Introduction
Laryngeal dysplasia is a relatively common pre-malignant condition with a high propensity for malignant transformation.Reference Karatayli-Ozgursoy, Pacheco-Lopez, Hillel, Best, Bishop and Akst1 Severe dysplasia, in particular, should not be underestimated, as malignant progression is described in approximately 30 per cent of these cases.Reference Weller, Nankivell, McConkey, Paleri and Mehanna2
The consensus statement published by Mehanna et al. in 2010 recommended a basic treatment strategy.Reference Mehanna, Paleri, Robson, Wight and Helliwell3 Carbon dioxide laser resection was advised. The use of laser for ablation or a vocal fold stripping procedure was not recommended. Regarding radiotherapy (RT), it states that ‘For primary lesions that have not been treated previously, radiotherapy should be offered with discretion only in rare circumstances and a very small number of patients, e.g. poor access for resection in a high grade lesion’. It also states that for patients with ‘Persistent or recurrent widespread severe dysplasia: Radiotherapy should be considered as an option by the multidisciplinary team and discussed with patients who have persistent or recurrent widespread severe dysplasia, especially in patients who continue to smoke’.Reference Mehanna, Paleri, Robson, Wight and Helliwell3
Radiotherapy provides an excellent outcome, with a lower progression rate to invasive carcinoma than superficial laser excision or stripping.Reference Sadri, McMahon and Parker4 However, close review revealed that the RT regimens have not been described in any dysplasia study, only in a handful of carcinoma in situ case series.Reference Small, Mittal, Brand, Shetty, Rademaker and Beck5–Reference MacLeod and Daniel8 The optimal RT regimen for dysplasia of the upper aerodigestive tract therefore remains unknown.
This study aimed to evaluate our experience of using RT with 55 Gy in 20 fractions, using modern RT technology (i.e. intensity-modulated RT), for treating high-grade dysplasia. Acute toxicity and the impact on quality of voice were evaluated. The overall role of RT in this pre-malignant condition of the larynx is also discussed.
Materials and methods
Patient selection
Prior to referral for RT, all patients were discussed in the head and neck multidisciplinary team meeting, on an individual basis, and the option of RT was agreed by the team.
Patient population
From 2013 to 2017 (a 5-year period), 14 patients (12 males and 2 females) were treated with RT. The median age of the patient cohort was 72 years (range, 51–82 years). All patients were histologically diagnosed with severe dysplasia according to the World Health Organization classification.Reference Barnes, Eveson, Reichart and Sidransky9 The mean follow-up time was 15.6 months (range, 5–40 months).
Five patients were originally diagnosed with mild or moderate dysplasia, and severe dysplasia developed during their pre-RT follow up. In three patients, there was recurrent disease following primary laser therapy (twice in each case), which was performed two to nine years prior to commencement of RT.
Treatment
All patients were treated with 6 MV photons using intensity-modulated RT (Figure 1). The clinical target volume was the whole larynx. A 5 mm circumferential margin was added to create the planning target volume. The treatment with a regimen of 55 Gy in 20 daily fractions was completed in all patients but one. In that one patient, the treatment was stopped at a dose of 44 Gy because of grade 4 dysphagia.
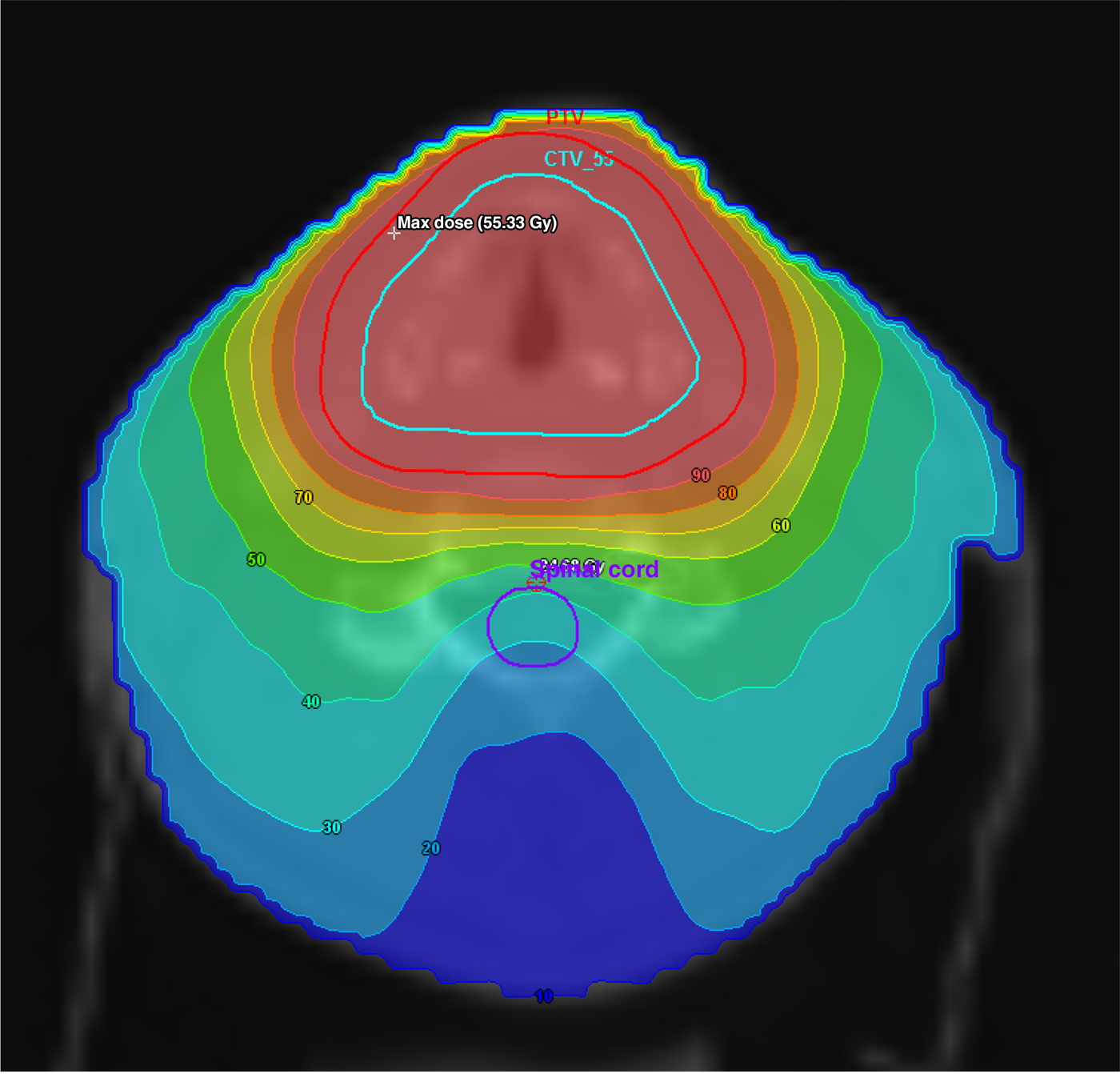
Fig. 1. Intensity-modulated radiotherapy (RT) to the larynx. The RT isodose lines are indicated. CTV = clinical target volume; PTV = planning target volume
Assessment
During the course of RT, all patients were assessed for acute toxicities on a weekly basis. Acute toxicities were documented as per the Common Terminology Criteria for Adverse Events, version 4.0.10
Voice evaluation was completed using a patient-reported outcome measure and an auditory perceptual measure (Voice Handicap Index-10, and Grade, Roughness, Breath, Asthenia, Strain (‘GRBAS’) scale, respectivelyReference Rosen, Lee, Osborne, Zullo and Murry11–Reference De Bodt, Wuyts, Van de Heyning and Croux14) before commencement and three months after RT completion.
Results
Complete response has been recorded in all patients. The mean follow-up duration was 15.6 months (range, 5–40 months); no cases of dysplasia recurrence or progression to invasive carcinoma were observed.
The acute toxicity of the treatment was significant. One patient developed grade 4 dysphagia after 16 fractions of RT, and treatment was terminated at the dose of 44 Gy. Three patients had grade 3 dysphagia, and required admission for nasogastric tube feeding and hydration. The acute RT-induced reactions settled within 6–12 weeks after treatment in all patients. No late toxicity has yet been observed in any of the patients. The quality of voice improved in all patients except one. The results are summarised in Table 1.
Table 1. Patients’ characteristics and treatment outcomes
* Indicates previous laser resection. Pt no. = patient number; VHI = Voice Handicap Index (10-item); GRBAS = Grade, Roughness, Breath, Asthenia, Strain scale; M = male; NA = not available; NG = nasogastric; F = female
Discussion
The treatment options in severe laryngeal dysplasia are: (1) surgical resection, most commonly cold steel or carbon dioxide laser excision, and to a lesser extent vocal fold stripping; (2) photodynamic therapy, which is very promising but still considered an experimental treatment;Reference Rigual, Thankappan, Cooper, Sullivan, Dougherty and Popat15, Reference Mimikos, Shafirstein and Arshad16 and (3) RT.
• Radiotherapy (RT) is an option to treat high-grade laryngeal dysplasia
• The optimal RT regimen is unknown
• The RT regimen of 55 Gy in 20 fractions is frequently used to treat early stage laryngeal cancer
• This regimen is effective in treating laryngeal dysplasia, but is associated with significant acute toxicity
• Dose de-escalation may be considered in the context of clinical trials
The position of RT in the treatment of early laryngeal cancer is well established and the optimal regimens of RT are well known. In laryngeal dysplasia, the situation is quite the opposite. Almost all published studies involving patients with laryngeal dysplasia also include patients with carcinoma in situ or even carcinoma in situ with microinvasion. From these studies’ findings, it is not possible to separate the RT dose fractionation and their outcome in these two cohorts of patients (with carcinoma in situ or severe dysplasia). Furthermore, patients in these studies were treated with obsolete techniques on old RT technology, such as cobalt-60 or orthovoltage treatment units.Reference Small, Mittal, Brand, Shetty, Rademaker and Beck5
The radiotherapy regimens used for the treatment varied significantly, even within individual studies. Garcia-Serra et al., in their series of 30 patients with carcinoma in situ, used an RT dose ranging from 56.2 to 75 Gy (median dose, 56.25 Gy), with dose per fraction ranging from 1.78 to 2.4 Gy (median, 2.25 Gy per fraction). The majority of patients were treated using cobalt units.Reference Garcia-Serra, Hinerman, Amdur, Morris and Mendenhall6 Le et al. reported on the treatment of 82 patients with carcinoma in situ using an RT dose ranging from 53 to 70 Gy (median dose, 64 Gy), with dose per fraction ranging from 1.5 to 2.4 Gy (median, 2 Gy per fraction).Reference Le, Takamiya, Shu, Smitt, Singer and Terris7 Again, patients were treated with a cobalt-60 or orthovoltage unit. In another study, MacLeod and Daniel reported on various RT regimens, including a thrice-weekly schedule, using a cobalt-60 unit, to treat patients with carcinoma in situ.Reference MacLeod and Daniel8
To the best of our knowledge, there has been no prospective trial to establish optimal RT dose fractionation in the treatment of severe laryngeal dysplasia.
The RT regimen of 55 Gy in 20 daily fractions has been widely used over many decades for treating the whole larynx in early stage carcinoma. It is quite an aggressive regimen associated with significant acute toxicity. In this current series of 14 patients, although functional voice outcome was good, the incidence of significant toxicity was considerably high. This occurred despite the use of modern RT technology. In view of this, it is worth considering a reduced dose – perhaps 52.5 Gy in 20 daily fractions, or even 50 Gy in 20 daily fractions – for treatment of this pre-malignant condition. However, this new dose fractionation must be evaluated in a prospective study.
The most valuable part of this study is the confirmation of excellent functional outcome concerning voice quality. In 9 out of 10 patients, a significant improvement of voice was observed three months after treatment.
The evidence concerning functional outcomes of treatment for laryngeal dysplasia is limited. The functional outcomes of surgery and RT have been discussed and compared for many years. The vast majority of published studies evaluated the treatment of early stage squamous cell carcinoma of the glottis. Therefore, it is unclear whether these data can be extrapolated to the case of laryngeal dysplasia. A recent publication by Huang et al. concluded that RT may be a better choice than laser surgery for a tumour stage T1a carcinoma of the glottis, as patients undergoing RT might have the advantage of increased maximum phonation time and decreased fundamental frequency.Reference Huang, Luo, Zhang and Liu17 This conclusion was based on a meta-analysis of 14 studies. Two previous meta-analyses reported similar findings, showing the trend of better functional outcomes with RT.Reference Higgins18, Reference Higgins, Shah, Ogaick and Enepekides19 These findings were confirmed by the only relevant randomised trial.Reference Aaltonen, Rautiainen, Sellman, Saarilahti, Makitie and Laranne20 However, one meta-analysis published in 2015 revealed no difference in functional outcome.Reference Greulich, Parker, Lee, Merati and Misono21
The current study has certain limitations. Firstly, it is a retrospective study conducted on a relatively small number of patients. Secondly, functional outcome data were not available for all treated patients.
Conclusion
The RT regimen of 55 Gy in 20 daily fractions using intensity-modulated RT is feasible for the treatment of severe laryngeal dysplasia, although the acute toxicity (dysphagia) is significant. Compared with other treatment modalities, functional voice outcome appears better three months after treatment, based on patient-reported outcomes and auditory perceptual measures. The de-escalation of RT dose should be considered in the context of a clinical trial.
Competing interests
None declared




