Introduction
Chronic otitis media is an infection of the middle-ear cavity lasting more than 12 weeks and associated with a permanent perforation of the tympanic membrane. It is usually present with intermittent ear discharge and a variable degree of hearing loss that is dependent on the size of the perforation.Reference Telian, Schmalbach, J.B and J.J1
The common causes of tympanic membrane perforation are infection, atelectasis, ventilation tube insertion and trauma.Reference Knapik and Saliba2 The term tympanoplasty was introduced and popularised by Horst Ludwig Wullstein and Frits Zollner in the early 1950s. It is the ‘gold standard’ surgery for the repair of tympanic membrane perforations with a success rate of more than 90 per cent in primary cases. The aim of surgery is to control recurrent ear infection, protection of the middle and inner ear, and to restore hearing.Reference House3
Different grafting materials have been used for the closure of tympanic membrane perforations, such as temporalis fascia, perichondrium, cartilage, periosteum, vein, dura mater, fat and scar tissue.Reference De Seta, Covelli, De Seta, Mancini and Filipo4 The most commonly used grafts are temporalis fascia and cartilage. Fascia has a low basal metabolic rate and is easily harvested in a large size from the same incision. Cartilage has slower metabolism, is resistant to infection and has considerable stiffness making it the preferred graft in poor Eustachian tube function, retraction pockets, infection, anterior perforations and revision surgery.Reference Sheehy and Anderson5,Reference Heermann, Heermann and Kopstein6
The classical techniques of tympanoplasty are the underlay and overlay techniques with different modifications, and refinements have been evolved over the last years.Reference Wehrs7 Each technique has its own advantages and disadvantages. Underlay tympanoplasty is the most widely used technique in which the graft is placed medially to the remaining tympanic membrane or malleus. In contrast, the more challenging overlay technique is usually reserved for anterior and total perforations or failed underlay surgery in which the graft is placed medially to the malleus handle and laterally to the tympanic membrane remnant after the squamous layer has been removed.Reference Kartush, Michaelides, Becvarovski and LaRouere8
The aim of the present study was to evaluate the difference in graft take rate after tympanoplasty between composite cartilage perichondrium and temporalis fascia grafts, and to compare success rates in adults with paediatric patient age groups, and overlay with underlay techniques.
Materials and methods
After obtaining approval from the institutional review board committee at our tertiary academic hospital, charts and medical records of consecutive patients who underwent type 1 tympanoplasty for tympanic membrane perforations between August 2011 and December 2019 were retrospectively reviewed. The following information was obtained: age, gender, side of surgery, site and size of perforation, myringosclerosis, middle-ear status (dry or wet, and presence or absence of adhesions), prior tympanoplasty, graft material (temporalis fascia or composite cartilage perichondrium), technique (underlay or overlay), success rate, reperforation after intact graft, status of the other ear, and the duration of follow up.
Tympanoplasty was performed for wet ears when they failed to dry after one month of antibiotic ear drops. Patients who had concomitant mastoidectomy, ossiculoplasty, history of previous ear surgery except for tympanostomy tubes and tympanoplasty, and follow up of less than six months were excluded.
The size of perforation was classified roughly according to percentage of perforation in relation to tympanic membrane: small (less than 50 per cent of tympanic membrane), large (more than 50 per cent) and subtotal (only annulus of tympanic membrane remained).
The overlay technique was selected in cases of anterior and subtotal perforations, while the underlay technique was performed in cases of small, large and subtotal perforations with a remnant of tympanic membrane not reaching the anterior annulus. Selection of cartilage graft was based on the tympanic membrane and middle-ear status with regard to wet ear, retraction, patient age less than seven years (more likely to have recurrent otitis media, otitis media with effusion and reperforation) and surgeon preference; otherwise, temporalis fascia graft was used.
All tympanoplasty procedures were performed by the same surgeon. The minimum amount of Spongostan™ soaked with ciprofloxacin ear drops was used for all cases to support the anterior medial surface of the graft. We routinely dissect tympanic membrane from the handle of malleus, and if myringosclerosis is close to the perforation edges, it is removed. Then the graft is placed under the malleus handle after making a slit in the fascia or resection of a small wedge in the cartilage. In overlay tympanoplasty, the skin of the anterior canal wall is completely removed and canaloplasty is performed in most cases, then the fascia is placed over the anterior annulus and under the malleus handle. To avoid anterior blunting, the fascia graft is brought only to the anterior sulcus on the annulus and not on to the anterior ear canal. The anterior canal skin is replaced keeping the acute angle between the graft and the anterior canal wall. At the end of surgery, the external canal was filled with Spongostan and finally a compressive ear dressing is applied for 24 hours.
Patients were discharged home on the next day after surgery on oral antibiotic and analgesia for one week. Antibiotic ear drops were prescribed after one week from surgery for three weeks.
Data were organised into groups according to the technique (underlay vs overlay), age of patients (paediatric patient less than 18 years vs adults) and graft type (temporalis fascia vs cartilage). The main outcome measures were tympanic membrane status (full graft take, perforation or reperforation) and the incidence of complications.
Success or full graft take was defined as intact healing of the tympanic membrane graft at least six months after surgery, and reperforation of the tympanic membrane was defined as perforation that occurred after six months.Reference Kartush, Michaelides, Becvarovski and LaRouere8
The Mann–Whitney U test was used for non-parametric data analysis. For categorical data analysis, the chi-square test or Fisher's exact test was used as appropriate. A p-value of less than 0.05 was considered statistically significant.
Results
A total of 198 patients (208 ears) who underwent type 1 tympanoplasty and met our inclusion and exclusion criteria were included in this study. The average age was 32.7 years (standard deviation (SD) ± 16; range, 4–74 years) with 108 males and 100 females. Right side tympanoplasty was performed in 85 ears (40.9 per cent), left side tympanoplasty was performed in 103 ears (49.5 per cent) and bilateral tympanoplasty was performed in 20 ears (9.6 per cent). Dry ear was present in 171 cases (82 per cent), myringosclerosis was present in 141 cases (67.8 per cent), middle-ear adhesions were present in 108 cases (52.7 per cent) and the contralateral side was normal in 160 cases (76.9 per cent). Overall, full graft take was achieved in 200 ears (96.2 per cent) in a mean follow up of 40.6 months (± 28.6; range, 6–102 months; Table 1).
Table 1. Patients' demographic features and clinical characteristics

Thirty-seven patients had wet ear at time of surgery. For these patients, cartilage tympanoplasty was performed in 22 cases (59.5 per cent) and an underlay technique was performed in 32 cases (86.5 per cent). Interestingly, full graft take was achieved in all cases at an average follow up of 44 months (range, 6–99 months).
The success rate of tympanoplasty was higher in adults compared with paediatric patients (97.5 per cent vs 92.25, respectively) but the difference was insignificant. Similarly, residual perforation was insignificantly higher in paediatric patients compared with adults (7.8 per cent vs 2.5, respectively). In addition, we did not find significant difference in the other examined parameters for both groups (Table 2). Reperforation was seen in 2 paediatric patients. One of them was 7 years old and had subtotal perforation and underwent cartilage tympanoplasty; after 8 months she had small posterior reperforation (close to the posterior rim of the cartilage) following acute otitis media. The other patient was 12 years old and had large reperforation after 10 months of fascia tympanoplasty and underwent revision cartilage tympanoplasty.
Table 2. Comparison of tympanoplasty between adults and paediatric patients
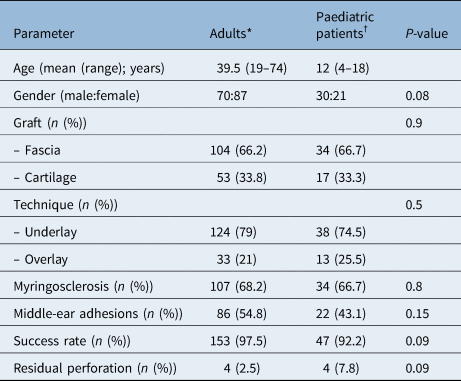
*n = 157; †n = 51
Myringosclerosis was found in 105 cases (76 per cent) of temporalis fascia group, while it was found in 36 cases (51 per cent) of cartilage group. This difference was statistically significant (p < 0.001). There was a higher but insignificant graft take rate in the cartilage group compared with the fascia group (97.1 per cent vs 95.7 per cent, respectively; Table 3).
Table 3. Comparison of tympanoplasty between fascia and composite cartilage perichondrium grafts

*n = 138; †n = 70
All cases of overlay tympanoplasty had full graft take (success rate 100 per cent); however, 4 cases (8.7 per cent) had anterior blunting. In the underlay group, successful graft take was achieved in 154 cases (95 per cent). This difference was statistically insignificant (Table 4).
Table 4. Comparison of tympanoplasty between underlay and overlay techniques
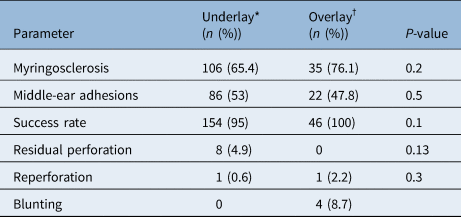
*n = 162; †n = 46
Discussion
Repair of tympanic membrane perforation by performing tympanoplasty leads to significant benefits including: prevention of recurrent ear infections and otorrhoea, hearing improvement, protection of the middle ear, ease of hearing aid usage, and elimination of water precautions during showering and swimming.Reference Sheahan, O'Dwyer and Blayney9,Reference Emir, Ceylan, Kizilkaya, Gocmen, Uzunkulaoglu and Samim10
The reported success rates of tympanoplasty ranged from 60 to 99 per cent in adults and 35 to 94 per cent in children.Reference Sarkar, Roychoudhury and Roychaudhuri11 Many factors have been reported to influence the success rates of tympanoplasty, including the age of the patient, site and size of perforation, the presence of infection at the time of surgery, graft material, status of the opposite ear, and surgical technique.Reference Emir, Ceylan, Kizilkaya, Gocmen, Uzunkulaoglu and Samim10,Reference Adkins and White12
Herein we present our experience with type 1 tympanoplasty. The results of this study are clinically significant. To the best of our knowledge, this is the first study in the literature to report results of tympanoplasty by comparison of adults, temporalis fascia graft and underlay technique with paediatric patients, cartilage and overlay technique, respectively. Overall, we achieved excellent results with a 96 per cent graft take rate at an average follow up of 41 months. We agree with other authors that surgical skills and experience, and case by case selection of proper approach and graft are more important factors for success than clinical variables.Reference Cabra and Moñux13
Overlay and underlay tympanoplasty
The underlay and the overlay procedures are the most popular methods of grafting. The underlay technique has a high success rate, and it is preferred for posterior perforations with no risk of lateralisation. It is relatively simple, but anterior canal bulge can prevent adequate visualisation of the anterior middle-ear cavity and may result in anterior falling of the graft in cases of anterior perforations. Overlay tympanoplasty is ideal for large, subtotal and anterior perforations. It provides superior exposure with a high success rate; however, it is more complex, takes longer time, and has a risk of anterior blunting or graft lateralisation.Reference Kartush, Michaelides, Becvarovski and LaRouere8
The reported success rates in literature vary between authors. Surgical experience in either technique may have influenced these results. Surgeons who reported their experience in a single technique, either in underlay or overlay tympanoplasty, achieved a superior success rate; however, in comparative studies, authors reported almost identical or higher success rate in favour of the overlay procedure.Reference Rizer14,Reference Singh, Rai, Bandyopadhyay and Gupta15
Sheehy and AndersonReference Sheehy and Anderson5 reported results of 472 tympanoplasties performed by 14 otologists. Lateral grafting technique with fascia graft was used in 273 cases. A successful graft take was achieved in 97 per cent. Healing problems (anterior blunting or lateral healing, persistent epithelitis of membrane and epithelial pearl) occurred in less than 2 per cent of the cases. Similarly, Ryan and Briggs,Reference Ryan and Briggs16 Albera et al.Reference Albera, Ferrero, Lacilla and Canale17 and Angeli et al.Reference Angeli, Kulak and Guzmán18 reported high success rates of 100 per cent, 93 per cent and 91 per cent, respectively.
Anterior graft blunting is the main problem in the overlay technique. It has been reported to affect 0–10 per cent of cases.Reference Kartush, Michaelides, Becvarovski and LaRouere8,Reference Emir, Ceylan, Kizilkaya, Gocmen, Uzunkulaoglu and Samim10,Reference Rizer14,Reference Jung and Park19 Many modifications have evolved to overcome this complication. Jung and ParkReference Jung and Park19 reported a 1 per cent blunting in 100 mediolateral graft tympanoplasty procedures. Furthermore, anterior blunting was not seen in 234 patients who underwent three-point fix tympanoplasty in which anterior canal skin elevation beyond 4 o'clock was avoided.Reference Shim, Kim, Kim and Moon20
Emir et al.Reference Emir, Ceylan, Kizilkaya, Gocmen, Uzunkulaoglu and Samim10 reported a success rate of 88 per cent in 607 underlay grafts. They found a significantly higher success rate in males, with perforation less than 50 per cent and with senior surgeons performing the procedure. No significant difference was found between dry ears and discharging ones (88 per cent vs 88.6 per cent, respectively). In another study, Barake et al.Reference Barake, El Natout, Bassim and El Natout21 obtained a graft take rate of 99.3 per cent in 1100 patients who underwent loop underlay tympanoplasty for anterior, subtotal and total tympanic membrane perforations.
In a prospective randomised study of 60 cases with subtotal or large perforations, a success rate of 93.3 per cent in both techniques was achieved, and blunting was found in 6.6 per cent of overlay grafts.Reference Singh, Rai, Bandyopadhyay and Gupta15 In contrast, RizerReference Rizer14 reported a success rate of 95.6 per cent in 554 overlay grafts and 88.8 per cent in 158 underlay grafts.
There is no ‘gold standard’ technique for all tympanic membrane perforations. The surgeon should select the appropriate technique based on the site and size of the perforation. In our study, we obtained an anatomical success rate of 100 per cent for 46 overlay tympanoplasties; however, blunting was seen in 8.9 per cent of cases. Although, blunting is high in our series, these results were at the beginning of our experience in overlay technique. In underlay technique, we achieved a success rate of 95 per cent with no statistically significant difference between both techniques. The overlay tympanoplasty is more difficult to master, it gives greater exposure and a higher graft success rate. But blunting and lateral healing of the graft may occur until the technique is mastered. Canaloplasty, avoiding placement of the fascia on the anterior canal wall and placement of the fascia under the malleus handle decrease the risk of blunting.Reference Sheehy and Anderson5
Cartilage and fascia grafts
Temporalis fascia represents the most widely used grafting material; however, in recent years cartilage graft has gained wide popularity.Reference Yetiser and Hıdır22 Previous studies reported a graft take rate for cartilage tympanoplasty varying between 82 and 100 per cent.Reference Yetiser and Hıdır22,Reference Callioglu, Ceylan, Kuran, Demirci, Tulaci and Caylan23
Iacovou et al.Reference Iacovou, Vlastarakos, Papacharalampous, Kyrodimos and Nikolopoulos24 conducted a literature review comparing the success rate of cartilage with temporalis fascia grafts in type 1 tympanoplasty. They found that the mean graft integration rate in the cartilage group was 92.4 per cent and 84.3 per cent in the fascia group. The difference was statistically significant (p < 0.05). They also found that graft reperforation was significantly higher in fascia compared with cartilage groups (15.5 per cent vs 7.6 per cent, respectively). Another study conducted by Callioglu et al.Reference Callioglu, Ceylan, Kuran, Demirci, Tulaci and Caylan23 reported a statistically significant difference in favour of cartilage graft (95.2 per cent vs 80 per cent, p = 0.013). In a randomised controlled study of 123 patients, Cabra and MoñuxReference Cabra and Moñux13 also found significant difference in success rates between cartilage (82 per cent) and fascia groups (64.4 per cent). In contrast, other authors reported higher but insignificant differences in success rate between cartilage and fascia grafts.Reference Yetiser and Hıdır22,Reference Gamra, Mbarek, Khammassi, Methlouthi, Ouni and Hariga25
The differences in reported success rates may be attributed to the differences in surgical experience, success criteria, techniques used, duration of follow up and the number of cases. In the present study, we found that graft take rate was insignificantly higher in favour of cartilage graft (97.1 per cent vs 95.7 per cent) which coincided with previously reported rates.
Paediatric patient and adult tympanoplasty
Graft take rates have been reported from 60 to 99 per cent in adults, whereas a 35 to 94 per cent success rate has been reported in children. Some authors do not recommend tympanoplasty under the age of 7 because of the possibility of post-operative middle-ear effusion, recurrent otitis media and higher risk of reperforation.Reference Sheehy and Anderson5,Reference Sadé, Berco, Brown, Weinberg and Avraham26,Reference Podoshin, Fradis, Malatsakey and Ben-David27 In contrast, many authors did not find a significant difference in success rate in regard to age.Reference Emir, Ceylan, Kizilkaya, Gocmen, Uzunkulaoglu and Samim10,Reference Albera, Ferrero, Lacilla and Canale17,Reference Angeli, Kulak and Guzmán18,Reference Callioglu, Ceylan, Kuran, Demirci, Tulaci and Caylan23,Reference Zhan, Rawlins, Mattingly, Malhotra and Adunka28–Reference Umapathy and Dekker32
In a review of 78 paediatric patient lateral graft tympanoplasty procedures, Zhan et al.Reference Zhan, Rawlins, Mattingly, Malhotra and Adunka28 reported a successful closure of the tympanic membrane in 97.4 per cent and 92.6 per cent of cases after a follow up of 6 months and 1 year, respectively. They did not find a statistically significant difference in graft failure in regard to age, perforation size, history of bilateral Eustachian tube dysfunction, presence of a learner surgeon, myringosclerosis, presence of syndromic features or history of prior tympanoplasty.
Chandrasekhar et al. published a 10-year experience of paediatric patient tympanoplasty procedures from the House Ear Clinic and reported a failure rate of 7.5 per cent. Overlay fascia graft was used in 86 per cent of 268 cases. Similarly, they did not find any correlation between graft failure and age at surgery, size of perforation, disease status of the contralateral ear or history of adenoidectomy.Reference Chandrasekhar, House and Devgan29 Umapathy and DeckerReference Umapathy and Dekker32 found that graft take rate was 90 per cent in children younger than 14 years with no significant difference between children younger than 8 years (4–8 years) and an older group (9–14 years).
In the present study of 9 years, we achieved a higher but insignificant success rate in adults compared with paediatric patients (97.5 per cent vs 92.2 per cent, respectively). In addition, no statistically significant difference was found in regard to gender, myringosclerosis, size of perforation, presence of middle-ear adhesions, contralateral ear (diseased or normal), graft (fascia or cartilage) and technique (underlay or overlay).
We select the technique based on the site of the perforation; the overlay was used mainly for anterior perforations reaching the annulus. However, graft selection was based on the presence or absence of retraction; cartilage graft was used for retracted tympanic membrane. We agree that an experienced surgeon can obtain excellent results by performing either the overlay or underlay techniques and by using either fascia or cartilage grafts.Reference Sheehy and Anderson5,Reference Lin and Messner30
Traditionally, it is advised to perform tympanoplasty on dry ear because working on inflamed and thick middle-ear mucosa is more difficult with more bleeding and infection may increase the failure rate.Reference Sheehy and Anderson5 In 37 patients, the ear did not become dry despite long-time use of antibiotic ear drops. In these patients, we obtained a full graft take in 35 patients (95 per cent) and residual perforation was found in 2 cases with no significant difference between wet and dry ears. No significant association was also reported by many other studies.Reference Albera, Ferrero, Lacilla and Canale17,Reference Iacovou, Vlastarakos, Papacharalampous, Kyrodimos and Nikolopoulos24,Reference Shishegar, Faramarzi and Rashidi Ravari33
• Tympanic membrane perforation repair by performing tympanoplasty leads to significant benefits for the patient with high success rates
• The influence of age, graft material and technique are still controversial
• In this study, we compared the success rate of tympanoplasty in adults and paediatric patients, cartilage with fascia and underlay with overlay techniques
• We did not find any statistically significant difference between studied clinical variables
• It seems that surgical experience is the main factor in achieving high graft take rate regardless of technique or graft
The limitations of this study are: (1) it is retrospective, (2) a relatively small number of patients were in comparison groups, (3) the selection bias between the techniques (overlay vs underlay) and grafts (cartilage vs fascia). However, we think this work is of great value because it analysed different variables influencing success rates in tympanoplasty.
Our results show that age (paediatric patients and adults), technique (underlay or overlay) and graft type (fascia or cartilage) have no statistically significant deference on success rate of tympanoplasty. Similarly, gender, size of perforation, wet ear, myringosclerosis, middle-ear adhesions and opposite ear status seem to have no significant influence on graft take rate. We believe that an experienced otologist can achieve excellent results regardless of technique or graft and irrespective of clinical variables.
Competing interests
None






