Introduction
The incidence of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infection is rapidly increasing. Most community-acquired MRSA infections involve localised soft tissue disease; however, severe, life-threatening infections have occasionally been described.
Nasal septal abscess with facial cellulitis caused by community-acquired MRSA is uncommon. We present such a case.
Case report
A 19-year-old woman presented to our emergency department with a two-day history of fever associated with severe nasal obstruction and the rapid progression of painful, erythematous swelling over the nasal dorsum, bilateral periorbital regions and cheeks (Figure 1). She had suffered occipital pain for five days prior to the development of the above symptoms. She had a history of allergic rhinitis but denied any previous nasal surgery, trauma, sinusitis, epistaxis, dental procedures or diabetes mellitus.

Fig. 1 Physical examination revealed severe swelling over the nasal dorsum, bilateral periorbital regions and cheeks.
Physical examination revealed bilateral bulging of the nasal septum which obstructed both nasal cavities.
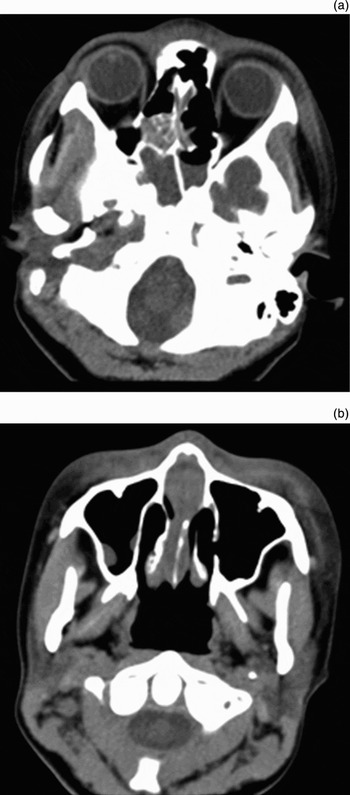
After an initial aspiration of 10 ml of purulent fluid, an urgent computed tomography (CT) sinus scan revealed opacified ethmoid and sphenoid sinuses with a thickened nasal septum and thickened facial soft tissues (Figure 2).

Fig. 2 Axial computed tomography scan of the sinuses, demonstrating (a) opacified ethmoid and sphenoid sinuses and (b) thickened nasal septum and facial soft tissues.
Gram staining of the aspirated fluid showed Gram-positive cocci. Amoxicillin with clavulanic acid was prescribed intravenously.
Under general anaesthesia, the patient underwent incision and drainage of the septal abscess and endoscopic drainage of the sinuses. The septal cartilage was found to be necrotic, with a residual limp, soft fragment, which upon histological examination showed micro-abscess formation. The periosteum was found to have separated from the bony septum, forming a tract leading from the abscess to the right side of the sphenoid sinus.
Bacterial culture of the aspirated fluid grew Staphylococcus aureus which was resistant to methicillin. The patient's antibiotics were changed accordingly, to vancomycin. Her facial swelling gradually resolved, but her suborbital soft tissue showed persistent bilateral necrotic change with hyperpigmentation (Figure 3). This gradually subsided over approximately one year.

Fig. 3 Persistent suborbital soft tissue necrosis was seen, despite marked regression of facial swelling, 4 days after surgical drainage.
There was no recurrence of disease over 18 months' follow up. However, a saddle nose deformity and posterior septal perforation, as a result of surgical drainage and debridement, were noted.
Discussion
Nasal septal abscess is rare, and is defined as a collection of pus between the nasal septum and the overlying mucoperichondrium or mucoperiosteum. Trauma is the most common cause of nasal septal abscess; less frequently, it is associated with nasal surgery, nasal furuncles, sinusitis, influenza and dental disease. Our patient self-medicated with analgesics for her occipital headache for five days, which may have allowed sphenoiditis to spread, resulting in septal abscess and facial cellulitis.
The most common presentation of nasal septal abscess is bilateral nasal obstruction. Other concurrent symptoms may include nasal pain, rhinorrhoea, fever and headache.Reference Lin and Huang1–Reference Huang, Chiang, Yang, Chao and Lee3 The pathophysiology of nasal septal abscess depends on its aetiology. Collins emphasised that isolated acute sphenoiditis can cause formation of a nasal septal abscess via direct subperiosteal extension along the anterior surface of the sphenoid bone, stripping the periosteum of the bony septum, to reach the subperichondrial surface of the quadrilateral cartilage.Reference Pang and Sethi2 This was probably the mechanism of abscess formation in our patient.
Huang and Hung reported that, of 601 patients with acute sinusitis, 16 (2.7 per cent) showed MRSA infection.Reference Huang and Hung4 In rare cases of nasal septal abscess, Staphylococcus aureus has been reported as the most common causative organism. However, the incidence of MRSA in cases of nasal septal abscess is unknown.Reference Lin and Huang1–Reference Huang, Chiang, Yang, Chao and Lee3 Although most community-acquired MRSA infections involve localised soft tissue disease, severe, fulminant infections have been described. Severe community-acquired MRSA infection is often seen in hitherto healthy young people, as seen in the reported case.Reference Crum5
• The incidence of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infections is rapidly increasing
• This report describes a case of nasal septal abscess caused by community-acquired MRSA
• If diagnosis and treatment of nasal septal abscess are delayed, potentially life-threatening complications may occur, including osteomyelitis, orbital and intracranial abscess, meningitis, and cavernous sinus thrombosis
• In this patient, a good clinical outcome was achieved by prompt surgical intervention and appropriate use of antibiotics
In cases of nasal septal abscess, a sinus CT scan is the most informative imaging investigation, and is usually obtained when the nasal septal abscess spreads to adjacent structures. Needle aspiration before incision and drainage can reduce the pressure within the abscess, which may decrease the risk of intracranial extension of infection; it also provides a specimen for bacterial culture.Reference Lin and Huang1–Reference Huang, Chiang, Yang, Chao and Lee3 Medical treatment should initially involve broad-spectrum intravenous antibiotics covering common pathogens; the antibiotic choice should be adjusted based on the results of culture and susceptibility tests. Delay in diagnosis and treatment may result in potentially life-threatening complications, including osteomyelitis, orbital and intracranial abscess, meningitis, and cavernous sinus thrombosis.Reference Lin and Huang1–Reference Huang, Chiang, Yang, Chao and Lee3 The clinical situation may be worse if the causative bacteria is virulent, as with MRSA. In our patient, a good clinical outcome was achieved through prompt surgical intervention and appropriate use of antibiotics.
In view of the rapidly increasing incidence of community-acquired MRSA infection, this report may serve to remind clinicians to remain vigilant for community-acquired MRSA as a cause of severe infection.