Introduction
The extended endoscopic approach to clival tumours has become an increasingly adopted alternative to traditional open approaches with comparative levels of tumour resection.Reference Jho1–Reference Fraser, Nyquist, Moore, Anand and Schwartz4 The endoscopic transclival approach offers the advantage of a direct route for complete tumour excision with improved visualisation, while avoiding the need for brain or brainstem retraction. In addition, as resection is typically conducted in a medial to lateral direction, the morbidity associated with mobilisation of neurovascular structures is potentially reduced. Despite these advantages, the risk of cerebrospinal fluid (CSF) leak remains a significant challenge as this approach gains more widespread acceptance.Reference Fraser, Nyquist, Moore, Anand and Schwartz4–Reference Stippler, Gardner, Snyderman, Carrau, Prevedello and Kassam7
A review of studies examining the endoscopic transclival approach for chordoma resection revealed a 0–33 per cent incidence of post-operative leak.Reference Fraser, Nyquist, Moore, Anand and Schwartz4–Reference Dehdashti, Karabatsou, Ganna, Witterick and Gentili8 Although comparable to the incidence in open approaches, this variable morbidity presents a true obstacle for an expeditious and successful clinical outcome. Also, as we continue to extend this approach to encompass a broader range of pathologies that concern the clival region, including those with potential intradural extension, our ability to reconstruct various skull base defects becomes increasingly paramount to the success of surgery. With an increasing number of cases performed at tertiary institutions, we have witnessed a decrease in the rate of leaks in other approaches, including the transsellar, transplanum and transcribriform approaches, since the adoption of multi-layer reconstruction with a pedicled nasoseptal flap.Reference Adappa, Learned, Palmer, Newman and Lee9–Reference Pinheiro-Neto, Prevedello, Carrau, Synderman, Mintz and Gardner12 Unfortunately, this success does not seem to be as easily attainable with the transclival approach. Factors that have been linked to this higher leak rate with the transclival approach include tumour location (intradural vs extradural), tumour size, type of skull base reconstruction and use of a lumbar drain.Reference Fraser, Nyquist, Moore, Anand and Schwartz4–Reference Dehdashti, Karabatsou, Ganna, Witterick and Gentili8, Reference Oostra, van Furth and Georgalas13–Reference Sanborn, Kramarz, Storm, Adappa, Palmer and Lee15
Our objective in this article was to present our experience with the extended endoscopic approach to clival pathology with specific focus on skull base reconstruction and CSF leak. We sought to examine the reasons that make reconstruction in this region more challenging than elsewhere and hoped to shed light on technical nuances that can help prevent this complication.
Patients and methods
Patients were selected from a consecutive series of 37 patients undergoing extended endoscopic endonasal approaches for skull base tumours performed by the senior authors (J L, J P, N A and J N) between June 2008 and July 2012. Nine of these patients underwent an extended endoscopic transclival approach. Patients were prospectively registered in a database in which patient age, pathology, tumour location, intradural vs extradural, tumour size (pre-operative maximal diameter), endoscopic approach, pre-operative symptoms, reconstruction material and use of a lumbar drain were recorded. We did not record gender as the focus of our study was not the prevalence or incidence of skull base tumours. After the completion of a short hospital course, post-operative incidence of leak was also recorded. Exclusion criteria included only tumours without extrasellar extension. We obtained institutional review board approval from the Hospital of the University of Pennsylvania prior to initiation of this study. All patients gave their written, informed consent for their clinical data to be used for research purposes.
Transclival operative approach
At our institution, an otolaryngology and neurosurgery team approach is used for all extended endoscopic endonasal approaches. The use of stereotactic image guidance with magnetic resonance and computed tomography imaging is used in all cases. For tumours involving the superior portions of the clivus, exposure is conducted starting at the sella and continuing inferiorly. Locations of neurovascular structures, including the carotid arteries, are confirmed using both image guidance and endoscopic Doppler sonography. For tumours involving the lower two-thirds of the clivus, an inverted, U-shaped flap of pharyngeal mucosa, buccopharyngeal fascia and pre-vertebral musculature is created below the sphenoid sinus. Alternatively, for low-lying clival lesions, a midline incision is made and a laryngeal retractor is inserted in the oropharynx to keep the mucosa retracted. The clival bone can then be judiciously drilled to expose the dura while keeping the carotid arteries as the lateral limitation. Once the dura is exposed widely, intradural dissection based on tumour location is conducted in a medial to lateral direction taking care to identify neurovascular structures including the basilar artery and abducens nerve.
Skull base reconstruction
For intradural tumours, we typically use a fat graft to obliterate the dead space, fascia lata as an inlay within the dural opening or DuraGen (Integra Life Sciences, Plainsboro, New Jersey, USA), with overlay vascularised nasoseptal flap(s). The layers are held in place with the use of TISSEEL (Baxter International Inc., Deerfield, Illinois, USA) or DuraSeal (Covidien, Dublin, Ireland) to ensure watertight closure. Finally, surgical glove fingers with Pope sponges are placed bilaterally against closure for further bolstering. This is followed by placement of bilateral rubber nasopharyngeal airway tubes or nasal trumpets. The glove finger packs are removed at the first post-operative visit (approximately one week post-operatively). Lumbar drains were initially placed in many of our cases, but given the paucity of literature regarding the prevention of CSF leaks, our institution stopped using lumbar drains in all expanded skull base cases. If placed, they are typically drained at a rate of 5 ml/hour for 2–3 days and subsequently removed when appropriate.
Statistical analysis
Descriptive statistics included frequency, mean and median calculations using Microsoft Excel (Microsoft, Redmond, Washington, USA). Statistical analysis included the development of 2 × 2 contingency tables. Because of the small sample sizes, Fisher's exact tests were used to test the association between the classifications. Stata 10 (College Station, Texas, USA) was used to calculate the statistics. P values ≤ 0.05 were considered statistically significant.
Results
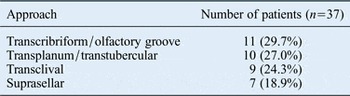
From June 2008 to July 2012, we identified 37 consecutive patients undergoing extended endoscopic endonasal approaches for skull base tumours. The mean age overall was 47.9 years (range, 5–77 years). The mean tumour size (pre-operative maximal diameter) was 27 × 21 mm (range, 14–45 × 3–41 mm). The tumour pathology encountered is detailed in Table I. The tumour locations are detailed in Table II. The supratentorial approach was used in 28 patients, while 9 patients underwent an infratentorial approach. The overall incidence of post-operative CSF leak was 10.8 per cent (4 patients). Three (75 per cent) of these patients who had a post-operative CSF leak underwent an infratentorial dissection with a transclival approach (p < 0.05). The use of a lumbar drain did not show a statistically significant correlation with CSF leak (p > 0.05).
Table I Tumour pathology

Table II Skull base approach
Transclival approach
The transclival approach was used in nine patients. Table III provides a clinical summary of the included transclival approach patients. For this approach, the mean age was 44.9 years. The mean tumour size (pre-operative maximal diameter) recorded in 7 of the 9 patients was 28 × 22 mm (range, 15–45 × 10–28 mm). Of the 9 patients with clival pathology, 5 (56 per cent) were considered to have an intradural component while 4 (44 per cent) had solely extradural tumours. All 3 (33 per cent) clival tumour patients who had a CSF leak underwent an intradural dissection (p < 0.05). The patients with extradural clival pathology (two chordomas, one chondrosarcoma and one osteosarcoma) had a 0 per cent incidence of post-operative CSF leak. In addition, tumour size (pre-operative maximal diameter) was not significantly different in the cases with a transclival approach when compared to other approaches.
Table III Characteristics of nine patients undergoing the endoscopic endonasal transclival approach

*Tumour size was not accurately determined for various reasons, including location, bony invasion and imaging modalities. CSF = cerebrospinal fluid
Discussion
The extended endoscopic approach offers several advantages when compared to traditional open approaches for clival pathology. Despite decreased morbidity, the risk of CSF leak remains a significant challenge.Reference Bohman, Stein, Newman, Palmer, Adappa and Khan14–Reference Lee, Ramakrishnan, Chiu, Palmer and Gausas17 In our series of 37 patients undergoing an extended endoscopic approach for skull base tumours, the risk of CSF leak was significantly increased when a transclival approach was used. This increased risk did not correlate with lumbar drain use or tumour size. However, all post-operative CSF leaks were encountered in transclival resections that had a significant intradural component.
Current studies regarding the extended endoscopic approach for clival tumours pertain largely to clival chordomas that are typically extradural with a limited intradural component.Reference Hwang and Ho18 The CSF leak rate in these series ranges from 0 to 33 per cent and is dependent on the intradural extent and use of a multi-layer reconstruction with a vascularised nasoseptal flap.Reference Fraser, Nyquist, Moore, Anand and Schwartz4–Reference Dehdashti, Karabatsou, Ganna, Witterick and Gentili8 Most authors agree that the use of a multi-layer closure with a vascularised nasoseptal flap, drastically reduces the rate of CSF leak to near 0.Reference Fraser, Nyquist, Moore, Anand and Schwartz4, Reference Fraser, Nyquist, Moore, Anand and Schwartz6–Reference Dehdashti, Karabatsou, Ganna, Witterick and Gentili8, Reference Solares, Grindler, Luong, Kanowitz, Sade and Citardi19 Our experience with clival chordomas was similar to these reports. The four patients with extradural clival pathology (two chordomas, one chondrosarcoma and one osteosarcoma) closed in a multi-layer fashion with a vascularised nasoseptal flap, had a 0 per cent incidence of post-operative CSF leak. The one patient with a chordoma with intradural extension also did not have a CSF leak. However, 75 per cent of our patients (3 out of 4 patients) with a largely intradural, infratentorial component had a post-operative CSF leak. Although our study is limited by the small sample size, especially with regard to intradural pathology, this is the first study to our knowledge that documents a challenge with the transclival intradural approach. Despite the relative rarity of intradural pathology in this region, a larger study is needed to investigate the challenges highlighted by our cohort.
• The extended endoscopic approach to clival tumours has become an accepted alternative to traditional open approaches
• Much of the current literature pertains to extradural clival dissection, where the use of a multi-layer closure with a vascularised nasoseptal flap drastically reduces the rate of cerebrospinal fluid (CSF) leak
• Our study found that 75 per cent of our patients (3 out of 4 patients) with a largely intradural infratentorial component had a post-operative CSF leak
• Although limited by sample size, this is the first study to our knowledge that documents a challenge with the transclival intradural approach
• We suggest that the observed increased incidence of CSF leak following the transclival approach is secondary to the higher chance of graft migration, difficulty with graft bolstering and the dynamic qualities of the region during speech and swallowing
We suggest that the observed increased incidence of CSF leak following reconstruction of the skull base after using the transclival approach reflects the unique challenges that this region presents. First, the wider bony resection and larger dural opening make it difficult to place a watertight intradural (inlay) graft to withstand the subarachnoid CSF pulsations. Despite the use of autologous fat to effectively reduce the dead space, we feel that, without an effective intradural seal, the graft has a higher chance of migration. Second, we found that although the vascularised nasoseptal flap would effectively cover the defect, it was technically challenging to ensure a tight seal against the clival defect. We attributed this to the flap's extended arc of rotation and the inability to reliably buttress this area. Third, unlike other areas along the skull base, the transclival approach demands a relatively wide and inferior–posterior septectomy. This, in combination with the already larger surface area of the nasopharynx, makes it challenging to bolster the flap against the defect with a pack or balloon bolster. Finally, the clival reconstruction, unlike reconstruction in other regions, is subjected to the dynamic qualities of the pharyngeal and palatal movement. The lateral aspects of the reconstruction are subject to continuous and seemingly involuntary movement of the pharyngeal musculature. Similarly, the entire reconstruction is subject to the closure and elevation of the palate during speech and swallowing.
Conclusion
The extended endoscopic approach technique has advanced significantly since its initial description. Many of these advancements, including the advent of the vascularised nasoseptal flap, have helped us tremendously in improving post-operative CSF leak rates. Despite this, intradural transclival approaches continue to pose a challenge. Further investigation is necessary to aid in technique improvements to facilitate the unique challenges associated with transclival approaches.





