Published online by Cambridge University Press: 01 March 2004
The retrograde amnesia of patients with memory loss related to rupture and surgical repair of anterior communicating artery (ACoA) aneurysms is compared with the retrograde amnesia of temporal amnesic patients and nonamnesic control participants. Two tests which focus on popular culture but which differ according to extent of news exposure and the cognitive processes necessary for task performance were used to measure retrograde memory. ACoA patients demonstrated more significant retrograde memory problems than did nonamnesic controls; however, the severity and pattern of their memory loss was less severe than that seen in association with temporal amnesia. Different factors influenced the remote memory loss of respective groups: ACoA patients' problems were related to impaired lexical retrieval whereas temporal amnesic patients had problems secondary to both retrieval and storage deficits. (JINS, 2004, 10, 221–229.)
The effect of basal forebrain and prefrontal damage on cognitive functions has been investigated in patients who have sustained rupture and who have undergone surgical repair of anterior communicating artery (ACoA) aneurysms (DeLuca & Diamond, 1995; Diamond et al., 1997). Many studies underscore neuropsychological deficits characterized by amnesia, executive impairments, and confabulation. While there is consensus that rupture and surgical repair of ACoA aneurysms adversely affect memory, there is less agreement regarding the pattern of memory deficits observed in association with this condition. In some studies ACoA patients have performed disproportionately worse on tasks of free recall versus recognition. Such observations have led investigators to speculate that the mnestic problem of the ACoA patient is a consequence of deficient strategic retrieval. This contrasts with the pattern of memory loss seen in patients with hippocampal damage who may have retrieval deficits but who also have problems with consolidation.
Studies that have focused specifically on retrograde amnesia in ACoA patients have produced mixed results. Alexander and Freedman (1984) reported substantial variability in the remote memory profiles of ACoA patients. In their study the majority of patients demonstrated retrograde amnesias that were quite brief, lasting from 1 week to 3 months. However, 3 of their 11 patients had extensive retrograde amnesias of approximately 20 years. Vilkki (1985) reported that ACoA patients had difficulty recalling events predating surgery. This observation was based on anecdotal evidence, however, and systematic investigation of retrograde amnesia was not conducted. Parkin et al. (1988) found that patient J.B. did not have a significant retrograde amnesia on a task measuring recognition of famous faces. In another single case study Babinsky et al. (1997) reported that patient P.E. recalled personal events and famous faces whereas he was amnestic for famous events.
The most comprehensive study of retrograde amnesia with ACoA patients was conducted by Gade and Mortensen (1990). They compared 4 patient groups: patients with amnesia due to ACoA aneurysms, other amnesic patients, demented patients, and nonamnesic control participants. ACoA patients, like amnesic and demented patients, demonstrated retrograde amnesia on a public events questionnaire and they displayed a temporal gradient reminiscent of that seen in Wernicke Korsakoff syndrome. All groups benefited substantially from cuing.
Several factors may account for observed disparities in reports regarding the memory abilities of patients with ACoA aneurysms. There is a great deal of neuropathological heterogeneity in the aftermath of ACoA aneurysm rupture and surgical repair. Differences in the distribution of neural damage and associated neurocognitive profiles may confound analyses of retrograde amnesia. Previous work has shown that retrograde amnesia varies in association with lesion location and size. Patients with extensive neocortical damage related to conditions such as encephalitis and dementia have dense retrograde amnesias encompassing many decades (Albert et al., 1981; Cermak & O'Connor, 1983; Sagar et al., 1988; Wilson et al., 1981) whereas amnesics with more circumscribed damage have limited retrograde amnesia (Kopelman et al., 1999; Milner, 1972; Rempel-Clower et al., 1996).
A systematic investigation of the neural substrates of retrograde amnesia was conducted by Kopelman et al. (1999) who examined profiles of retrograde amnesia in patients with diencephalic, temporal, and frontal brain lesions using tests of autobiographical and semantic memory as well as a public events questionnaire. In this study, patients with diencephalic damage due to Korsakoff's syndrome had significant temporally graded retrograde amnesias whereas patients with focal diencephalic damage did not. Temporal lesion patients had extensive retrograde amnesias with flat temporal gradients on all tests. All groups responded to cuing, a finding that was interpreted as consistent with retrieval problems. This study supports the idea that distribution of neural damage affects the nature and severity of retrograde amnesia.
The relationship between damage to frontal systems and retrograde amnesia has also been investigated. Kopelman et al. (1999) found that patients who underwent bilateral tractomies for treatment of psychiatric ailments had extensive retrograde amnesias. D'Esposito et al. (1996) investigated the association between retrograde amnesia and performance on tasks of executive abilities thought to be mediated by frontal systems. They found that ACoA patients had remote memory problems in the early recovery phase but that these abated as executive abilities improved.
Another issue that complicates studies of retrograde amnesia concerns differences between tasks used to assess remote memory. Memories from the past vary along many dimensions. Studies with non-amnesic control participants have shown that age of acquisition, extent of exposure, personal meaningfulness, and emotional salience affect access to remote memories (Bahrick, 1984; Conway et al., 1992; Rubin & Schulkind, 1997). Investigations with amnesics have shown that the nature of the retrieval cue (Gade & Mortensen, 1990; Kopelman et al., 1999; Warrington & McCarthy, 1988) and differences in item content (DeRenzi et al., 1987; O'Connor et al., 1992) exert differential effects on remote memory.
The present study was designed to elucidate patterns of remote memory loss in ACoA patients with two tests that were constrained in terms of item content (i.e., popular culture) but that differed according to modality of presentation (sentences vs. photographs), extent of exposure (prolonged vs. transient), and nature of retrieval cues (lexical cues vs. forced choice recognition). The Famous Faces Test (FFT; Albert et al., 1979) includes photographs of famous people who were in the news for prolonged time periods. It is likely that memories for these individuals are reinforced over multiple exposures to the extent that they become embedded in semantic memory. The Transient News Events Test (TNET; O'Connor et al., 2000) focuses on recall and recognition of items that were intensively covered in the news media for only a limited time period. TNET items are less well rehearsed and have fewer semantic associations; hence, it is likely that they require more effort at time of retrieval.
Based on inherent differences between our tasks of retrograde amnesia and neuropathological differences between our patient groups, our predictions were as follows. In light of the differences between our tests with regard to item exposure, we expected that all groups would show enhanced recall of FFT versus TNET items. Second, we expected that the retrograde memory profiles of our patient groups would differ. Third, based on previous studies, we predicted that the executive deficits of the ACoA group would adversely affect their performance on retrograde amnesia tasks, as these deficits would undermine strategic retrieval of previously stored information. In contrast, we expected that the retrograde amnesia of patients with damage to medial and lateral temporal cortices would be more extensive, reflecting the contribution of both retrieval and storage deficits.
Two amnesic patient groups and a nonamnesic control (NC) group were enrolled as participants (Table 1). One amnesic group included patients who had memory problems secondary to ACoA aneurysms. The other group included patients with varying etiologies of amnesia affecting temporal brain regions. They are referred to as having temporal amnesia (TA). There were no significant between-group differences with respect to age and verbal IQ estimates using the American National Adult Reading Test (AMNART; Grober & Sliwinski, 1991). TA patients, however, were significantly better educated than were the other groups (Table 1).
Demographic data and neuropsychological measures

Fourteen patients were referred from local rehabilitation facilities (Table 1). All had undergone surgery for repair of a ruptured anterior communicating artery aneurysm within 2 years prior to testing (M = 6 months). All patients had complaints of significant and disabling memory problems in their everyday lives but considerable variability was noted in terms of their memory performance. These patients were of average intelligence (VIQ = 102). Eight had shown evidence of confabulation in the acute post-operative phase.
Post-operative CT scan data were available for 10 of the 14 ACoA patients. Two neurologists, who were blind to experimental hypotheses, rated each scan along the following three dimensions: presence and extent of lesion in frontal brain regions, presence of striatal lesion, and presence of basal forebrain lesion. The extent of frontal damage was rank ordered on a scale of 1–6 with a score of 1 indicating no frontal damage. Data regarding lesion location and size in frontal, striatal, and basal forebrain areas are presented in Table 2.
Lesion data for ACoA patients

Twelve patients with amnesia based on neurological conditions presumed to affect medial temporal brain regions were included in the study. Etiology of amnesia in this group included herpes simplex encephalitis (3), anoxia (5), cerebrovascular accidents in posterior brain regions (2), and amnesia of unknown etiology (2). All TA patients, except those with amnesia of unknown etiology, demonstrated medial temporal damage on CT or MRI. Some of the patients had damage in areas beyond the medial temporal lobe but no TA patient had deficits in cognitive domains other than memory. The average Verbal IQ of the TA group was 108 and the mean duration of amnesia in this group was 6 years. The 2 patients with amnesia of unknown etiology went on to develop Alzheimer's disease years after their participation in the study. At the time of the study, both patients were fully intact on all cognitive tests save memory. One (M.R.) was densely amnesic (General Memory Index = 95; Delayed Memory Index = 54) in the context of superior intelligence (VIQ = 128), intact naming (BNT = 59/60; Kaplan et al., 1978), and superior performance on tests of executive abilities. The other (E.B.) had a similar profile with dense amnesia (General Memory Index = 85; Delayed Memory Index < 50), high average intelligence (VIQ = 122), intact naming (BNT = 58/60) and superior executive abilities. Based on the clinical presentations of these 2 patients and the ultimate course of their conditions, the involvement of medial temporal regions seems likely.
Seventeen nonamnesic control (NC) participants were recruited through advertisements in local newspapers. All NC participants underwent comprehensive screening procedures including memory testing. Exclusion criteria included any medical illness known to affect cognition. None of the NC participants had a history of alcoholism, dementia or psychiatric illness.
A select set of neuropsychological tests was administered to all participants by a neuropsychologist blinded to experimental hypotheses. Tests were chosen to provide information relevant to executive functions and new learning.
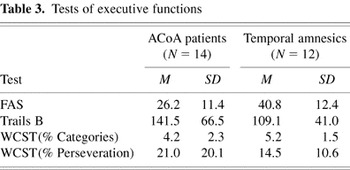
Executive functions were assessed with the Trail Making Test (TMT; Reitan, 1958) Controlled Word Association Test (FAS; Benton & Hamsher, 1989) and the Wisconsin Card Sorting Test (WCST; Heaton, 1981). These tasks were administered to patient groups only. ACoA patients performed worse than TA patients on all executive tasks but significant between group differences were noted only on the FAS task (Table 3).
Tests of executive functions
Anterograde amnesia was assessed with the Wechsler Memory Scale–Revised (WMS–R; Wechsler, 1987) and the Rey Auditory Verbal Learning Test (RVLT; Rey, 1964). The WMS–R was administered according to standard protocol and was administered only to patients (Table 1). The RVLT was administered to patient and NC participants. As per standard RVLT protocol, 15 words were read aloud five times. A measure of total recall was calculated for all five trials (range = 0–75). Delayed recall following a 20-min interval was calculated as was delayed recognition of the 15 words which were embedded in a list of 30 (15 target, 15 foil) words.
Results (Table 1) indicated severe learning and retention problems for both patient groups who performed significantly worse than NC participants on measures of RVLT total recall [F(2,33) = 15.35, p < .01], delayed recall [F(2,33) = 20.9, p < .01], and delayed recognition [F(2,33) = 10.3, p < .01]. There was a significant between-group difference with regard to the number of false positive errors [F(2,32) = 5.9, p > .001]. Nonamnesic control participants made an average of .45 (.69) false positives whereas ACoA patients produced an average of 2.8 (2.8) and TA patients produced an average of 3.6 (2.1) false positives. There was no difference between patient groups with regard to false positive errors. On the WMS–R there were no significant differences between patient groups with respect to performance on the General Memory (GM) Index [F(1,23) = 2.4, p > .10]; however, there were significant between-group differences on the Delayed Memory Index [F(1,23) = 10.9, p < .01] in that TA patients performed significantly worse than the ACoA patients.
The FFT and TNET both focused on memory for information in the public domain. Because TA patients varied in terms of time of onset of anterograde amnesia, events that followed the onset of amnesia (i.e., during the period of anterograde amnesia) were not included. Because all participants lacked exposure to remote news events that occurred prior to each individual's 15th birthday, these items were not included in the analyses.
Retrograde memory for famous people was evaluated with the FFT, a well-known measure of retrograde amnesia that has been used in many research studies. This test provides information regarding memory for photographs of individuals popular from the 1920's until the time of testing. The individual is asked to name the person in each photograph. In the event that they were unable to do so, lexical (first name) cues were provided to stimulate recall. Measures of free recall and cued recall were obtained.
A second test of memory for public information was the TNET. The original version of the TNET was used. This test included 40 questions focused on politics, crimes, and entertainment events that occurred in the news during the four decades that preceded testing. Transient items were selected according to objective criteria so that an item had to be in the New York Times an average of 60 times during a specific year and it had to fade from the news over the 3 following years. Across decades, items were matched for equivalent news frequency. Recall and recognition questions were asked. For example, a question from the year 1956 pertained to the tragic deaths of a group of Marines at Parris Island. If the participant did not come up with critical recall data regarding this event (i.e., the recruits drowned in the context of a punishment march), forced-choice alternatives were provided (were the recruits fired upon during an artillery exercise or did they drown during a forced march?). An event from 1975 involved the identity of Lynette Squeaky Fromme. In the event that the participant was unable to recall salient information regarding this person, he/she was given forced-choice alternatives (Lynette Squeaky Fromme either belonged to the Charles Manson family or she was the co-host of a television program with Soupy Sales).
Results were analyzed with one way analyses of variance (ANOVAs). Correlations were calculated in order to examine the relationships between retrograde amnesia, density of anterograde amnesia (estimated on the basis of the Delayed Memory Index from the WMS–R), and performance on tasks of executive abilities.
Consistent with our predication that TNET items would be more easily accessed than FFT items, nonamnesic participants showed significantly better performance on the FFT versus the TNET [t(15) = 6.4, p < .01]. This pattern of preferential recall of FFT items was seen in all three groups [t(41) = 7.6, p < .01].
Free and cued recall scores from the FFT were analyzed separately. As seen in Figure 1, NC participants recalled 77%, ACoA patients recalled 61%, and TA patients recalled 40% of FFT items. Analysis of variance revealed significant between group differences with respect to free recall [F(2,39) = 9.1, p < .01]. Post-hoc analyses revealed significant differences between NC and ACoA participants [t(29) = 2.1, p < .05]. Significant recall differences were also detected between the ACoA and TA participants [t(24) = 2.2, p < .05].

Recall and recognition of items from the Famous Faces Test.
Cued recall performance was 93% for NC, 89% for ACoA, and 76% for TA participants. In order to determine whether groups benefited differentially from cuing, difference scores (recognition minus free recall) were calculated. Between-group analyses revealed that all groups benefited from cuing [F(2,39) = 3.6, p < .05]. Contrary to our expectations, ACoA patients did not benefit more from cuing than did TA patients (p > .05).
Neither density (r = .29, p > .05) nor duration (r = .29, p > .05) of anterograde amnesia correlated with FFT recall for the ACoA group. Performance on FFT recall and performance on the FAS task were significantly correlated (r = .76, p < .01) whereas there were no significant correlations between FFT recall and other tests of executive functions. In the TA patient group there were no significant correlations between FFT recall and density or duration of anterograde amnesia (p > .05). TA patients did not demonstrate significant correlations between FFT performance on FAS or other tests of executive functions.
There were significant between group differences with regard to TNET recall [F(2,39) = 15.2, p < .01]. NC participants recalled 57%, ACoA patients recalled 42%, and TA patients recalled 15% of the TNET items (Figure 2). Post-hoc analyses revealed that the ACoA patients performed significantly worse than NC participants [t(29) = 2.1, p < .05] as did the TA group [t(28) = 5.8, p < .01]. ACoA patients performed significantly better than TA patients [t(24) = 3.4, p < .01].

Recall and recognition of items from the Transient News Events Test.
Analyses of TNET recognition revealed a significant group effect [F(2,39) = 9.2, p < .01]. On the recognition task ACoA patients (83%) did not differ from NC participants (89%) whereas TA patients (69%) performed significantly worse than NC participants [t(28) = 4.0, p < .01] and ACoA patients [t(24) = 2.6, p < .01]. In order to determine whether recognition probes disproportionately benefited any of the groups, a recall/recognition difference score was calculated. All groups benefited from recognition probes [F(2,38) = 7.8, p < .01]. Post-hoc analyses revealed that the ACoA group and NC participants did not differ with regard to the magnitude of response to recognition probes (p > .05). TA participants benefited significantly more from recognition probes in comparison with ACoA patients (p < .05) and NC participants (p < .01). Despite the advantage gained from recognition probes, TA patients still demonstrated significant deficits on TNET recognition.
Further analyses within the ACoA group focused on the relationships between density and duration of anterograde amnesia and TNET recall. A trend was noted between density of amnesia and TNET recall (r = .51, p = .06). However, duration of amnesia did not correlate with task performance (r = .23, p > .05). There was a significant correlation between TNET recall and performance on the FAS task (r = .70, p < .05). No other significant correlations were noted between TNET recall and behavioral measures of executive abilities.
Within the TA group, analyses did not reveal a significant correlation between density or duration of anterograde amnesia and task performance. Performance on TNET recall and the FAS task were not significantly correlated in this group (r = .24, p > .05), perhaps reflecting a floor effect as TA patients only recalled 15% of these items. No other significant correlations were noted between TNET recall and other tests of executive abilities in the TA group.
In light of previous work by Irle et al. (1992), we explored the possibility that combined basal forebrain and striatal lesions might be associated with increased memory loss. In our sample (Table 2), only 4 patients had imaging evidence of combined lesions in the basal forebrain and striatum. Consistent with previous findings, 3 of these patients (A.C., B.W., and W.Q.) performed poorly on tasks of anterograde amnesia. These patients also performed poorly on the TNET task. However, they did not all perform poorly on the FFT. In addition, a 4th patient (B.S.), who also had lesions in the basal forebrain and striatum, did not demonstrate evidence of severe anterograde or retrograde amnesia. Furthermore, other patients (A.T., G.S., and B.T.) demonstrated retrograde amnesia in the absence of combined basal forebrain and striatal damage. There was no significant correlation between the extent of frontal brain damage and FFT (r = .04, p > .05) or TNET recall (r = .13, p > .05).
The current findings confirm that patients who sustain rupture and who undergo surgical repair of anterior communicating artery aneurysms are at risk post-operatively for retrograde memory problems. These results are consistent with other studies that have demonstrated significant retrograde amnesia in ACoA patients. In comparison to nonamnesic control participants, ACoA patients demonstrated deficient recall of photographs of famous people and popular news events. However, the magnitude of the remote memory problems of ACoA patients was less than that seen in association with temporal amnesia.
Performance on two tests of memory for information in the public domain was examined. These tests differed with respect to frequency of exposure of their respective events and the nature of the retrieval cues. All groups, including nonamnesic control participants, were more adept in recalling FFT than TNET items. These findings indicate that recurrent exposure improves retention, a pattern noted in previous studies of long-term memory (e.g., Bahrick, 1984; Conway et al., 1992). The FFT and TNET both focus on recall of factual information and, to that extent, both tests involve semantic memory. However, because TNET items are from a circumscribed time period they also may involve episodic memory. It is likely that successful retrieval of TNET items depends on access to contextual cues. For instance, recall of the TNET item Fawn Hall (who was in the news frequently, but for a limited time period, in the late 1980's) would evoke specific contextual associations (i.e., the Contragate affair, Oliver North, Senate hearings, etc.) whereas recall of the FFT item Princess Diana would be contextually independent.
ACoA patients performed worse than NC but better than TA participants on FFT recall. With cuing, ACoA patients performed similarly to NC participants suggesting that their deficient memory was due to a retrieval problem rather than a knowledge deficit. Cuing was very beneficial for TA patients but, even with cuing, they demonstrated impoverished memory for FFT items in comparison to ACoA and NC participants. Consequently, their deficient knowledge of FFT items could not be simply seen as a consequence of deficient retrieval.
The second test of retrograde amnesia, the TNET, focused on knowledge of events that were in the news for a time-limited period. Both amnesic groups demonstrated significant impairments on tasks of free recall, with ACoA performing significantly better than TA patients. On the recognition test ACoA patients performed as well as NC participants but TA patients performed significantly worse than both groups. The failure of TA patients to respond to TNET recognition probes is further confirmation that their remote memory problems are qualitatively different from those seen in the ACoA group.
As in previous studies (e.g., Gade & Mortensen, 1990; Kopelman et al., 1999), cuing and recognition probes significantly enhanced the performance of memory impaired patients in our study. ACoA patients did not differ significantly from NC participants when cues were given but, even with cuing and recognition probes, the TA group performed significantly worse than ACoA and NC participants. This pattern of findings suggests that remote events were represented in memory for ACoA patients whose failure to recall items was due to retrieval difficulties. The finding that TA patients were unable to remember items, even when provided with cues and recognition probes, suggests that their problem was not solely due to a disruption of retrieval. It may well be that the TA patients could not access remote items due to the degradation of this information secondary to lesions in medial and lateral temporal cortices.
The contribution of executive dysfunction to various components of retrograde amnesia was examined in amnesic patients. Contrary to our prediction that executive deficits would underlie retrograde amnesia, performance on Trails–B and two indices of the WCST did not correlate with any measure of retrograde amnesia for either group. However, FAS performance correlated significantly with free recall of FFT and TNET items in the ACoA group. TA patients did not show significant correlations between FAS and recall of information from remote memory.
Our failure to detect a significant association between many aspects of executive abilities and retrograde memory may be due to the particular tasks used to assess executive dysfunction. The FAS, the Trail-Making Test, and the WCST are thought to be mediated by dorsolateral prefrontal cortices whereas the damage following rupture and surgical repair of ACoA aneurysms typically involves orbitofrontal brain regions. Had we chosen tests more sensitive to orbitofrontal damage, a different pattern of findings might have emerged. At the same time, it should be noted that other investigators demonstrated evidence of executive impairment in the ACoA patient population using a test battery similar to ours (D'Esposito et al., 1996).
The pattern of findings noted above can also be understood by examining the neuropsychological processes common to the selected tasks of executive functions and retrograde amnesia. The Trail-Making and WCST tests focus on components of cognition (e.g., mental flexibility, set maintenance, and problem solving) that may not be critical in terms of recall or recognition of remote events. In contrast, the processing demands of the FAS task and the tests of retrograde amnesia used in this study are quite similar. All three tests rely on the lexical retrieval of information previously stored in memory. It is, therefore, not surprising to note significant associations between performance on these tasks.
Subsequent analyses provided further support for the idea that the retrograde amnesia of the ACoA patient group was largely due to impaired lexical retrieval. Even though patient groups were matched according to naming on the BNT, performance on this test correlated only with retrograde memory in ACoA patients. TA patients did not show significant correlations between BNT scores and recall on the FFT (r = .28; p > .05) or TNET (r = .20; p > .05). In contrast, there was evidence of a significant correlation between the BNT performance of ACoA patients and recall of items from the FFT (r = .53; p < .05) and TNET (r = .78; p < .001).
Previous studies have shown that lesions in frontal regions, the basal forebrain, and the striatum contribute to the density of anterograde amnesia in the ACoA patient group (Damasio et al., 1985; Irle et al., 1992). Moreover, severity of amnesia has been associated with a specific pattern of lesion: combined lesions in basal forebrain and striatal regions have resulted in severe memory loss whereas isolated damage to either of these brain regions resulted in milder memory deficits. This finding was partially confirmed in the current study where 3 patients with damage in these brain regions demonstrated severe anterograde amnesia. However, there were exceptions to this pattern: at least 1 patient with damage in these brain regions did not have significant anterograde amnesia and 2 others without damage in those regions did have dense anterograde amnesia. Based on Irle's findings, we also speculated that combined lesions in the basal forebrain and striatum would predict density of retrograde amnesia. However, our findings were mixed with regard to this hypothesis. Several patients with basal forebrain and striatal damage had severe retrograde amnesia but others demonstrated dense memory loss in the absence of these lesions.
There are several differences between Irle's investigation and our study that are worth noting. Irle et al. (1992) examined a total of 57 ACoA patients, 30 with well-defined lesions and 27 who did not have evidence of lesions on imaging studies. Irle's conclusions regarding the critical substrates of anterograde amnesia were based on averaged data from patients grouped according to lesion site. We had access to imaging data for only 10 ACoA patients, several with no imaging evidence of lesions. Our small sample was further fractionated by heterogeneity of lesion site. The small sizes of our respective groups precluded statistical analysis of the relationship between damage to focal brain regions and retrograde amnesia. Close scrutiny of individual ACoA patients' performance in both studies revealed that basal forebrain/striatal lesions are not always seen in conjunction with anterograde or retrograde amnesia: as in our study, several of Irle's ACoA patients had severe memory difficulties even though there was no imaging evidence of brain lesions.
There have only been two similar group studies that have focused on the profile of retrograde amnesia in ACoA patients. Our findings are consistent with those of Gade and colleagues who showed that ACoA patients, assessed 2 years post onset, had retrograde amnesia. Our findings are also consistent with those of D'Esposito and colleagues who examined the performance of ACoA patients on the FFT at two consecutive points in time. Initial testing (1–2 months post onset) revealed evidence of impaired FFT recall for those patients with executive dysfunction. Repeat testing (2–4 months post onset) revealed improved FFT recall in conjunction with generally improved executive abilities. These findings supported the hypothesis that retrograde amnesia may result from a combination of memory impairments and executive deficits. Our patients also demonstrated impaired FFT recall in the presence of executive dysfunction. In our study, FAS was the only executive test that correlated with remote recall. This suggests that an inability to access stored information is the common underpinning in the remote memory problems and FAS deficits in ACoA patients.
Several limitations of this study may have affected the outcome. The first limitation pertains to selection biases. All of the patients in this study were referred to the Memory Disorders Research Center on the basis of memory difficulties in everyday life. Consequently, the present findings do not necessarily generalize to the larger population of individuals who have suffered rupture and surgical repair of an anterior communicating artery aneurysm. A second limitation concerns the fact that only a small number of patients participated in this investigation; it may well be that findings would differ in a larger cohort. This issue may have been particularly problematic with regard to the neuroanatomical analyses because data from only 10 patients were available. A third limitation concerned a possible ceiling effect regarding the performance of NC participants' on tasks of cued recall and recognition. A ceiling effect may have obscured a possible difference between ACoA and NC participants on these measures. Future studies should use more challenging tasks. Finally, it should be acknowledged that reliability and validity analyses of the FFT and TNET have not, to date, been undertaken. This shortcoming is particularly problematical in light of previous work indicating that even dense amnesics may demonstrate inconsistent recall on such tasks (Cermak & O'Connor, 1983).
Findings from the present study are consistent with previous studies indicating that ACoA patients have remote memory problems. In the present investigation ACoA patients performed worse than nonamnesic control participants on two tasks of retrograde amnesia. In addition, ACoA patients performed better than TA participants. Findings suggested that the poor performance of ACoA patients on tasks of remote memory was associated with impaired lexical retrieval, a problem that also affected performance on tasks of verbal fluency. Regardless of etiology of amnesia, all patients benefited from cuing and recognition probes. However, even with cuing, TA patients did not perform at the same level as ACoA or NC participants suggesting that their remote memory deficits could not be wholly attributed to a retrieval deficit.
Preparation of this paper was supported by Grants NS26985 and MH57681 awarded to Boston University. We thank Drs. Michael Alexander and Mark D'Esposito who reviewed and provided ratings for the imaging studies in this investigation and Marie Walbridge, Ph.D., who assessed many of the patients.

Demographic data and neuropsychological measures

Lesion data for ACoA patients

Tests of executive functions

Recall and recognition of items from the Famous Faces Test.

Recall and recognition of items from the Transient News Events Test.