyses; the OTC were included for comparison with mediation modeling. Sample demographic and injury characteristics are in Table 1 (see Results).
Table 1. Sample demographics, injury characteristics, and symptom presentations

Note. Acute assessments unless otherwise noted. OTC = orthopedic trauma controls; WRAT = Wide Range Achievement Test (SS); SCAT = Sport Concussion Assessment Tool 3/5 (raw score total); BSI-18 = Brief Symptom Inventory-18 (T); MMPI-2-RF = Minnesota Multiphasic Personality Inventory-2-Restructured Form (T); SS = Standard Score (M = 100, SD = 15). T scores (M = 50, SD = 10).
*Significant group differences for total sample but not follow-up sample. **Significant group differences for total sample and follow-up sample.
a Combined yes (witnessed) and suspected (self-reported, unwitnessed) categories.
For inclusion, patients had to be age 18 years or older, English speaking, admitted within the previous 10 days for a traumatic injury and, for the mTBI group, meeting the American Congress of Rehabilitation Medicine’s definition of mTBI: A traumatically-induced physiological disruption of brain function, manifested by at least one of the following: loss of consciousness (LOC; < 30 minutes), memory loss for the events before or after (post-traumatic amnesia; PTA) injury (< 24 hours PTA), or other evidence of alteration of mental state immediately post-injury; or documentation of focal neurologic deficit after trauma; as well as initial Glasgow Coma Scale (GCS) score ≥ 13 (Kay et al., Reference Kay, Harrington, Adams, Anderson, Berrol, Cicerone and Malec1993). Common exclusions included an injury being outside the target (10-day) window, GCS score < 13, dementia, and non-English speaking. Persons who were incarcerated or unable to consent (e.g., activated power of attorney for healthcare) were also excluded. Study procedures were approved by the Medical College of Wisconsin IRB.
Study Protocol
Acute assessment
After obtaining informed consent, research staff conducted a bedside clinical assessment (median = 2 days after injury; range = 0–12 days) during each participant’s hospital admission (“Acute” timepoint) collecting demographics, self-report personality and symptom scales, and neurocognitive testing using the Wide Range Achievement Test-4 (WRAT-4) Word Reading subtest (Wilkinson & Robertson, Reference Wilkinson and Robertson2006), Hopkins Verbal Learning Test-Revised (Benedict, Schretlen, Groninger, & Brandt, Reference Benedict, Schretlen, Gronginger and Brandt1998), Oral Digit Symbol Modalities Test (Smith, Reference Smith1982), and Wechsler Adult Intelligence Scale-III Digit Span subtest (Wechsler, Reference Wechsler1997). Additional demographic, medical history, and treatment information was extracted from electronic medical records. Participants were read questionnaires by the examiner if they achieved less than a 6th grade estimated reading level on WRAT-4 Word Reading, requested that items be read to them, or if the examiner had concerns about their ability to complete questionnaires independently. Overall, 52% had all questionnaires read to them and 26% had a portion of questionnaires read to them.
Follow-up assessments
Participants were contacted by phone at 1 month and 3 months after injury to administer select questions focused on symptom recovery, including the SCAT. The 3-month (“Chronic”) assessment was the focus of this study.
Measures
The Sport Concussion Assessment Tool – 3rd/5th edition symptom checklist (SCAT3/5, referred to herein as the SCAT; Guskiewicz et al., Reference Guskiewicz, Register-Mihalik, McCrory, McCrea, Johnston, Makdissi and Meeuwisse2013; McCrory et al., Reference McCrory, Meeuwisse, Aubry, Cantu, Dvorak, Echemendia and Turner2013) was used to assess mTBI symptoms at each timepoint. The SCAT comprises 22 common concussion symptoms (e.g., headache, dizziness, confusion, irritability), each rated on a seven-point Likert scale (0 = none to 6 = severe) that are summed to yield a symptom severity score (range 0–132). Acute general distress was assessed with the 18-item Brief Symptom Inventory (BSI-18; Derogatis, Reference Derogatis2001), which contains six-item subscales of Depression, Anxiety, and Somatization symptoms that comprise a Global Severity Index (GSI); items are rated on a five-point Likert scale (0 = not at all to 4 = extremely) and T scores are obtained for subscales and GSI. Acute symptoms were also assessed with the select administration of the Somatic Complaints (RC1) and Low Positive Emotions (RC2) Restructured Clinical scales of the Minnesota Multidimensional Personality Inventory – 2 Restructured Form (MMPI-2-RF; Ben-Porath & Tellegen, Reference Ben-Porath and Tellegen2008); these scales contain 27 and 17 true-false items, respectively, and T scores are obtained.
Measures of personality included an abbreviated version of the Multidimensional Personality Questionnaire (MPQ; Patrick, Curtin & Tellegen, Reference Patrick, Curtin and Tellegen2002). The 29-item version we used was derived from the 35-item MPQ, which was developed for a large epidemiologic study to efficiently assess the higher order constructs of negative emotionality (NEM), positive emotionality (PEM), and constraint (MIDUS, 2018). We used MPQ to assess NEM and PEM, which reflect temperaments and tendencies to experience negative or positive emotions, respectively. Negative affect is associated with distress and unpleasant mood states, such as anxiety and anger, and positive affect is associated with positive engagement, enthusiasm, and well-being (e.g., Patrick, Curtin, & Tellegen, Reference Patrick, Curtin and Tellegen2002; Watson, Clark, & Tellegen, Reference Watson, Clark and Tellegen1988). NEM (10 true-false items) and PEM (15 true-false items) subscales were computed as mean standardized domain scores (Z) obtained from the lower-order domain scores for each of these two higher-order dimensions (NEM: stress reaction, alienation, aggression; PEM: well-being, social potency, well-being, social closeness). PEM was used as a proxy of adaptive/resilient personality.
The 11-item Disinhibition scale was used (DIS-11, derived from the Externalizing Spectrum Inventory), which is designed to measure trait propensity toward disinhibitory pathology (Krueger, Markon, Patrick, Benning, & Kramer, Reference Krueger, Markon, Patrick, Benning and Kramer2007); items are rated on a four-point scale from 0 to 3 (response options: true, somehwat true, somewhat false, and fase), and a mean item score is obtained. The Personality Disorder Inventory for DSM-5 – Brief Form (PID-5-BF; Krueger, Derringer, Markon, Watson, & Skodol, Reference Krueger, Derringer, Markon, Watson and Skodol2012) was used to measure five broad maladaptive personality traits (i.e., negative affect, detachment, antagonism, disinhibition, psychoticism); each scale comprises five items rated on a four-point scale from 0 to 3 (response options: very false or often false, sometimes or somewhat false, sometimes or somewhat true, and very true or often true), and mean item scores are obtained. The PID-5 was created to guide the development of a personality traits model for DSM-5, capture dimensions of maladaptive personality previously identified, and ensure the poles of these trait dimensions adequately reflected personality disorder pathology outlined in DSM-IV (American Psychiatric Association, 1994; Krueger et al., Reference Krueger, Derringer, Markon, Watson and Skodol2012). The PID-5 measures 25 lower-order facets which, per Krueger and colleagues (Reference Krueger, Derringer, Markon, Watson and Skodol2012), reflect five higher-order dimensions of (1) negative affect (reflecting anxiousness, emotional lability, hostility, perseveration, an absence of restricted affectivity, separation insecurity, and submissiveness), which corresponds with FFM trait neuroticism; (2) detachment (reflecting anhedonia, depressivity, intimacy avoidance, suspiciousness, and withdrawal), which corresponds with low levels of FFM extroversion; (3) antagonism (reflecting attention seeking, callousness, deceitfulness, grandiosity, and manipulativeness), which corresponds with low levels of FFM agreeableness; (4) disinhibition (reflecting distractibility, impulsivity, irresponsibility, absence of rigid perfectionism, and risk taking), which aligns with low levels of FFM conscientiousness; and (5) psychoticism (reflecting eccentricity, cognitive and perceptual dysregulation, and unusual beliefs and experiences). PID-5 Psychoticism has no FFM counterpart but is akin to psychoticism from Harkness’ Personality Psychopathology 5 (PSY-5) model of clinically relevant personality traits (Harkness, McNulty, & Ben-Porath, Reference Harkness, McNulty and Ben-Porath1995; Krueger et al., Reference Krueger, Derringer, Markon, Watson and Skodol2012).
The Injury Severity Score (Baker, O’Neill, Haddon, & Long, Reference Baker, O’Neill, Haddon and Long1974), extracted from the hospital trauma registry, was used to assess the severity of all injuries participants sustained.
Data Analyses
Descriptive statistics were used to examine the demographics, injury parameters, and self-report personality and symptom scales of the mTBI (n = 75) and OTC (n = 79) samples. Chi-square analyses, likelihood ratio tests, and t-tests were used to compare the groups on key variables. Our primary analyses emphasized the mTBI sample given the primary relevance of this group to our study aims and neuropsychological practice. However, we also examined whether the paths by which personality predicts mTBI symptom outcomes were similar in the OTC sample to inform understanding of the specificity of the main findings to mTBI patients. Two-tailed, bivariate Pearson correlations were used to examine relationships among personality, acute symptom ratings, and acute and chronic mTBI symptoms (mTBI; n = 75 for acute data, n = 50 for chronic data). Skewness and kurtosis were within the bounds (± 2) for the majority of symptom variables to consider the use of parametric statistics appropriate (Kendall, Stuart, Ord, & Arnold, Reference Kendall, Stuart, Ord and Arnold1999), so these were favored given their widespread use and interpretability. Kurtosis fell just outside these bounds for two variables – PID-5-BF Disinhibition (2.15) and Antagonism (2.23) — but sensitivity analyses comparing parametric and nonparametric associations with these variables confirmed that the decision made no meaningful difference on the results.
Linear regression analyses (mTBI; n = 50) were performed to identify the predominant personality and acute symptom predictors of chronic mTBI symptoms and establish the degree to which chronic mTBI symptoms could be predicted from the independent variables. Forward stepwise elimination variable selection was employed, and independent variables with bivariate associations with chronic symptoms at p ≤ .10 were considered for inclusion in the parsimonious multivariate model. Variables were retained in the model if they significantly improved the model R 2 (α = .05). Two-way interactions were tested among variables that demonstrated main effects; interaction terms were not included in the reported models unless significant.
Finally, we tested a series of modern mediation and conditional process (moderated mediation) models to explore how maladaptive and adaptive personality traits influence chronic mTBI symptoms. As described in the Results, patterns of association between personality and outcomes in mTBI (n = 50) were similar across indicators of the higher-order internalizing personality dimension theorized by other authors (i.e., negative affect/emotionality, detachment; see Wright, Thomas, Hopwood, Markon, Pincus, & Krueger, Reference Wright, Thomas, Hopwood, Markon, Pincus and Krueger2012). Thus, to reduce the number of mediation models examined, we derived an Internalizing Traits composite variable from our total sample (N = 154) that was used in subsequent analyses. We estimated regression-based factor scores from a 1-factor exploratory principal axis factor analysis of MPQ NEM, PID-5 Negative Affect, and PID-5 Detachment. PID-5 Psychoticism was not included because of prior evidence that it reflects a construct distinct from (although correlated with) internalizing and externalizing personality dimensions (Wright et al., Reference Wright, Thomas, Hopwood, Markon, Pincus and Krueger2012). All three variables loaded robustly (range .70 to .82) on a single common factor (eigenvalues 2.13, .49, .39) that explained 70.9% of the total variance in item ratings.
Next, in mTBI and OTC groups we tested all reasonable path model configurations and followed recommended practice to select the most complex path model that was supported by the data as the final path model (Hayes, Reference Hayes2018). All statistical analyses were performed in IBM SPSS Statistics, version 25 (IBM Corp, Armonk, NY, USA), and path modeling used the PROCESS version 3 macro (Hayes, Reference Hayes2018) for SPSS. Only one predictor (X) variable is allowed in these models, so each model configuration was tested separately for each personality predictor. Following PROCESS terminology, Model 1 reflected a simple moderation effect with PEM moderating the association between the maladaptive personality trait (X) and chronic mTBI symptoms (Y). Model 4 represented a simple mediation model with one mediating variable between X and Y. Model 5 was an extension of Model 4 with addition of a moderator on the c’ path (i.e., testing for mediation and separately for moderation on the direct path from X to Y). Model 7 was an extension of Model 4 with addition of a moderator on the a path (i.e., testing for moderated mediation on the indirect path from X to the mediator). Moderation effects were probed using simple slopes reflecting specified levels of the moderator and the Johnson-Neyman technique for detecting regions of significance.
Results
Characteristics of the mTBI Sample
Demographic and injury characteristics are presented in Table 1. The mTBI sample was demographically diverse with regard to age, gender, and education, identified primarily as Caucasian followed by African American, and demonstrated average mean estimated baseline intellectual functioning (i.e., WRAT-4 Word Reading performance). The most common cause of injury was motor vehicle collision (56.0%) and fall (38.7%). Acute injury characteristics were distributed as follows: 66.7% loss of consciousness, 48.0% posttraumatic amnesia, and 17.3% retrograde amnesia. About half of this sample (54.7%) had acute intracranial findings (CT+) on clinical head CT scans, a similar percentage as the 3-month follow-up subsample (60.0%). The CT+ and CT− groups were not statistically different on Injury Severity Score (t[69] = −1.23, p = .221) or length of hospital admission (t[73] = 1.33, p = .188).
There were no differences between those who completed the 3-month follow-up (n = 50) versus those who did not in age, gender, education, or mTBI type (i.e., with vs. without acute intracranial findings on head computed tomography [CT] scans). However, mTBI participants who completed the follow-up had lower acute symptom severity ratings (SCAT; M = 38.2, SD = 27.8) versus those who did not (M = 55.4, SD = 33.1; p = .03; Cohen’s d = .56).
SCAT scores for acute and chronic timepoints are also presented in Table 1. In the mTBI subgroup who completed the follow-up (n = 50), SCAT scores declined significantly between acute (M = 38.2, SD = 27.8) and chronic (M = 27.0, SD = 27.4) timepoints, t(49) = 2.84, p = .007; Cohen’s d = .41. Descriptive statistics for acute somatic and emotional distress measures are also summarized in Table 1.
Single Predictors of Chronic mTBI Symptoms
Table 2 presents bivariate associations between acute symptom and personality predictors of acute and chronic mTBI symptoms in the mTBI sample. Acute SCAT symptom severity was, as expected given construct/measure overlap, the strongest single predictor of 3-month SCAT scores (r = .49, p < .001). Among the remaining acute symptom predictors, Somatic Complaints scale (RC1) was the strongest predictor of persistent mTBI symptoms (r = .47), although BSI-18 GSI, Somatization, and Anxiety also significantly predicted chronic mTBI symptoms. Conversely, depression/anhedonia as measured by the BSI-18 and Low Positive Emotions scale (RC2) was not significantly associated with chronic mTBI symptoms.
Table 2. Bivariate correlations between acute symptoms, personality characteristics, and chronic mTBI symptoms in mTBI (n = 75)
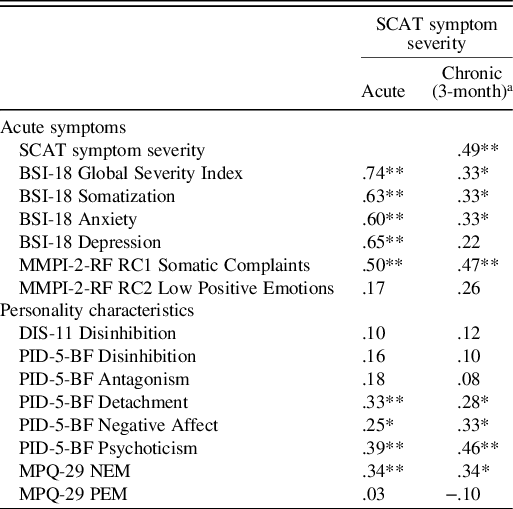
Note. SCAT = Sport Concussion Assessment Tool 3/5 (raw score total); BSI-18 = Brief Symptom Inventory-18 (T); MMPI-2-RF = Minnesota Multiphasic Personality Inventory-2-Restructured Form (T); DIS-11 = Disinhibition Scale of Externalizing Spectrum Inventory (mean item score); PID-5-BF = Personality Disorder Inventory for DSM-5 – Brief Form (mean item score); MPQ = MPQ-29 = Multidimensional Personality Questionnaire (mean standardized [Z] domain score); NEM = negative emotionality; PEM = positive emotionality. T scores (M = 50, SD = 10). Z scores (M = 0, SD = 1.0).
*p < .05, **p < .01.
a Chronic group (n = 50).
Among personality dimensions assessed, trait Psychoticism was the strongest single predictor of chronic mTBI symptoms (r = .46) in the mTBI group. Personality traits associated with internalizing tendencies (detachment and negative affectivity/emotionality) also predicted chronic mTBI symptoms (r = .28–.34), whereas traits associated with externalizing (disinhibition, antagonism) were not significantly related to mTBI symptoms. Consequently, a common Internalizing Traits factor was estimated for use in subsequent analyses, which correlated with chronic mTBI symptoms similarly to its component variables (r = .38, p < .01).
Multivariate Predictors of Chronic mTBI Symptoms
A parsimonious multivariate model was developed to identify the primary unique personality and acute symptom predictors of chronic mTBI symptoms and estimate to what degree these psychological and personality constructs predict this outcome in mTBI. These models considered all variables from Table 2 as well as the internalizing personality composite variable. The final regression model is presented in Table 3. In particular, findings were threefold: (A) Psychoticism incrementally predicted chronic mTBI symptoms beyond acute mTBI symptoms (see Model 2), (B) Psychoticism was the strongest, and only unique, personality predictor of chronic mTBI symptoms (e.g., internalizing personality did not significantly predict chronic symptoms when controlling for Psychoticism), and (C) Acute Somatic Complaints (RC1) also incrementally predicted the outcome beyond acute SCAT symptom severity and Psychoticism (Model 3). The final parsimonious model with the independent variables acute mTBI symptoms, Psychoticism, and Acute Somatic Complaints predicted 41% of the variance in chronic mTBI symptoms, substantially more than the variance explained by acute mTBI symptoms alone (24%).
Table 3. Personality and acute symptom predictors of chronic mTBI symptoms in mTBI: final stepwise regression model (n = 50)

Note. SCAT = Sport Concussion Assessment Tool 3/5 (raw score total); PID-5-BF = Personality Disorder Inventory for DSM-5 – Brief Form (mean item score); MMPI-2-RF = Minnesota Multiphasic Personality Inventory-2-Restructured Form (T). T-scores (M = 50, SD = 10).
*p < .05, **p < .01, ***p < .001.
Causal Pathways to Chronic mTBI Symptoms
The regression models clarified the predictive power of Psychoticism and Acute Somatic Complaints (RC1) but could not inform the question of how personality influences the persistence of symptoms in mTBI. Therefore, we estimated several mediation and moderated mediation models to explore this question. Prior to investigating models, analytic decisions were made to balance our desire to consider a range of reasonable candidate path models while keeping the number of models run to a minimum. First, we selected two personality variables for consideration: Psychoticism, based on its performance as the strongest overall personality predictor of chronic mTBI symptoms in mTBI, as well as internalizing personality. Internalizing personality was retained due to its robust bivariate association with the outcome in mTBI and because its performance in the multivariate regression models does not necessarily preclude it from playing an important role in a path model. Second, although acute general distress (GSI) and Somatic Complaints (RC1) were a priori mediators of interest based on correlational data, the regression results clarified that only RC1 was likely to act as a mediating variable and was retained solely to minimize the number of models. Finally, PEM was selected a priori as an index of adaptive personality and considered as a potential moderator of the maladaptive personality traits.
With these model components selected, we modeled all reasonable path model configurations (e.g., PROCESS Models 1, 4, 5, and 7, described in the Method). Consistent with contemporary recommendations for identifying causal pathways, models were tested by systematically incorporating increasing levels of complexity through the addition of mediators and moderators until the most complex model supported by the data was identified (Hayes, Reference Hayes2018). There was not a strong literature to guide placement of RC1 as a predictor (i.e., personality trait variable) or mediator (i.e., measure of acute symptoms/emotional state). However, given the behavior of RC1 in the regression models, RC1 was placed as a mediator; if these analyses supported it as a mediator that was considered to be positive empirical support for this decision. The configuration and statistical output for all models evaluated are presented in Table 4.
Table 4. Data summary for mediation, moderation, and moderated-mediation models predicting 3-month mTBI symptoms

Note. OTC = orthopedic trauma controls. Bootstrap = 10,000 with 95% CI. X = predictor variable. Cov. = covariate. INT = internalizing personality standardized factor score. RC1 = MMPI-2-RF Somatic Complaints (T). PEM = MPQ-29 positive emotionality (mean standardized (Z) score). PSY = PID5-BF Psychoticism (mean item score). R 2 = variance explained when outcome variable is SCAT. a = predictor to mediator path. b = mediator to outcome path. ab = indirect path. c’ = direct path. c = total effect. CSIE = completely standardized indirect effect. IMM = Index of Moderated Mediation. Range = moderator values defining Johnson-Neyman significance region; % = percent below significance region. Bolded = significant model elements and/or paths. Model numbers refer to the PROCESS version 3 model configurations and are described in the Data Analyses subsection.
*p < .05, **p < .01.
The optimal model developed using Psychoticism as the predictor is depicted in Figure 1A (corresponding fit statistics are in Table 4 and denoted by the superscript A). In mTBI, Psychoticism had a direct effect on chronic mTBI symptoms (i.e., was not moderated by PEM or mediated by acute somatic complaints).

Fig. 1. Causal models predicting persistent mTBI symptoms in mild traumatic brain injury (mTBI; n = 50) and orthopedic trauma controls (OTC; n = 53). Note. (A) In mTBI, Psychoticism (PID-5-BF) had a direct effect on chronic mTBI symptoms (SCAT). In OTC, Psychoticism had an indirect effect on chronic mTBI symptoms through enhancement of acute post-injury somatic complaints (RC1) and a conditional direct effect at low levels of positive emotionality (PEM). (B) In mTBI and OTC, the internalizing personality traits composite variable had an indirect effect on chronic mTBI symptoms through enhancement of acute post-injury somatic complaints and a conditional direct effect at low levels of positive emotionality; when controlling for psychoticism, the conditional direct effect only held for the OTC group.
The optimal model using internalizing personality traits composite variable (i.e., detachment and negative emotionality) as the predictor is illustrated in Figure 1B (fit statistics are in Table 4 and denoted by the superscript B). In mTBI, internalizing personality traits had an indirect effect on chronic mTBI symptoms through enhancement of acute somatic complaints (mediation) and a conditional direct effect on chronic mTBI symptoms at low levels of PEM (i.e., moderation; PEM scores in the range of −1.52 to −.30). Psychoticism subsequently was included as a covariate because of its importance in the mTBI regression analyses; the mediation of internalizing personality traits through acute somatic complaints remained significant, but the PEM moderation finding became non-significant.
Comparisons with OTC
Demographic and injury characteristics of the OTC sample (n = 79) are presented in Table 1. The OTC group was diverse in age, gender, and education, identified primarily as Caucasian, and demonstrated average mean estimated intellectual functioning (WRAT-IV Word Reading). The most common cause of injury was fall (43%) followed by motor vehicle/traffic accident (35%). There were no differences between OTC participants who completed the 3-month follow-up versus those who did not in education, acute SCAT scores, or chronic SCAT scores. However, OTC participants who completed the follow-up were older (M = 52.7, SD = 16.8) versus those who did not (M = 38.1, SD = 17.9; p = .002; Cohen’s d = .84), and females were more likely than males to complete the follow-up (χ 2 (1) = 5.31, p = .021).
The mTBI and OTC samples were comparable in many Table 1 variables with a few exceptions. Demographically, there were more males in the OTC group at baseline (χ 2 (1) = 8.35, p = .004), but this difference was not significant in the subsample with follow-up data. Cause of injury varied with significantly more assaults in the OTC group at baseline (χ 2 (3) = 11.22, p = .011), but this difference was not significant in the follow-up subsample. As expected given group criteria, the mTBI group had significantly more injuries resulting in loss of consciousness (χ 2 (1, 151) = 60.20, p < .001), posttraumatic amnesia (χ 2 (1, 154) = 49.49, p = < .001), and retrograde amnesia (χ 2 (1, 153) = 14.78, p = < .001). The mTBI group had higher acute distress on the BSI-18 GSI (t(152) = 1.20, p = .048; Cohen’s d = .32) and acute somatic complaints on the MMPI-2-RF RC1 (t(151) = 2.37, p = .019; Cohen’s d = .38) at baseline, but these differences were not significant in the follow-up subsample. The mTBI group had higher acute SCAT symptom severity than the OTC group (t(142.43) = 3.92, p = < .001; Cohen’s d = .63); this group difference held in the follow-up subsample. Notably, mTBI and OTC groups did not differ on chronic SCAT ratings. There were also no group differences on personality measures in the follow-up subsample.
In order to determine if the causal models identified through PROCESS analyses were unique to mTBI, a parallel set of mediation analyses as described for the mTBI sample were completed within the OTC group (see Table 4 for model configurations and output). The optimal model using Psychoticism as the predictor is depicted in Figure 1A (fit statistics are in Table 4 and denoted by the superscript A). In OTC, Psychoticism had an indirect effect on chronic mTBI symptoms through enhancement of acute somatic complaints (mediation) and a conditional direct effect on chronic mTBI symptoms at low levels of PEM (moderation; PEM scores in the range of −1.83 to −1.26). The optimal model using internalizing personality traits composite variable (i.e., detachment and negative emotionality) as the predictor is illustrated in Figure 1B (fit statistics are in Table 4 and denoted by the superscript B). In OTC, internalizing personality traits had an indirect effect on chronic mTBI symptoms through enhancement of acute somatic complaints and a conditional direct effect on chronic mTBI symptoms at low levels of PEM (moderation; PEM scores in the range of −1.83 to .00), which held after controlling for Psychoticism.
Discussion
This study provided a prospective, comprehensive examination of the degree to which diverse risk and resilience personality dimensions predict mTBI symptom recovery, expanding understanding of the well-accepted but understudied relationship between pre-injury traits and mTBI outcomes. Our key findings were threefold: (1) consistent with hypotheses, internalizing personality traits (including detachment and negative affect) robustly predict chronic mTBI symptoms; (2) more novel, trait psychoticism emerged as an even stronger predictor of chronic mTBI symptoms (uniquely predicting this outcome over and above internalizing symptoms in individuals with mTBI specifically); and (3) psychoticism and internalizing personality may influence chronic mTBI symptoms through different pathways after mTBI specifically (psychoticism had a direct influence and internalizing personality has an indirect influence by enhancing somatic complaints). With the exception of psychoticism, which demonstrated different causal paths to chronic mTBI symptoms in the mTBI and OTC groups, other personality and symptom variables appeared similarly valuable in understanding chronic “post concussive symptoms” regardless of the cause of injury, implying some generalizability in the role of personality and chronic mTBI-related symptoms.
The fact that internalizing personality traits predicted chronic mTBI symptoms was not surprising in light of a large literature linking personality traits, such as neuroticism and negative affect, and general health outcomes, including symptom recovery following mTBI (e.g., Broshek et al., Reference Broshek, De Marco and Freeman2015; Lahey, Reference Lahey2009). More novel, this study further extends the research base by identifying a potential causal pathway by which internalizing personality traits influence mTBI recovery through enhancement of acute somatic complaints. This finding is consistent with prior research demonstrating associations between somatization and poor mTBI outcomes (Nelson et al., Reference Nelson, Tarima, LaRoche, Hammeke, Barr, Guskiewicz and McCrea2016) and addresses critical gaps in the research by identifying a possible mechanism linking personality and health outcomes (Smith, Reference Smith2006).
Another key finding of this study was that trait psychoticism was the strongest and only unique personality predictor of chronic mTBI symptoms in persons who sustained mTBI. The meaning of this finding is unclear given the novelty of assessing psychoticism in a TBI study and uncertainty about the clinical implications and correlates of varying levels of this trait. As measured in this study via the PID-5-BF inventory, trait psychoticism reflects low versus high eccentricity, cognitive and perceptual dysregulation, and unusual beliefs and experiences (Krueger et al., Reference Krueger, Derringer, Markon, Watson and Skodol2012), akin to Psychoticism as assessed by Harkness’ Personality Psychopathology 5 (PSY-5) model of clinically relevant personality traits (Harkness, McNulty, & Ben-Porath, Reference Harkness, McNulty and Ben-Porath1995). Psychoticism is not synonymous with “psychosis” but is considered a continuum ranging from low to high levels of eccentricity to, at the highest end of the spectrum, proneness to hallucinations and delusions. Indeed, high levels of PID-5 Psychoticism have been found to help discriminate between individuals with versus without clinical psychosis (Bastiaens et al., Reference Bastiaens, Smits, De Hert, Thys, Bryon, Sweers and Claes2019). At lower levels of the spectrum, however, the implications of varying degrees of psychoticism are less clear. Contemporary models of personality and psychopathology place psychoticism as distinct from internalizing and externalizing personality dimensions (e.g., Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby and Zimmerman2017; Kreuger & Markon, Reference Krueger and Markon2014) or as falling under the internalizing dimension but being distinct from fear and distress (e.g., Keyes et al., Reference Keyes, Eaton, Krueger, Skodol, Wall, Grant and Hasin2013). Within the FFM of personality, psychoticism has also been described as a maladaptive end of the openness to experience factor (Gore & Widiger, Reference Gore and Widiger2013), although the link between psychoticism and openness to experience appears weak at a global level and may only hold for select subfacets of these dimensions (Chmielewski et al., Reference Chmielewski, Bagby, Markon, Ring and Ryder2014; Suzuki et al., Reference Suzuki, Griffin and Samuel2017).
These theoretical and empirical frameworks help give context to our finding that psychoticism functioned quite differently from internalizing and externalizing traits in individuals with mTBI and had a robust, direct effect on their chronic mTBI symptom reporting. The emphasis on reality distortion or cognitive/perceptual disturbance is a particularly salient construct in considering how psychoticism might influence response to injury. Perhaps individuals high in psychoticism are predisposed to experience heightened perception of or sensitivity to mental or physical experiences, thus increasing symptom endorsement. However, it remains unclear how psychoticism may affect chronic “post-concussive” symptom reporting differently in persons with mTBI versus other forms of traumatic injury as shown in this study. It is also possible that this difference in group findings may be secondary to low power. Although we were powered sufficiently to detect complex mediation and moderation paths in both mTBI and OTC, it is possible that there were meaningful but smaller effects in the mTBI psychoticism analyses that we lacked statistical power to detect. However, that the association between psychoticism and chronic symptoms remain similarly robust after controlling for somatic complaints (B = .34 vs. .33 without vs. with somatic complaints in the model; see Table 3) suggests that somatic complaints do not meaningfully mediate the relationship between psychotic and chronic mTBI symptoms in patients with mTBI. Thus, the findings suggest there is something unique to how personality factors, such as psychoticism, influence symptom experience after brain injury. Further research into the dimensions of psychoticism and its neurobiological underpinnings may advance both models of psychopathology and understanding this possible link between psychoticism and TBI outcomes. For example, emerging work is uncovering a number of neurobiological correlates of thought disorder relevant to TBI, such as inflammatory and autonomic nervous system functioning (Suvisaari & Mantere, Reference Suvisaari and Mantere2013; Toichi, Reference Toichi1999; Pertab, Merkley, Cramond, Cramond, Paxton, & Wu, Reference Pertab, Merkley, Cramond, Cramond, Paxton and Wu2018; Moganti-Kossmann, Rancan, Stahel, & Kossman, Reference Moganti-Kossmann, Rancan, Stahel and Kossmann2002). Future work should investigate the neurobiological underpinnings of these types of personality-outcome associations to strengthen the biopsychosocial understanding of risk and resilience factors for mTBI recovery.
Furthermore, by deepening our understanding of how personality influences mTBI outcomes, this study may also provide additional context for prior work linking personality, psychopathology, and chronic mTBI symptom reporting. In particular, several studies have demonstrated a paradoxical severity effect in which mTBI groups endorse higher rates of personality and emotional pathology than moderate and severe TBI groups, with endorsement on psychopathology measures corresponding with higher rates of mTBI symptoms (Kennedy, Cooper, Reid, Tate & Lange, Reference Kennedy, Cooper, Reid, Tate and Lange2015; Kurtz, Shealy, & Putnam, Reference Kurtz, Shealy and Putnam2007). This study provides a potential window into that process and underscores the importance of personality factors in predicting injury response. Demonstrating similarities in how personality and somatic symptoms constructs influence “post concussive symptoms” in both mTBI and trauma control groups may help improve understanding of persistent mTBI-like symptom reporting independent of mTBI and adds to the literature addressing PCS as a construct. For instance, Garden, Sullivan, and Lange (Reference Garden, Sullivan and Lange2010) examined a non-clinical sample and found that nearly half of the sample met ICD-10 PCS diagnostic criteria and that this subgroup endorsed high levels of emotional distress and dysfunctional personality styles (i.e., dependent, sadistic, somatic, borderline). It is possible that the causal models incorporating personality factors in this study of mTBI and general trauma recovery may translate to non-clinical samples, as might be expected based on Garden, Sullivan, and Lange (Reference Garden, Sullivan and Lange2010). This could be an interesting area for future research to elucidate, which, if confirmed, might serve to reinforce the perspective of PCS as a flawed construct with symptoms and underlying causal mechanisms that are non-specific to brain injury.
This study has several methodological strengths, including its prospective design and broad assessment of personality and psychopathology risk and resilience variables. The use of abbreviated personality inventories may increase the translatability of the findings into clinical practice, where any bedside clinical assessment needs to be brief. In addition, our use of path analyses represents both a design advantage (i.e., allows for direct assessment of causal pathways) and statistical advantage (i.e., using modern mediation approaches to enhance ability to identify complex models). Limitations of this study include having a modest sample size that limited the ability to examine subgroup differences, such as cause of injury or gender, which have been shown to have some relevance to outcome. Further, as the study was power planned to detect bivariate associations between personality and outcome measures, mediation models were admittedly exploratory and power planning difficult in the context of these more complex analyses (Hayes, Reference Hayes2018). As such, these findings are preliminary and should be replicated in an independent sample. Additionally, because of time constraints performing bedside exam in the inpatient environment, symptom validity was not assessed, which could be a useful future consideration. In addition, the racial diversity of this sample was somewhat limited relative to the broader US population. Thus, generalizations to racial or ethnic minority groups should not be made given that such groups often perform differently on measures of personality and psychopathology than Caucasians. Generalizability may also be limited to groups comprising complicated and uncomplicated injuries, at least until additional studies can clarify to what extent this injury marker and potential underlying neurobiological mechanisms might be relevant to understanding personality influences on symptom reporting. Furthermore, consistent with the vast majority of civilian mTBI research, participants were enrolled post-injury, and it is unknown to what degree self-ratings of pre-injury personality may be affected by injury. However, it is unlikely that mild brain injuries markedly impact personality function, and other research suggests that TBI patients are accurate and consistent in their post-injury personality ratings over time (Rush, Malec, Brown, & Moessner, Reference Rush, Malec, Brown and Moessner2006).
In conclusion, this study advances understanding of the importance of personality traits for mTBI recovery and highlights areas for potential advancement in personalized medicine for mTBI. Our findings may be particularly useful in secondary prevention efforts targeting individuals at risk for prolonged and/or complicated recoveries after mTBI, such as through integrating brief, predictive personality measures into routine clinical evaluation and management efforts. Overall, this research underscores the importance of the biopsychosocial model in understanding mTBI recovery and has direct implications for ongoing research, conceptualization, and treatment of this population.
Acknowledgements
This work was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, under Grant UL1TR000055, and the National Institute of Neurological Disorders and Stroke grant #R01 NS110856. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. In addition, this project was funded by the Research and Educational Program Fund, a component of the Advancing a Healthier Wisconsin endowment of the Medical College of Wisconsin. We thank Amy Nader, Tim Geier, and Josh Hunt for their work on the study.
Conflict of Interest
The authors have no conflicts of interest to declare.







