Introduction
A priority focus on palliative and supportive care is supporting the 43.5 million caregivers who care for individuals with serious illness. Increasing attention is being paid to the high demands placed on family caregivers, who provide an average of 24 h of unpaid support per week to relatives and friends with a serious health condition or disability (National Alliance for Caregiving and American Association for Retired Persons, 2015). For many caregivers, undertaking this role is burdensome and distressing, resulting in increased anxiety, depression, and poor quality of life (Ho et al., Reference Ho, Chan and Woo2009; Nielsen et al., Reference Nielsen, Neergaard and Jensen2016; Geng et al., Reference Geng, Chuang and Yang2018). Other negative health effects and behaviors among caregivers have been documented, including increased cardiovascular events and decreased preventive health behaviors (Son et al., Reference Son, Erno and Shea2007; Reeves et al., Reference Reeves, Bacon and Fredman2012; Dionne-Odom et al., Reference Dionne-Odom, Demark-Wahnefried and Taylor2017), especially among women and spousal caregivers (Bom et al., Reference Bom, Bakx and Schut2018). Given the increasing number of patients with serious illness (Hughes and Smith, Reference Hughes and Smith2014), the burden on family caregivers is expected to increase, and it is important that palliative and supportive care teams better understand their unmet needs and provide optimal resources to minimize distress.
Optimizing social aspects of care for patients with serious illness and their families is a clinical practice guideline domain for quality palliative care (Ferrell et al., Reference Ferrell, Twaddle and Melnick2018). Social support is one resource that may be helpful to minimize distress and improve quality of life. Social support provides practical and emotional resources to help individuals to cope with stressful life events, particularly when this support is responsive to previously unmet needs (Collins and Feeney, Reference Collins and Feeney2000; Feeney and Collins, Reference Feeney and Collins2015). Research examining the link between social support and distress, including among caregivers, reveals a strong link between high perceived social support and lower levels of distress and burden (Adelman et al., Reference Adelman, Tmanova and Delgado2014; Santini et al., Reference Santini, Koyanagi and Tyrovolas2015; Chang et al., Reference Chang, Zhang and Jevagurunathan2016; Del-Pino-Casado et al., Reference Del-Pino-Casado, Frias-Osuna and Palomino-Moral2018). A recent meta-analysis found a moderate negative association between perceived social support and burden among caregivers of older adults (Del-Pino-Casado et al., Reference Del-Pino-Casado, Frias-Osuna and Palomino-Moral2018). Perceived social support can be differentiated as appraisal, instrumental support, emotional support, and informational support (LaRocco et al., Reference LaRocco, House and French1980; House et al., Reference House, Umberson and Landis1988). Instrumental support refers to assistance with material and task performance for oneself, such as help with household chores and transportation to medical appointments (Seeman and Berkman, Reference Seeman and Berkman1988), and its receipt is linked to better health outcomes (Berkman, Reference Berkman1984). Caregivers, in particular, need instrumental support, both related and unrelated to their caregiving activities, given the high demand placed on them to perform many tasks, often with little formal assistance or training.
Distressed individuals have better health outcomes in general when they receive support (Girme et al., Reference Girme, Overall and Simpson2013). Caregivers specifically report lower distress when they receive higher instrumental support (Jarrott et al., Reference Jarrott, Zarit and Stephens2005). However, some studies report conflicting findings. A replication analysis of studies examining social support and distress among caregivers found that higher instrumental support was associated with lower distress in only one out of four datasets examined, indicating the need to further study the role that instrumental support plays in alleviating caregiver distress (Miller et al., Reference Miller, Townsend and Carpenter2001). Theoretically, instrumental support to help caregivers directly as well as with caregiving tasks may bolster caregiver coping (Miller et al., Reference Miller, Townsend and Carpenter2001; Nishio et al., Reference Nishio, Kimura and Ogomori2017). However, population-based studies of instrumental support provided to family caregivers are limited. The objective of the current study was to identify relationships between instrumental support and caregiver distress in a national sample of U.S. family caregivers of adults with serious health problems. We hypothesized that higher instrumental support would be associated with lower caregiver distress. We also hypothesized that the association between support and distress would differ by the level of caregiving burden.
Methods
Data source
We analyzed data from the 2018 Health Information National Trends Survey (HINTS), Version V, Cycle 2. Briefly, HINTS is an annual nationally representative survey about the American public's use of health information, health behaviors, and health communication patterns (Hesse et al., Reference Hesse, Greenberg and Peterson2017). We chose this HINTS cycle because it contained a module on caregiving and a validated instrumental support measure.
Participants
We defined informal/family caregivers in the current study as those positively endorsing the item “currently caring for or making healthcare decisions for someone with a medical, behavioral, disability, or other condition” (n = 474). We excluded those who indicated that they were caregiving solely for a child or children (n = 122), given the variation in cultural conceptions about illness across the life course and differences in the way healthcare delivery is organized between adults and children. We also excluded caregivers who reported that they were paid for any part of the care they provided (n = 41) to avoid including home healthcare aids and to focus on unpaid family caregivers, leaving a total of n = 311 informal caregivers of adults.
Measures
We measured psychological distress by using a combination of depressive and anxiety symptoms from the Patient Health Questionnaire (PHQ-4) (Kroenke et al., Reference Kroenke, Spitzer and Williams2009; Ellis et al., Reference Ellis, Orom and Giovino2015), as done in previous caregiving studies (Denno et al., Reference Denno, Gillard and Graham2013; Haun et al., Reference Haun, Sklenarova and Brechtel2014; Chang et al., Reference Chang, Zhang and Jevagurunathan2016). Anxiety symptoms were measured using two items: (1) “being bothered by feeling nervous, anxious, or on edge” and (2) “not being able to stop or control worrying” (range: 0–6; r = 0.70). Depressive symptoms were measured by two items: (1) “being bothered by feeling down, depressed, or hopeless” and (2) “having little interest or pleasure in doing things” (range: 0–6; r = 0.74). All four items were summed to create a measure of psychological distress (range: 0–12). High scores indicate high distress. We categorized the PHQ-4 according to established clinical ranges of distress [within normal limits (WNL): 0–2, mild: 3–5, moderate: 6–8, severe: 9–12] (Kroenke et al., Reference Kroenke, Spitzer and Williams2009).
We used the four-item Patient-Reported Outcomes Measurement Information System® (PROMIS®) Short-Form (SF) v2.0 Instrumental Support 4a measure to assess instrumental support reported to be received by caregivers (Hahn et al., Reference Hahn, DeWalt and Bode2014). Note that the PROMIS instrumental support measure is not specific to caregiving; items refer to support for oneself generally. Items assessed whether caregivers have “someone to prepare meals if unable to do themselves,” “someone to take them to the doctor if needed,” “someone to help with daily chores if they are sick,” and “someone to run errands if needed.” All responses use a 5-point Likert scale ranging from “never” to “always.” PROMIS measures are reported on a T-score metric; 50 is considered average in the US general population, and 10 points equates to one standard deviation. For the current study, Cronbach's α for PROMIS instrumental support was 0.90. Guidelines for interpretation of PROMIS scores suggest that 3–5 points indicate a meaningful difference in outcome (Northwestern University, 2019). Details on the performance of the PROMIS instrumental support measure for the HINTS caregiving sample are provided in Supplementary Appendix 1.
Socio-demographic covariates included age at survey (categorical: 18–34, 35–49, 50–64, 65–74, 75+), gender (dichotomized: male or female), race/ethnicity (categorical: Non-Hispanic White, Non-Hispanic Black, Hispanic, and Non-Hispanic Other), household income (dichotomized: ±$75 K), educational attainment (categorical: high school graduate or less, some college or technical school, or college graduate or above), employment (categorical: employed/student, not working or in school, retired), geographic density based on residence at survey (dichotomized: urban vs. rural, based on 2003 US Department of Agriculture Rural/Urban Commuting Area (RUCA) Codes: urban = 1–3, rural = 4–9) (Weaver et al., Reference Weaver, Geiger and Lu2013). Additionally, we included caregiving-specific variables. We stratified caregiving duration at ±2 years (National Alliance for Caregiving and American Association for Retired Persons, 2015). We captured caregiving burden as a composite variable comprised of the following weighted measures using an approach detailed by the National Alliance for Caregiving 2015 Caregiving in the USA: (1) hours of caregiving per week, (2) assistance with activities of daily living (ADLs, including bathing, dressing, toileting, incontinence assistance, feeding, and transfers from bed and chairs), and with (3) instrumental activities of daily living (IADLs, including meal preparation, assistance with finances, shopping, housework, and transportation) (National Alliance for Caregiving and American Association for Retired Persons, 2015). We assigned caregiving hours per week the following points: 0–8 h = 1 point; 9–20 h = 2 points, 21–40 h = 3 points, and 41+ h = 4 points. Both ADL and IADL assistance were summed according to tasks: 0 ADLs, 1 IADL = 1 point; 0 ADLs, 2+ ADLs = 2 points, 1 ADL, any IADLs = 3 points; 2+ ADLs, any IADLs = 4 points. We categorized the sum of both hours per week and ADL/IADL assistance points as low (2–4 points), medium (5 points), and high (6–8 points) (National Alliance for Caregiving, 2015).
To capture differences found in caregiving burden between spousal and non-spousal caregivers (Davis et al., Reference Davis, Gilliss and Deshefy-Longhi2011; Li et al., Reference Li, Mak and Loke2013; Reblin et al., Reference Reblin, Donaldson and Ellington2016), we classified care recipient relationship as spouse/partner vs. non-spouse/partner (dichotomous). We categorized care recipient condition as having had Alzheimer's/dementia, chronic conditions including cancer, other (orthopedic/musculoskeletal issues, mental health/behavioral/substance abuse issues, neurological/developmental issues, acute conditions, aging/aging-related conditions not listed, and other), or multiple conditions (categorical). We handled missing data using hot-deck imputation for selected socio-demographic variables (i.e., age [n = 5], gender [n = 2], race/ethnicity [n = 17], education [n = 4], and marital status [n = 4]). For household income, we included a missing category. We used listwise deletion for missing data on remaining variables.
Statistical analysis
We adjusted the multivariable linear regression models of instrumental support and distress for socio-demographics and caregiving variables. Given a known significant association between caregiving strain and caregiver distress (Bevans and Sternberg, Reference Bevans and Sternberg2012; Beinart et al., Reference Beinart, Weinman and Wade2012; Applebaum and Breitbart, Reference Applebaum and Breitbart2013; Evangelista et al., Reference Evangelista, Stromberg and Dionne-Odom2016) and that instrumental support can ameliorate burden (Badr and Krebs, Reference Badr and Krebs2013; Chi and Demiris, Reference Chi and Demiris2015; Ferrell and Wittenberg, Reference Ferrell and Wittenberg2017), we tested an interaction between caregiving burden level and instrumental support on distress. We reported adjusted mean instrumental support scores according to distress categories (Kroenke et al., Reference Kroenke, Spitzer and Williams2009). All models incorporated survey weights to account for complex sampling design and parameters were tested for significance at p < 0.05. We conducted statistical analyses using SAS version 9.4 (SAS Institute, Cary, NC) and SAS-callable SUDAAN version 11.0.0 (RTI International, Research Triangle Park, NC).
Results
A total of 474 respondents indicated that they were serving as an informal/family caregiver, representing 14.9% of the US adult population. Of those, 352 reported caring for an adult. Finally, of those individuals, 41 were excluded if they reported receiving payment for any part of that care. The final analytic subset included 311 individuals representing 23,452,665 (10.2% of the US adult population).
Caregiver characteristics are provided in Table 1. The majority of caregivers were female (64.8%), non-Hispanic White (64.9%), and married or partnered (70.7%). Many caregivers reported having attended some college or technical school (45.7%), and with household incomes at ≤$75 K (52.2%). Most caregivers reported working or studying (65.5%) and living in an urban environment (83.8%). Caregivers were most likely to report caring for a parent (42%), attending to a care recipient with multiple health problems (65.5%), and caring for more than 2 years (61.7%). More than half of caregivers reported low/no levels of burden (57.6%), with 29.3% reporting high burden, and 13.1% reporting medium burden.
Table 1. Socio-demographic and caregiving characteristics, HINTS 5 Cycle 2 Caregiving-Instrumental Support Study, n = 311 informal caregivers of adult recipients
Instrumental support
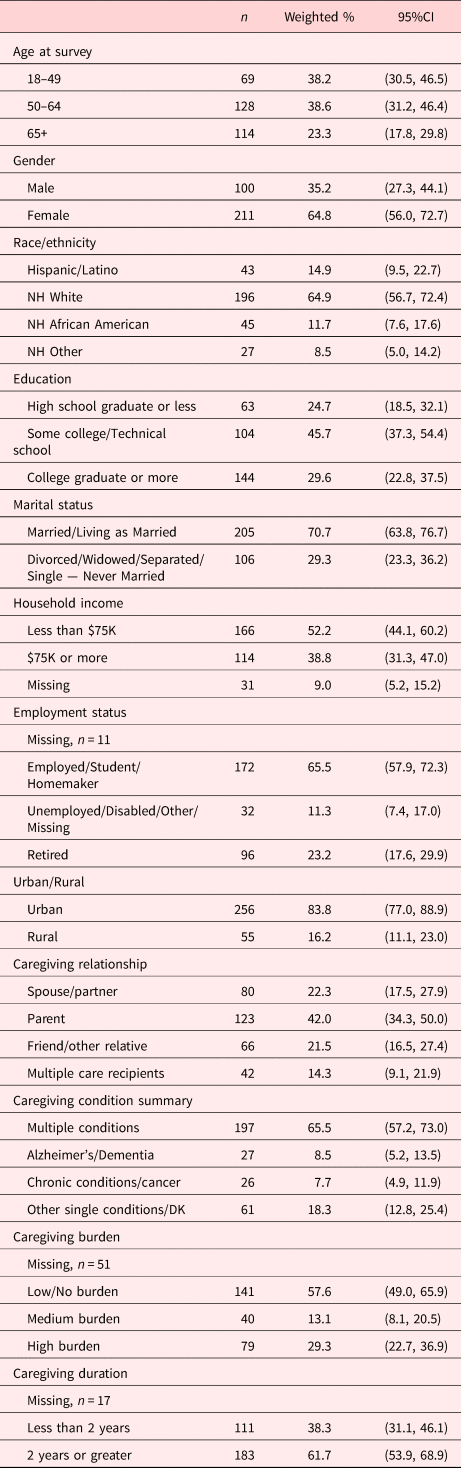
The distribution of instrumental support received was negatively skewed, with 31% of respondents indicating the highest level of support (T-score: 63.3; Figure 1). The mean unweighted instrumental support T-score was 50.4 (SD = 10.6, range = 29.3–63.3). The mean weighted instrumental support T-score was 51.22 (SE = 1.00).
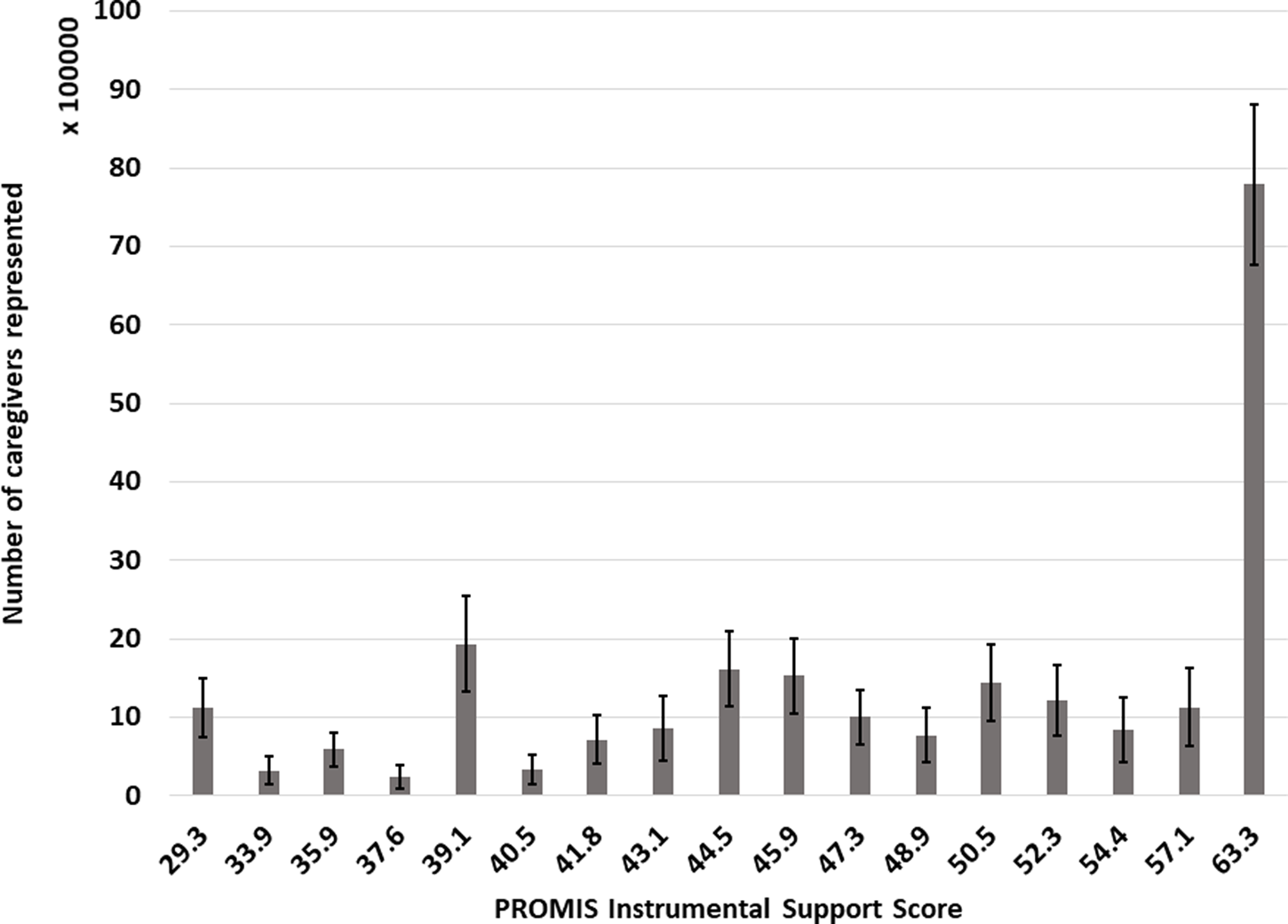
Fig. 1. Distribution of instrumental support reported by caregivers (n = 311, weighted n = 23,452,665). Error bars represent the standard error of the estimated population size.
Instrumental support and psychological distress
Table 2 shows the adjusted parameter estimates of the multivariable models regressing psychological distress on instrumental support, socio-demographic factors, and caregiving variables. Higher instrumental support was significantly associated with lower distress in both the unadjusted and adjusted models, (adjβ = −0.09, SE = 0.03, p = 0.003). Other variables significantly associated with distress in the adjusted model included younger age, employment status, and caregiving duration. Individuals ages 65+ at survey reported lower distress (adjβ = −2.31, SE = 0.92, p = 0.02) than those ages 18–49. Being employed/student/homemaker associated with lower distress than being unemployed/disabled (adjβ = −3.38, SE = 1.17, p = 0.006) and caring for ≥2 years compared to <2 years was associated with greater distress (adjβ = 1.44, SE = 0.52, p = 0.008). Neither caregiving burden (p = 0.73) nor the interaction term between caregiving burden and instrumental support was significant (p = 0.71); thus, the final model shown contains no interaction term.
Table 2. Adjusteda parameter estimates for linear regression on psychological distress (PHQ-4)

a Adjusted for all factors in the model, n = 282, r² = 0.33.
b Caregiving burden index from caregiving in the US survey, the composite score of assistance with activities of daily living, instrumental activities of daily living, and hours per week providing care.
Figure 2 shows the average level of instrumental support at clinical thresholds for distress: WNL: 52.3, mild: 49.4, moderate: 48.9, and severe: 39.7, demonstrating decreasing levels of instrumental support at each threshold of distress.
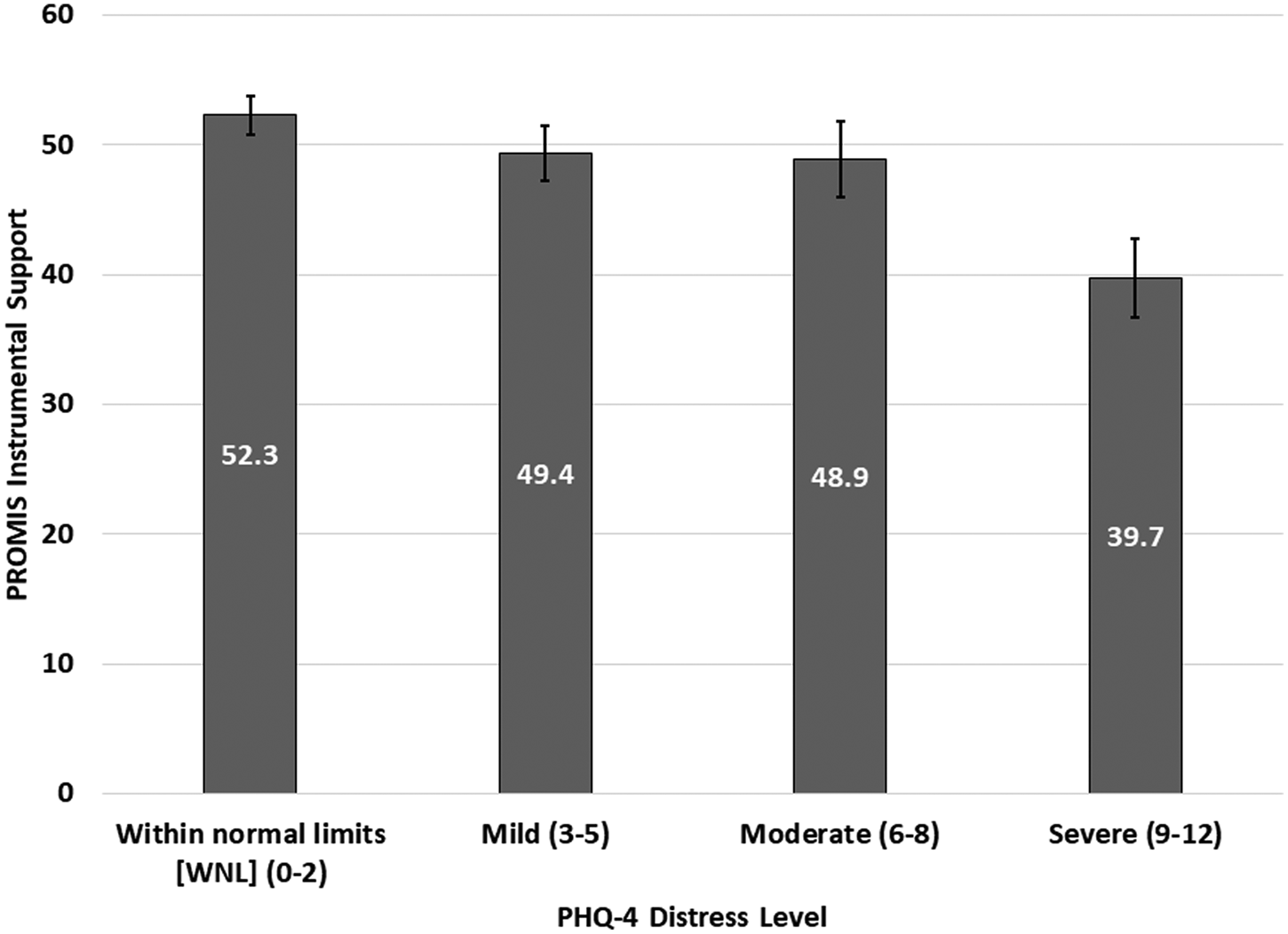
Fig. 2. Adjusted least-squared means of Instrumental Support by PHQ-distress level (WNL: n = 210, Mild: n = 57, Moderate: n = 19, Severe: n = 21, Missing: n = 4), r 2 = 0.28. Error bars represent 95% confidence intervals.
Discussion
In this population-based study of U.S. caregivers, we demonstrated a significant inverse association between instrumental support and psychological distress, after adjusting for key socio-demographic and caregiving variables. This supports our hypothesis that higher instrumental support is associated with lower distress. Our findings suggest that palliative and supportive clinicians should recognize social aspects of care in meeting patients and families’ needs.
Overall, high levels of instrumental support were reported among caregivers. While there are limited validation studies of the PROMIS instrumental support measure, in our study, the mean T-score was lower than reported in a study of adults receiving outpatient surgery (mean = 55, SD = 8.8) (Nota et al., Reference Nota, Spit and Oosterhoff2016) and higher than for patients with both a chronic illness and comorbid depression (mean = 47.2, SD = 10) (Hong et al., Reference Hong, Aspey and Bao2019). However, caregivers who reported any level of distress had significantly lower instrumental support than caregivers who reported no distress. This effect was largest for caregivers who reported “severe” distress and who indicated a level of instrumental support far lower than all other caregivers and others within the general population. This finding suggests that caregivers facing severe distress may be lacking in sufficient instrumental support.
Though not the primary association investigated in our study, it was surprising that caregiver burden was not significantly related to overall distress and did not modify the observed association between support and distress. However, consistent with the stress and coping model of caregiving (Fletcher et al., Reference Fletcher, Miaskowski and Given2012), greater duration of caregiving was associated with distress. Unemployment was also associated with caregiver distress, consistent with other findings in the caregiving literature (Longacre et al., Reference Longacre, Valdmanis and Handorf2017). Being unemployed could lead to distress in caregivers for many reasons, including financial distress from loss of income (de Moor et al., Reference de Moor, Dowling and Ekwueme2016) and loss of identity associated with work (Kim et al., Reference Kim, Baker and Spillers2006), as well as one component of role theory, role enhancement, which suggests that employment can buffer stress through social support and respite (Gonzales et al., Reference Gonzales, Lee and Brown2017). Other factors such as caregiver–care recipient relationship and care recipient health condition were not significantly associated with distress. Contextual, psychosocial factors related to relationship quality might be more important in predicting both burden and benefit-finding than relationship type or care recipient health condition in predicting distress (Reblin et al., Reference Reblin, Donaldson and Ellington2016); however, we could not determine this in the current study.
While there are many aspects of social support, perceived support (including instrumental, emotional, informational, and other forms of perceived social support) may be of particular importance when examining distress and other caregiving outcomes (Collins and Feeney, Reference Collins and Feeney2000; Gleason et al., Reference Gleason, Iida and Shrout2008; Feeney and Collins, Reference Feeney and Collins2015). Perceived support is distinct from and may have a greater impact on caregiver experience than support, otherwise assumed or observed (Gleason et al., Reference Gleason, Iida and Shrout2008; Uchino, Reference Uchino2009; Del-Pino-Casado et al., Reference Del-Pino-Casado, Frias-Osuna and Palomino-Moral2018). Assessing perceptions of support directly from caregivers, as was done in the current study, may be critical for palliative care clinicians trying to understand the actual impact of support on caregiver distress (Gleason et al., Reference Gleason, Iida and Shrout2008). In addition, social support may act as an effect modifier as well as a predictor, and its role should be examined in longitudinal datasets to provide further insight into the causality of social support and distress among caregivers.
These results point to the need for palliative and supportive care interventions that bolster perceived instrumental support among caregivers. There are several reviews of psychosocial interventions to support caregivers of adults with serious health problems, including heart failure (Evangelista et al., Reference Evangelista, Stromberg and Dionne-Odom2016), cancer (Ferrell and Wittenberg, Reference Ferrell and Wittenberg2017), and Alzheimer's disease (Beinart et al., Reference Beinart, Weinman and Wade2012), with interventions building upon different coping strategies. Problem-focused coping, which focuses on the individual's ability to adapt to and manage environmental stressors (Baker and Berenbaum, Reference Baker and Berenbaum2007), may be particularly appropriate for enabling caregivers to harness instrumental support from their networks (Dionne-Odom et al., Reference Dionne-Odom, Applebaum and Ornstein2018; Kent and Dionne-Odom, Reference Kent and Dionne-Odom2019). Interventions designed with self-management principles and based on the Caregiver Stress Model (Pearlin et al., Reference Pearlin, Mullan and Semple1990) and other similar theories can help caregivers identify and map out their sources of support by type (hands-on, informational, communication, financial, emotional, and self-care). This, in turn, provides caregivers with a way to tailor the support they receive (Reblin et al., Reference Reblin, Wu and Pok2017). Strategies like these can help caregivers and their network recognize and activate specific types of social support, like instrumental, which in turn may lead to lower burden and distress. Furthermore, as emphasized by the National Consensus Project Clinical Practice Guidelines on Quality Palliative Care, interdisciplinary palliative care teams should include professional social workers (Ferrell et al., Reference Ferrell, Twaddle and Melnick2018). Social workers may be best positioned to address both patient and family social factors, including helping family caregivers leverage the instrumental support they need. Finally, system-level interventions are needed, including those delivered to healthcare providers and other clinical staff to help raise awareness about support needs for caregivers and connect them to resources through the healthcare system and in the community. State-level policies to encourage, and in some cases require, hospitals to identify, prepare, and communicate with caregivers are being implemented (Ahern Gould, Reference Ahern Gould2018). Whether these policies will reduce caregiver distress remains to be seen.
One limitation of the present study was the lack of available data on other dimensions of social support, including emotional support (Feeney, Reference Feeney2004). Instrumental support may interact with emotional support receipt and provision (Morelli et al., Reference Morelli, Lee and Arnn2015). Assessing additional dimensions of social support is important for future study. The PROMIS measure is not specific to caregiving tasks; however, the goal of the current study was to elucidate caregivers’ views on the availability of help and support for themselves. Controlling for caregiving burden controlled for some confounding of the burden on distress; however, this variable had a moderate amount of missing data (n = 51). A sensitivity analysis removing the burden from the model yielded no change to the parameter estimate for instrumental support on distress; thus, the support and distress association appears to be robust. Additional caveates included limited sample size to examine differences by specific care recipient condition, which is critical for informing practice and future study, and some heterogeneity in our sample of caregivers who cared for individuals with diverse health problems. In addition, given that this study excluded paid caregivers, it is possible that some caregivers who received compensation for the care they provided, through Medicaid, the VA, or another payor, were excluded from the analysis. Finally, these data are cross-sectional; thus, associations do not imply causality. Strengths of the study include its population-based sampling, an uncommon opportunity in studies of caregivers. In addition, detailed questions on caregiving experience available through the caregiving module in HINTS V2 allowed for assessment of constructs germane to the caregiving experience. Finally, using two validated measures, the PROMIS instrumental support short form and the PHQ-4, allowed a more rigorous ascertainment of constructs of support and distress, superior to other studies reliant on single-item and more generic measures.
Conclusions
In this population-based, nationally representative study, we found that instrumental support has an inverse association with distress in informal caregivers of adults with serious health problems. Future work should use longitudinal data collection to determine the trajectory of support provision and the receipt of multiple dimensions of social support. In addition, palliative and supportive care interventions should focus on improving support for caregivers as a means of reducing distress. Instrumental support may buffer against poor health outcomes among caregivers. Findings from this study suggest that increasing access to and use of instrumental support could be an effective target for caregiver-focused interventions.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951520000036.
Funding
Dr. Dionne-Odom is funded by the National Institute of Nursing Research (R00NR015903) and the National Cancer Institute (R01CA229197). Dr. Ornstein is funded by the National Institute on Aging (K01AG047923, R01AG060967) and the National Palliative Care Research Center.
Disclaimer
The findings and interpretations in this manuscript are those of the authors and do not necessarily represent those of the National Cancer Institute or National Institutes of Health.







