Introduction
Obstructive sleep apnoea (OSA) is defined as a ‘disorder of breathing during sleep characterised by prolonged partial upper airway obstruction and/or intermittent complete obstruction that disrupts normal ventilation during normal sleep patterns’.1 OSA is one of the many chronic conditions in which partial or complete airway obstruction occurs, termed ‘sleep disordered breathing disorders’.2 A large proportion of children with OSA can be successfully treated by adenotonsillectomy. On clinical examination, it is important to note that large tonsils and adenoids do not necessarily indicate that the patient has OSA. Other significant factors are neuromuscular tone of the upper airway, obesity and craniofacial abnormalities. If left untreated, children may suffer significant neurocognitive consequences such as long-term learning difficulties, mood disorders and memory impairment, and carry lifetime cardiovascular risks such as systemic and pulmonary hypertension and growth failure.Reference Sinha and Guilleminault3, Reference Gozal4 In the UK, the roles of clinical history and examination (as well as investigation) have been well established for adults with OSA, but not for children. UK guidelines published by the Scottish Intercollegiate Guidelines Network and the National Institute for Health and Care Excellence include specific diagnostic criteria for adults with OSA, which are largely used in clinical practice today. These include a series of questions regarding general medical health, a detailed sleep history (e.g. the Epworth Sleepiness Score) and specific examination findings (e.g. retrognathia, hypertension, height, weight, oral examination, neck circumference).5, 6 Recognised signs and symptoms of paediatric OSA have been outlined by the American Academy of Pediatrics (Table I) but no UK guidelines currently exist.
Table I Signs and symptoms of obstructive sleep apnoea syndrome*

* According to the American Academy of Pediatrics1
It is widely accepted that children deemed at risk of post-operative cardiorespiratory complications should be managed in a specialist centre with provision of paediatric intensive care services. Children deemed unsuitable for surgery at a district general hospital were outlined in 2009 by a UK multidisciplinary working party (Table II).Reference Robb, Bew, Kubba, Murphy, Primhak, Rollin and Tremlett7 The working party recognised that a ‘normal child with severe OSA’ who is also at risk of post-operative cardiorespiratory complications is much more difficult to identify pre-operatively and that these children may be identified by overnight pulse oximetry.Reference Robb, Bew, Kubba, Murphy, Primhak, Rollin and Tremlett7
Table II Characteristics of children at risk for respiratory complications who are unsuitable for DGH adenotonsillectomy*

* According to the UK Multidisciplinary Working Party.Reference Robb, Bew, Kubba, Murphy, Primhak, Rollin and Tremlett7 DGH = district general hospital; ASA = American Society of Anaesthesiologists; ECG = electrocardiogram
Polysomnography objectively measures markers of sleep quality including brain activity, oxygen saturation, heart rate, breathing, and eye and limb movements; it is recognised as the ‘gold standard’ method of diagnosing paediatric OSA. The American Academy of Paediatrics recommends that polysomnography should be performed for all children with a clinical history of OSA.Reference Marcus, Brooks, Draper, Gozal, Halbower and Jones8 Unfortunately, this procedure is either not available or has a considerable waiting time in many hospitals across the UK. In addition, because of the long waiting lists for adenotonsillectomy, clinicians must also prioritise patients with severe OSA.Reference Nixon and Brouillette9 The severity of OSA in adults and children is measured using the apnoea–hypopnoea index. The definitions of obstructive apnoea and hypopnoea differ slightly in children compared with adults. Obstructive apnoea in children is defined as the total absence of airflow through the mouth and nose, with continued chest and abdominal effort for at least two respiratory cycles (duration of two missed baseline breaths). Hypopnoea is defined by the American Academy of Sleep Medicine as a reduction in nasal–oral airflow of at least 30 per cent, lasting for a period of two breaths and associated with decreased oxygen saturation of at least 3 per cent or cortical arousal or awakening. The classification of OSA severity in children is less widely accepted than that of adults. The suggested classification is based on the following polysomnography apnoea–hypopnoea index scores: less than 1, normal; 1–5, mild; 5–10, moderate; and more than 10, severe.Reference Flemons, Buysse, Redline, Pack, Strohl and Wheatley10, Reference Hauri and Sateia11 The lack of an accepted classification of paediatric OSA severity combined with a lack of clear guidance has resulted in variations in management.Reference Koo Ng and Kubba12
Where polysomnography is unavailable, other diagnostic sleep studies, such as pulse oximetry, have been used. Pulse oximetry demonstrates the patterns of cyclical oxygen desaturation by continuously monitoring oxygen saturation. In many centres, it is used as an alternative screening tool for OSA in children, despite there being no criteria by which to diagnose the condition or measure OSA severity. Brouillette et al. developed a scoring system akin to the apnoea–hypopnoea index in which a mixed–obstructive apnoea–hypopnoea index of at least 1 defined OSA.Reference Brouillette, Morielli, Leimanis, Waters, Luciano and Ducharme13 Out of 349 healthy children, 93 were diagnosed as having OSA according to these criteria: 90 of these tested positive for OSA by polysomnography. Thus, the procedure had a positive predictive value of 97 per cent. The McGill oximetry score, used in pre-operative pulse oximetry, was developed by Nixon et al.Reference Nixon, Kermack, Davis, Manoukian, Brown and Brouillette14 This system uses both oxygen desaturation frequency and the number of desaturation clusters as a means of prioritising surgery for children with OSA (Table III).Reference Nixon, Kermack, Davis, Manoukian, Brown and Brouillette14 The New Zealand Ministry of Health adapted these guidelines and combined them with those of the Paediatric Society of New Zealand for the use of post-operative pulse oximetry alone: a McGill oximetry score of at least 3 (corresponding to more than three desaturation events of less than 85 per cent) means that a child should be monitored for cardiorespiratory complications.15 Indeed, centres commonly perform adenotonsillectomy based on positive overnight pre-operative pulse oximetry findings and a strong history of OSA, although the definition of a positive result may vary widely from centre to centre.
Table III Mcgill scoring system for paediatric OSA*

* Adapted from Nixon et al. Reference Nixon, Kermack, Davis, Manoukian, Brown and Brouillette14
The inherent ambiguity of managing ‘healthy’ children with OSA is largely due to the sparse evidence available for diagnosis and the lack of clear guidance. For this reason, a UK multidisciplinary working party developed a consensus statement to assist clinicians in the decision-making process. Their main recommendation was to support the safe, local management of these patients, but to encourage the practice of referral to a tertiary centre when clinical suspicion alone suggested that these children may require post-operative paediatric intensive care facilities.Reference Robb, Bew, Kubba, Murphy, Primhak, Rollin and Tremlett7
The primary aim of this study was to examine the rationale behind pre- and post-operative pulse oximetry for diagnosing paediatric OSA. The method of ENT department referral, features identified on clinical examination, patients that underwent surgery, and quality of life (QoL) scores for patients who either did or did not undergo surgery to treat OSA were also investigated.
Materials and methods
A retrospective case note review was performed for patients who underwent pre-operative or immediate post-operative pulse oximetry between April and October 2013 at a large district general hospital in London. Pulse oximetry tests using the Masimo Radical-7® instrument were requested for 65 patients. Fifty-one patient notes were retrieved and an additional 14 patients were excluded because oxygen saturation had been monitored manually by nursing staff on the ward; therefore, results from 37 patients were available for analysis. Post-operative QoL scores were obtained retrospectively using the OSA-18 QoL questionnaire via telephone consultation.
Variables measured included age, sex, weight, height, referral method, main presenting complaint, features on clinical examination, high-risk co-morbidities and the number of positive pulse oximetry tests (defined as a McGill oximetry score of 2–4).
Results
Pre- or post-operative pulse oximetry was carried out on 65 children aged between 2 and 12 years: 38 boys and 27 girls. Fifty-seven patients (88 per cent) were referred to the ENT department by a general practitioner and eight (12 per cent) by a paediatrician. Over 96 per cent of patients presented with a history of either sleep apnoea or snoring. Five patients had a history of growth failure; all of these patients were referred by a paediatrician. Only 14 per cent of patients had their height recorded and 69 per cent had their weight recorded in their case notes: the weight range was 11–80 kg. Twenty-six of the 27 patients who presented with snoring had either grade 3–4 tonsils or evidence of obstructing adenoids on examination or lateral neck X-ray. Seven patients had significant co-morbidities including chronic lung disease, Down's syndrome, neurofibromatosis type 1 and sickle cell disease.
Of the 65 patients referred to the ENT department, pre-operative pulse oximetry was requested for 28 and post-operative pulse oximetry was requested for 37. Patient records revealed that three patients in the latter group did not undergo post-operative testing because it was deemed unnecessary by the clinician following surgery; however, all other patients had post-operative in-patient monitoring as planned prior to surgery. Thirty-seven test results (using the Masimo Radical-7® pulse oximeter) were available for analysis: for 21 patients in the pre-operative pulse oximetry group and 16 in the post-operative pulse oximetry group. Table IV shows that 15 out of 37 patients (41 per cent) had oxygen saturation of greater than 90 per cent (i.e. a negative pulse oximetry test, according to the McGill oximetry score) and 22 patients (59 per cent) had oxygen saturation of less than 90 per cent (i.e. a positive pulse oximetry tests according to the McGill oximetry score). Within the latter group, four patients had an oxygen saturation nadir of less than 80 per cent. In three of these patients, desaturation of less than 80 per cent occurred only once, which is consistent with moderate OSA according to the McGill oximetry score (Figure 1). Eight patients in the pre-operative pulse oximetry group who had negative pulse oximetry findings went on to have surgery. For only one child in this group, surgery was deemed unnecessary because of a negative pulse oximetry test.

Fig. 1 Bar graph showing the number of patients for each oxygen desaturation range. The box highlights the number of patients with an oxygen saturation nadir of less than 80 per cent. Pre-op = pre-operative; Post-op = post-operative.
Table IV Number of desaturation events and mean event duration in pre- and post-operative pulse oximetry groups

Pre-op = pre-operative; Post-op = post-operative; s = seconds
The only pulse oximetry test with a saturation nadir of less than 70 per cent was an unplanned test requested by the anaesthetist because the patient had developed loud stertor during recovery. This child did not deteriorate, require continuous positive airway pressure (CPAP) nor require transfer to a tertiary centre. Only one child underwent pre- and post-operative testing, where pre-operative testing was requested by the paediatric team prior to referral to the ENT department. Interestingly, in this case, the pre-operative McGill oximetry score was 3 (i.e. moderate OSA) and the post-operative McGill oximetry score was 2 (i.e. mild OSA).
Quality of life outcome scores were obtained for 32 patients who underwent pulse oximetry testing. Of these patients, 13 were from the pre-operative pulse oximetry group, and 14 were from the post-operative pulse oximetry group and 5 patients had manual pulse oximetry monitoring (including 2 pre- and 3 post-operative oxygen saturation monitoring). Twenty-five patients underwent surgery for OSA: 6 from the pre-operative pulse oximetry group, 14 from the post-operative pulse oximetry group and 5 from the manual pulse oximetry monitoring group. There was a significant difference between pre- and post-operative QoL outcome scores in the surgical group (p < 0.0001). In contrast, there was no significant difference in pre- and post-operative QoL outcome scores in the non-surgical group, where the mean follow up was 8.4 months after clinic review (p = 0.34; Tables V and VI).
Table V QoL Scores for patients who underwent surgery*
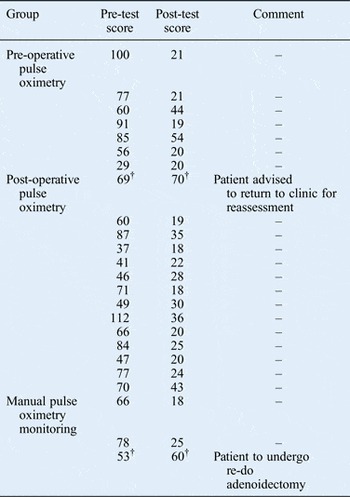
* Significant difference between pre- and post-test scores (p = 0.0001). †Patients with relatively high pre- and post-test scores
Table VI QoL Scores for patients who did not undergo surgery*

* No significant difference between pre- and post-test scores (p = 0.062). †Patients with relatively high pre- and post-test scores
Discussion
Findings
Of the 22 positive pulse oximetry tests, only one indicated severe OSA (i.e. had a McGill oximetry score of 4). Based on the working party consensus recommendation, this child should have been managed at a tertiary referral centre because they would have been deemed at a high risk of post-operative cardiorespiratory complications. Of the patients in the pre-operative pulse oximetry group, a few had co-morbidities that may have put them at a high risk of post-operative complications. In such cases, the need for referral to a tertiary centre relied very much on the clinician's judgement during patient assessment.
It is important to recognise that although four patients experienced an oxygen saturation nadir of less than 80 per cent, for three patients an oxygen desaturation event occurred only once. According to the Working Party Consensus Statement, these children would be diagnosed with severe OSA, as opposed to moderate OSA according to McGill oximetry score. The difference between these two classification systems therefore determines how and where these patients are managed.
Post-operative pulse oximetry testing of ‘healthy’ children at a district general hospital remains controversial. Our results show that this did not influence management, even when the result was positive. In children considered at a high risk of post-operative complications, there is definitely a role for post-operative observation and monitoring, though formal pulse oximetry testing may not be necessary. Of the seven children with significant co-morbidities, none were excluded from having surgery at a district general hospital and only four underwent pre- and/or post-surgical pulse oximetry, which is inconsistent with current guidance.
Reliability of pulse oximetry
In the literature, the reliability of pulse oximetry has been questioned because it can miss apnoeic episodes that are not associated with oxygen desaturation.Reference Ryan, Hilton and Boldy16 In addition, it cannot confidently exclude the diagnosis in milder cases.Reference McNicholas17 Furthermore, although some studies suggest a high positive predictive value for pulse oximetry, a negative predictive value of 57 per cent has also been reported, as well as a sensitivity of 31–98 per cent and specificity of 41–100 per cent.Reference Koo Ng and Kubba12, Reference Caulfield and Gleeson18 The American Thoracic Society recognises that most evidence on pulse oximetry is level 3 (case control, cohort, observational studies), and that high levels of false positive rates can over- or underestimate OSA severity, with implications for management.
Physiology
Cardiorespiratory complications occur because hypopnoea and apnoea cause hypoxia and hypercarbia. Hypoxia leads to a rise in sympathetic output, causing vasoconstriction, tachycardia and raised blood pressure. In turn, this leads to subcortical arousals, which terminate the obstructive airway event. Long standing OSA leads to irreversible pulmonary hypertension and consequently right sided heart failure and cor pulmonale.Reference Guilleminault and Cummiskey19 It is thought that OSA can persist in the early post-operative period because of a combination of upper airway swelling, central respiratory depression, particularly from opioids and time taken for re-calibration of the central hypercapnic respiratory drive.Reference Guilleminault and Cummiskey19 One study involving 133 children with OSA has shown that adenotonsillectomy significantly increases baroreflex sensitivity after six weeks and six months, thereby lowering blood pressure and preventing the development of cardiorespiratory complications. However, it does not comment on the immediate post-operative period, which is what is observed in post-operative pulse oximetry.Reference Crisalli, McConnell, VanDyke, Fenchel, Somers, Shamszumann, Chini, Daniels and Amin20 Ideally, a child at a high risk of post-operative cardiorespiratory complications (where post-operative monitoring is warranted) may require CPAP; there must therefore be adequate paediatric intensive care facilities to support this. In many district general hospitals, including ours, this is unavailable, raising the question of the appropriateness of performing this test in settings where there is no available CPAP or non-invasive positive pressure ventilation.
Patient follow up
Interestingly, the UK Multidisciplinary Working Party only mentions the use of pre-operative pulse oximetry as a screening tool for patients at a high risk of post-operative complications, and does not mention the role of post-operative monitoring.Reference Robb, Bew, Kubba, Murphy, Primhak, Rollin and Tremlett7
Patients who underwent surgery were not followed up in this study, but post-operative polysomnography suggests that patients may continue to have OSA despite surgery.Reference Caulfield and Gleeson18 The reasons for persistent OSA include anatomical and neuromuscular factors which affect the size and shape of the pharyngeal airway.Reference Rosen, Muckle, Mahowald, Goding and Ullevia21 The American Thoracic Society recommends that all children with OSA should be reassessed at six to eight weeks post-operatively.1 It is recommended that patients that continue to have symptoms should be placed in the high risk group and undergo a post-intervention sleep study.Reference Caufield22 Whether or not this is applicable in a district general hospital setting, where a confirmed diagnosis is not certain, is perhaps best left to the individual clinician. Quality of life scores remained high in 7 out of 32 of the patients (22 per cent), which may reflect persistent OSA in some. Two of these patients are still awaiting surgery and three have been re-referred to the ENT department, where revision surgery to the adenoid tissue has been scheduled for two of them.
Limitations of the study
Out of 65 patients, only 37 results (57 per cent) were usable for analysis, which reduces the power of the study. Quality of life scores were obtained retrospectively via telephone, which is another limitation. Different groups of children (i.e. unmatched) that had pulse oximetry testing and did or did not have surgery were compared in our results, thus introducing bias.
Financial considerations
At our hospital, pulse oximetry testing using a Masimo Radical-7 device costs approximately £150. The cost of an overnight stay on a paediatric ward is £500. It is important to mention, however, that in many parts of the UK, the oximetry is carried out cost-effectively as a domiciliary procedure managed by community paediatric nursing staff. In contrast, a standard polysomnography study costs approximately £820 and the hospital stay may be more costly, depending on whether patients require non-invasive positive pressure ventilation. Given that none of the patients in the post-operative pulse oximetry group warranted transfer to a tertiary centre (because of the lack of CPAP and/or non-invasive positive pressure ventilation availability), one may question the utilisation of these tests and their large cost implications to the Trust. Surely a more expensive test such as polysomnography with appropriate on-site facilities would be of more value to patients and Hospital Trusts. Given the expense and poor availability of polysomnography, some studies have investigated the use of symptom questionnaires as a cheaper, more accessible alternative to polysomnography. However, some such as the OSA-18 QoL questionnaire, with a sensitivity of 40 per cent, do not accurately diagnose or detect OSA.Reference Caufield22, Reference Constatin, Tewfik and Brouillette23
We examined the opinions of five consultant otolaryngologists at our hospital regarding use of pulse oximetry; all agreed that children at a high risk of post-operative cardiorespiratory complications require formal polysomnography testing. Some consultants also felt that post-operative pulse oximetry monitoring was a reasonable investigation for children suspected of being at a high risk of post-operative cardiorespiratory complications; however, others disagreed and thought that any suspicion warranted pre-operative testing and re-review in clinic prior to considering surgery at a district general hospital. This variation in opinion and practice is reflected in our results, and is more widely applicable across the UK. Interestingly, one study in Leeds examined the regional surgical referral patterns of 15 consultants to paediatric intensive care facilities, and found no consensus on patient referral, despite the guidance available for referring children at a high risk of post-operative cardiorespiratory complications.Reference Blenke, Anderson, Raja, Bew and Knight24 Another study surveyed 298 UK consultants before and after the UK Multidisciplinary Consensus Statement came out. It found that less than 2 per cent of clinicians used polysomnography and 70 per cent would proceed with surgery without any form of sleep study. There was no difference between responses before and after publication of the Consensus Statement.Reference Pringle, Natesh and Buchanan25 One study comparing the similar practice of 183 otolaryngologists in North America found that objective testing for OSA before surgery was less than 10 per cent.Reference Weatherly, Mai, Ruzicka and Chervin26
• Pulse oximetry can guide the triage of patients who require specialist paediatric services
• It is not a diagnostic tool for obstructive sleep apnoea
• It may help in deciding the surgical intervention for obstructive sleep apnoea
• Post-operative pulse oximetry is unlikely to affect patient management
Irrespective of which practice is conducted at centres across the UK, it is important that a logical and safe approach is used. We propose a pragmatic approach to a child with suspected OSA which satisfies the Working Party Consensus Statement. This includes taking a thorough medical history and performing an examination as described by the American Academy of Pediatrics. Children can then be allocated to two groups: ‘normal’ children with OSA and those at a high risk of post-operative cardiorespiratory complications. If a child falls into the high-risk group, we advise referral to a tertiary centre or management at a centre with a paediatric high-dependency unit and/or paediatric intensive care unit facilities available (Figure 2).

Fig. 2 Flowchart illustrating the Local Trust policy. HDU = high-dependency unit; PICU = paediatric intensive care unit; PNS = posterior nasal spine; OSA = obstructive sleep apnoea; post-op = post-operative.
Conclusion
Our study shows the use of both pre- and post-operative pulse oximetry and demonstrates variability in clinical practice amongst otolaryngologists. Without the availability of paediatric high-dependency unit and/or paediatric intensive care unit facilities, patients at a high risk of post-operative cardiorespiratory complications or those with severe OSA cannot be fully supported at a district general hospital. It is vital that Working Party Consensus Guidelines are recognised in clinical practice to ensure the safe management of children with OSA. More research is required to develop reliable diagnostic studies for paediatric OSA in ‘healthy’ children to avoid unanticipated cardiovascular complications in this group. Many children are now managed as day cases and pulse oximetry adds helpful pre-operative information on those of borderline age and weight on their suitability for non-specialist day case admission for surgery. The National Service Framework states: ‘Quality and safety of care is assured by having systems in place across health services and local authorities to deliver continuously improving high quality child-centred services’.27 In order to achieve this, hospitals must be guided by evidence based policies that will assure best clinical practice and better QoL outcomes for patients.










