In recent years, telemedicine has become the focus of increasing attention in clinical practice research. Understood as the use of information and communication technologies (ICTs) to enable the transfer of medical information for diagnostic, therapeutic and educational purposes, it has created rising expectations for healthcare services. These include better management and increased quality, effectiveness and efficiency of clinical practice (1). However, available evidence suggests that telemedicine use is relatively limited (2). There is general consensus that its slow, arduous implementation can be attributed to the lack of definitive scientific evidence supporting its positive impact on clinical practice (improved quality and effectiveness) and economic outcomes (improved cost-benefit) (3).
While most studies have focused on analyzing the results of telemedicine use (effectiveness, improved healthcare services and quality, etc.) (1), it is crucial to consider the determinants of its use to fully understand the issue. In other words, it is necessary to perform an ex-ante analysis of the determinants of telemedicine use, rather than an ex-post analysis of the determinants of the outcomes of telemedicine use. This article, therefore, presents an ex-ante analysis and aims to provide evidence on the determinants of telemedicine use.
To understand the drivers of e-health adoption, a range of methodological and disciplinary approaches have been used. Technology-oriented research has noted that Roger's diffusion of innovations theory and Davis's technology acceptance model (TAM) have been successfully used to understand the factors that explain ICT use by healthcare professionals (4). Information systems and social-oriented research has highlighted that clinical practice may be intimately interconnected to a range of digital devices and forms of information (5), and to the ways that users use them in their private lives. Organization-oriented research has shown that the structure of healthcare organizations, tasks, people policies, incentives and decision-making processes play a major role in explaining how medical professionals overcome barriers to ICT use (6). Ethical and legal-oriented research has suggested that changes in the nature of the doctor–patient relationship, the status of health informatics and the role of hardware/software providers tend to have an effect on ICT use by medical professionals (7). Finally, usability-oriented research has shown that compatibility between clinical ICT systems and physicians’ tasks, ICT support for information exchange, communication and collaboration in clinical practice, and interoperability and reliability also explain the success of ICT use in healthcare (8).
Taking the above into account, this study analyses the determinants of the intentions of the medical staff at a healthcare institution to use telemedicine. The institution is a network of primary care centers and a reference hospital in the north of Barcelona. It provides private medical cover for a population of almost 100,000 people. As the unit of analysis, we took the healthcare institution and its experiences in developing different telemedicine-related projects to look after patients with chronic diseases, from primary care. By doing so, the intention was to attain a twofold objective. First, to characterize and develop a typology of medical professionals according to their ICT use and expectations, and to identify the factors that foster or hinder telemedicine use in the healthcare organization where they practice. And, second, to determine the factors that have a greater capacity to explain the intention to use telemedicine.
HYPOTHESES AND MODEL
TAM is the theoretical proposal most widely applied to research into the acceptance of new information technologies in the professional sphere (9–11). In particular, the model has the capacity to robustly explain variance in the intention to use ICTs and ICT use behavior, taking into account the individual's perceptions of technology. Specifically, these are (i) perceived usefulness and (ii) perceived ease-of-use (11). However, some studies conducted in the field of healthcare have shown that ICT use has a twofold usefulness. First, it improves the quality of clinical practice (12), and second, it reduces the economic, time and human costs associated with clinical practice (13). Thus, we propose the first hypothesis and sub-hypotheses of the study (see H1.1, and H1.2 in Table 3).
Regarding the second variable, TAM shows how the perceived ease-of-use of ICTs has a twofold effect on the individual. First, a greater intention to use technology; and second, greater perceived usefulness of it. In this respect, Davis et al. (9) argued that improved ease-of-use could be instrumental in contributing to an increase in medical professionals’ efficiency. In this respect, the second hypothesis (H2) is as shown in Table 3.
Despite its widespread acceptance, this model has a series of limitations that mainly stem from the fact that it does not take the influence of other types of variables into account. Bagozzi (14) underscored the need to increase the explanatory power of this model by incorporating additional variables. According to Davis, identifying variables like these in TAM can increase the explanatory power of the system users’ acceptance (10). This is particularly important to the development of TAMs in the field of healthcare, where the consideration of variables relating to information security and protection, for example, constitutes one of the main incentives for or barriers to technology acceptance. In this respect, the third hypothesis (H3) is as shown in Table 3.
In addition to the determinants identified above, we should stress the importance of the geographical, legal, social, cultural, and economic contexts of the territory (15) to the acceptance of telemedicine. Together, they have the potential to determine people's predisposition toward using new technologies. By taking into account the contributions made by models tending to stress the importance of the user profile and of social influence (subjective norm), such as the theory of reasoned action (TRA) and the theory of planned behavior (TPB), we were able to expand our model to include the influence of the professional environment or subjective norm (16): the patients, the medical staff and the healthcare center's board of directors. With regard to the incentives offered by the healthcare center's board of directors, it should be noted that, in addition to the effect that they have on the medical staff's intention to use telemedicine, they generate a moderating effect on the medical staff and the healthcare center. In this respect, the fourth hypothesis and sub-hypotheses (H4.1, H4.2, H4.3, and H4.4) are as shown in Table 3.
Some empirical studies have also noted the moderating effect that the subjective norm has on the user's perceived usefulness of ICT use (17). While there is no consensus on the moderating effect that the subjective norm has on perceived usefulness, we assumed that this effect on clinical practice was positive. Robinson's studies (18) showed how the opinions of the patients, the medical staff and the healthcare center's board of directors had a positive influence on the physician's perceived benefits of ICT use. In this respect, the fifth hypothesis and sub-hypotheses (H5.1, H5.2, H5.3, H5.4, H5.5, and H5.6) are as shown in Table 3.
Finally, it should be noted that physicians use ICTs in their professional and personal lives. As ICT users, physicians may use technology with differing degrees of intensity and frequency. When it comes to defining the profile of an ICT user, cultural and social aspects clearly have a role to play (1), as do other circumstantial variables such as experience and training (18). The development of mixed-approach models comprising elements that refer to both the user profile and to technology, such as Parasuraman and Grewal's theory of technology readiness (TR) (19), allowed us to consider the need to incorporate elements that refer to the user profile and the user's relationship with ICTs. In this respect, the sixth hypothesis (H6) is as shown in Table 3. The proposed model is shown in Figure 1.
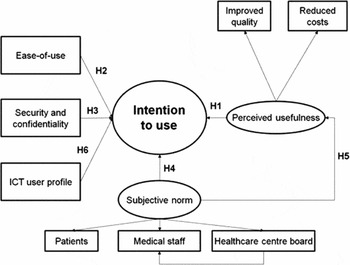
Figure 1. Model, hypotheses tested and outer weights diagram (mean). Model and Hypotheses, where we considered that the medical staff's intention to use telemedicine depended on three major groups of variables: (a) the physician's perception of telemedicine; (b) the subjective norm; (c) the physician's relationship with ICTs as a user in his or her personal life.
MATERIALS AND METHODS
One of the main contributions of this study is the proposal of an integrative model of the determinants of telemedicine use by medical staff. As indicated in the previous section, this model is the result of a review of classic theories. Thus, a review of TAM, TRA, and TPB led us to propose, in the form of hypotheses, that a physician's decision to adopt a technology would be determined by several factors: (i) the perceived usefulness of telemedicine (Hypothesis 1); (ii) ease-of-use of ICTs in clinical practice (Hypothesis 2); (iii) the perception of information security and confidentiality offered by telemedicine use in clinical practice (Hypothesis 3).
These first three hypotheses were formulated based on contributions from TAM.
Hypotheses 4 and 5 were formulated based on contributions from TRA and TPB, which highlight the direct and moderating effects that the social context exerts on decisions taken by the physician: (iv) specifically, patients, the medical staff, the healthcare center, and public authorities have a direct influence on the physician's decision to adopt a technology (Hypothesis 4); (v) in addition, the above-mentioned groups were considered to exert a moderating effect on the decision taken by the physician. This effect is determined by the influence that patients, the medical staff, the healthcare center, and public authorities have on the physician's perceived usefulness of telemedicine (Hypothesis 5).
Finally, and taking into account that the physician's personal context has an influence on his or her clinical practice, Hypothesis 6 was formulated. It proposes that the ICT user profile of the physician, in his or her personal life, has an influence on professional ICT use. Based on a sample comprising ninety-six physicians, section 3 of this study proposes the acceptance or rejection of the formulated hypotheses.
Study Design and Sample Selection
The research presented in this article is the result of a collaboration between the healthcare institution in question and the Open University of Catalonia (UOC), Spain. As an exploratory study focusing on the analysis of a single healthcare institution, a mixed qualitative and quantitative methodology was used, and a questionnaire (Supplementary Questionnaire) was designed to serve as the data collection instrument.
A review of the literature together with the healthcare professionals’ experience served as the basis to create the study variables and the metrics used in the first version of the instrument. The measurement instrument was validated following a pretest. The final questionnaire was organized into five blocks of questions: (i) sociodemographic and professional background; (ii) degree of ICT and Internet use in general; (iii) degree of IT-system, ICT and Internet use at work; (iv) opinions about ICT and Internet use in the field of health care; and (v) opinions about telemedicine use in clinical practice. The questionnaire had seven theoretical sections and thirty-six variables. The survey was anonymous and optional.
The survey targeted a total population of 398 medical professionals from a healthcare institution. This institution manages nine primary care centers in the metropolitan area of Barcelona, Spain, and has a University Hospital as its reference. These centers serve 240,000 inhabitants.
To test the hypotheses proposed in the model, it was necessary to measure each of the above-mentioned constructs using different variables (see Table 1). In the Supplementary Statistical Appendix of the paper, the study variables and measurement scale construction are presented.
Table 1. Study Variables

RESULTS
Medical Professional's Profile
At 24 percent, the response rate was much higher than the mean for online questionnaires (20). The study included the answers given by a randomly obtained sample of ninety-six professionals, who had agreed to take part and worked for the healthcare institution in question between April and June 2012. Given that it was a finite sample, the margin of error was 8.7 percent at a confidence level of 95 percent.
The sample of professionals analyzed was representative of the population analyzed, and, consequently, the results obtained from the study on it can be extrapolated to the entire institution. The sample was obtained using a random sampling procedure, and it represented 24 percent of the total of 398 physicians making up the workforce. Likewise, their characteristics faithfully reflected the profile of the medical population, comprised of 76 percent women and 24 percent men. The mean age is around 40 years and the mean period in post is 13 years. Seventy percent hold permanent contracts.
Regarding the study sample, it consisted mainly of women (73.1 percent) with a mean age that did not exceed 40 years. Specializing in primary care (87.5 percent were family doctors), they practiced in a healthcare center (90 percent) and had been in post for a mean of 13 years.
As a professional group, it perceived that telemedicine use offered significant benefits. Indeed, more than 50 percent of the respondents considered that using telemedicine would improve the quality of clinical practice and would reduce the costs associated with it. Likewise, they pointed out that the ICT applications in the field of healthcare would be secure and not too difficult to use. The modal values were high in both cases.
However, they could not be characterized as professionals that used ICTs intensively in their clinical practice. In fact, most of them said that they were not particularly innovative, and that their use of ICTs in their personal lives was not very intensive. Thus, with regard to the ICT user profile, the youngest professionals, under 40 years of age, were found to be intermediate or advanced users of technology. A correlation between the two variables was found (Chi-square: 98.026, sig. 0.004).
Finally, it should be noted that the medical profession is heavily influenced by the pressures of its environment. In total, 75 percent of the professionals acknowledged that the influence exerted by the patients and the medical staff was high. Likewise, the influence exerted by the healthcare center's board of directors was also high among the youngest professionals.
Intention to Use Telemedicine
To test the hypotheses proposed in the study and, therefore, to establish the direct and moderating effects that the above-mentioned variables have on the physicians’ intention to use telemedicine, a logistic regression analysis was performed. Logistic regression is a type of probabilistic statistical classification model. This technique is similar to multiple regression analysis, in that one or more independent variables are used to predict a single dependent variable. According to Hair et al. (21), it shows the relationship between a dependent and one or more independent variables, and allows the fit of the model and the significance of the relationships (between dependent and independent variables) to be examined.
The model's goodness-of-fit was confirmed by the values and levels of significance reached by the Chi-square statistic (30.786, 0.013) and the Hosmer-Lemeshow test (17.75, df:8, 0.046). Likewise, the value of Nagelkerke's statistic indicated that the model obtained explained 48.1 percent of the dependent variable's variance.
Table 2 shows the estimated parameters for each independent variable, as well as their level of significance within the model. The variable with the highest explanatory power within the model was perceived usefulness for reducing costs. In descending order of importance, the medical staff's interest in using telemedicine was second and the security and confidentiality offered by telemedicine was third. All of the variables showed a significant direct effect on the physician's intention to use telemedicine.
Table 2. Relationships between the Explanatory Variables and Telemedicine Use

The results obtained show that patients and the healthcare center did not exert a direct effect on the physician's decision. However, these groups showed a moderating effect on the physician's decision, as the physician perceived that, for patients, the physicians themselves and the healthcare center, telemedicine would have a positive influence on improved quality and reduced costs associated with clinical practice.
Finally, it should be noted that the ICT user profile of the physician did not have an influence on the intention to use telemedicine. This may have been because the technology used by the physician in his or her clinical practice was not excessively complex. Thus, whatever ICT user profile the physician might have had in his her private life, it did not influence the intention to use telemedicine.
The results obtained allowed us to accept hypotheses H1.2, H3, H4.1, H4.2, H5.1, H5.2, H5.3, H5.4, and H5.6, and reject hypotheses H1.1, H4.3, H4.4, H5.5, and H6 with regard to the direct and moderating effects exerted by these variables. To sum up, Table 3 shows the final results for the hypotheses proposed in the study. This table shows whether the variables were accepted or rejected, depending on the level of significance reached.
Table 3. Hypotheses and Results

DISCUSSION
The aim of this study was to explain the factors that determine the adoption of telemedicine in clinical practice by the healthcare institution's medical staff. To that end, a theoretical model based on a modified TAM was used as the analysis tool.
Our study revealed four main results. First, it confirmed that a) perceived usefulness for reducing costs associated with clinical practice (β = 1.324; p = 0.020) and b) the medical staff's interest in using telemedicine (β = 1.005; p = .091) were the explanatory factors that had the biggest impact on the probability of using telemedicine. As the TAM suggests, the statistical significance of these two determining factors refers back to the importance of perceived usefulness when the use of a technology needs to be explained. Specifically, the physicians at the healthcare institution placed importance on telemedicine's potential to reduce costs, and on its usefulness to the medical profession. The need to optimize costs in a context of economic crisis, healthcare cost containment, and health service cutbacks (22), and the fact that this healthcare institution is a nonprofit private foundation may explain the significance of reducing costs associated with clinical practice. At the same time, the result relating to the medical staff's interest in telemedicine could also be attributed to network effects, which are crucial to the adoption of any technology (23).
Theories such as TAM, TPB, and TRA highlighted the importance of the above-mentioned variables. Thus, TAM showed that perceived usefulness or information security and confidentiality had an important influence on the decision to adopt technology in clinical practice. This is especially important when professional activity is connected with the provision of a healthcare service, given the confidential and sensitive nature of the information processed, as well as the high costs associated with the service provision.
Moreover, TPB and TRA showed that social context, also called the subjective norm, was a factor that had an influence on the decision to adopt technology. Within the context in question, work colleagues exerted a high level of influence on the physician when it came to adopting technology or not.
It was odd to find that some variables highlighted in the aforementioned theories did not exert a significant direct influence on the physician's decision to adopt telemedicine. Specifically, variables such as perceived usefulness for improving quality or the influence that patients and the healthcare center itself had on telemedicine use did not reach the necessary levels of significance. Regarding perceived usefulness for improving quality, the lack of significance may have been because the healthcare center already offered high levels of quality. Thus, physicians intended to use telemedicine to increase the efficiency of healthcare processes while maintaining the existing quality standards and reducing associated costs in the process.
However, neither telemedicine's perceived usefulness for improving the quality of clinical practice, nor the perceived ease-of-use of ICTs in clinical practice were found to be significant. In this respect, telemedicine was perceived as a technology that serves to reduce costs rather than increase quality. Three characteristics of the sample and research model may explain why perceived usefulness in terms of quality was not significant. First, health systems are currently burdened by an increasingly ageing population and also by an increasing prevalence of long-term conditions. These factors, coupled with an increase in healthcare expectations in a political context of reduced healthcare spending, all combine to place a significant increase in demand for care and increasing pressure on available healthcare resources (24). Second, given that the physicians in the study sample had a mean age of under 40 and had been in their posts for a mean period of 13 years, they had experience in the use of ICTs. Therefore, they were experts in relation to the potential use of ICTs, that is, the positive impact of telemedicine on service quality. Third, as stated in the empirical literature (25), promoting the use of telemedicine should go beyond the purely technological dimension. Instead, the professional and social determinants, as well as those of a contextual and organizational nature, should also be considered.
In the explanation of the physicians’ intention to use telemedicine at the healthcare institution, second in order of importance were the perception of medical information security and confidentiality (β = 0.768; p = .017), and the patients’ predisposition toward telemedicine (β = 0.583; p = .084). While there is empirical evidence of the significance of medical information security and confidentiality, much of the research has concluded that the lack of a privacy and confidentiality policy represents a considerable barrier to telemedicine use. In the explanation of the intention to use telemedicine, the positive effect of the patients’ influence could be attributed to the specific nature of the healthcare institution.
In the explanation of the physicians’ intention to use telemedicine at the healthcare institution, a third group of results demonstrated the statistical significance of a set of moderating factors. Albeit with lower coefficients/probabilities than those noted previously, the intention to use telemedicine can be explained by the fact that: (i) the patients’ positive assessment of telemedicine use by the physicians exerts a moderating effect on the physicians’ perceived usefulness of telemedicine for improving their clinical practice (β = 0.347; p = .084) and (ii) for reducing the costs associated with their clinical practice (β = 0.462; p = .004); (iii) the medical staff's positive assessment of telemedicine use exerts a moderating effect on the physicians’ perceived usefulness of telemedicine for improving their clinical practice (β = 0.366; p = .046) and (iv) for reducing the costs associated with their clinical practice (β = 0.488; p = .044); and (v) the healthcare institution's positive assessment of telemedicine use exerts a moderating effect on the physicians’ perceived usefulness of telemedicine for reducing the costs associated with their clinical practice (β = 0.571; p = .022). In the explanation of the intention to use telemedicine, this set of moderating effects would appear to corroborate the importance of the physicians’ own opinions. The physicians would moderate their perceptions of usefulness when the patients’ and the institution's opinions of telemedicine use were favorable.
Finally, in the explanation of the intention to use telemedicine, the intensity of the physicians’ ICT use in their personal lives was not significant. Despite being a professional group that did not use ICTs intensively, it perceived that ICT applications in the field of healthcare were secure, not too difficult to use, and also offered significant benefits in terms of reducing costs, all of which prevailed in the physicians’ intention to use telemedicine.
These results have revealed the need for a dynamic approach to the design of telemedicine use, especially when it targets a variety of end-users. Hence, the importance of conducting studies before using telemedicine, and attempting to identify which of the above-mentioned predictors exert an influence and how. Research is confronted with the challenge of producing such evidence, a prerequisite for the generalized adoption of telemedicine. In this respect, it is reasonable to assume that the variations in barriers to technology adoption have more to do with local factors than technology infrastructure development. This scenario poses a considerable challenge for the formulation of public policies and strategies by healthcare institutions, where decisions on telemedicine use should not be overlooked. Policies that promote the use of telemedicine should, therefore, go beyond the purely technological dimensions and take into account other factors such as professional and social determinants, as well as those of a contextual and organizational nature. Its potential to improve the healthcare sector's efficiency when, in addition, it is accompanied by a suitable information confidentiality and privacy policy could, therefore, be considered a twofold positive aspect of incorporating telemedicine use into healthcare.
Beyond these preliminary results, the authors believe that future research should include (a) a comparison of the results with other samples of physicians who use telemedicine, particularly a comparative study of the public and private sectors, and (b) an extension of the ex-ante model to an ex-post model to analyze how the determinants of telemedicine use affect the outcomes of clinical practice.
SUPPLEMENTARY MATERIAL
Supplementary Questionnaire
Supplementary Statistical Appendix
Supplementary Tables 1–4 http://dx.doi.org/10.1017/S0266462316000015
CONFLICTS OF INTEREST
The authors declare no competing interests.






