Introduction
Oropharyngeal dysphagia is a common symptom that can cause mild discomfort to life-threatening aspiration events. Swallowing dysfunction has devastating health implications, putting patients at high risk for aspiration of secretions, liquids or food particulates, subsequent development of aspiration pneumonia, and potential death.Reference McClave, DeMeo, DeLegge, DiSario, Heyland and Maloney1
The estimated prevalence of dysphagia ranges from 3 to 4 per cent in otherwise healthy adults in Western countries with increased rates among high-risk populations.Reference Chadwick and Jolliffe2–Reference Bhattacharyya4 Martino et al. reported that following a stroke up to 78 per cent of patients had abnormal swallowing with increased risk for pneumonia among patients with evidence of aspiration.Reference Martino, Foley, Bhogal, Diamant, Speechley and Teasell5 Hospital and societal costs for patients affected by dysphagia are increasingly recognised as a major expense that will continue to increase with an aging population. In the USA, hospital stays among dysphagic patients were 1.64 times longer and almost double the cost of patients without dysphagia, with an estimated cost per year reaching approximately $547 million.Reference Cichero and Altman6
Aspiration pneumonia is an infectious process caused by the inhalation of organic debris or oropharyngeal secretions colonised by pathogenic bacteria, with the risk of occurrence among patients with dysphagia increased through a variety of mechanisms. Dehydration reduces salivary flow and leads to higher rates of pathogen colonisation in the oropharynx.Reference Via and Mechanick7 This places dysphagia patients at higher pneumonia riskReference Sellars, Bowie, Bagg, Sweeney, Miller and Tilston8,Reference Furman9 and is further exacerbated by a susceptibility to opportunistic infection secondary to increased rates of malnutrition and weight loss. As such, patients with dysphagia tend to have an increased overall risk of disability and death.Reference Altman, Yu and Schaefer10 The mental health and social impact of dysphagia is also significant with strong associations including compromised quality of life, mental well-being and social functioning, and increased risk of anxiety and depression.Reference Plowman-Prine, Sapienza, Okun, Pollock, Jacobson and Wu11
The videofluoroscopic swallow study permits examination of swallow efficiency and risk of aspiration by relating bolus flow to structural movement throughout the upper digestive tract in real time. Radiological evaluation of swallowing allows examination of swallowing dysfunction using varying consistencies of liquid and solid food and is most commonly reported with the eight-point penetration-aspiration scale.Reference Rosenbek, Robbins, Roecker, Coyle and Wood12
Interpreting videofluoroscopic swallow study results improves outcomes in dysphagia patients, offering the ability to determine appropriate modified dietary regimens with altered textures and consistencies that minimise risk of aspiration while supporting adequate nutritional and fluid intake.Reference Martin-Harris, Logemann, McMahon, Schleicher and Sandidge13 In addition to specified diet allocation, the videofluoroscopic swallow study can be used to guide clinical decision-making through the prescription of patient-tailored rehabilitation methods, altered positioning while eating or supporting restricted oral feeding.Reference Carnaby, Hankey and Pizzi14 The long-term outcomes of patients who undergo videofluoroscopic swallow study to guide treatment is not well understood. A recent study by Bock et al. (2017) evaluated the clinical outcomes of patients found to be at risk of aspiration but did not consider patients with low-risk swallow studies.Reference Bock, Varadarajan, Brawley and Blumin15 What remains unknown is the change in fluoroscopic outcomes for individual patients who undergo swallowing assessments over time.
The goal of this study was to evaluate the degree of dysphagia between sequential videofluoroscopic swallow studies in a cohort of patients evaluated at a tertiary out-patient dysphagia clinic, identify alterations in aspiration risk over time and assess the subsequent rate of pulmonary events following identification of abnormal swallowing function.
Materials and methods
Patient selection and data collection
This study was approved by the University of Calgary Conjoint Health Research Ethics Board (protocol number: 18-1332). A retrospective cohort was developed by identifying patients who underwent a videofluoroscopic swallow study at the Alberta Health Services Outpatient Dysphagia Clinic between 1 January 2018 and 31 December 2018 who had completed a prior videofluoroscopic swallow study assessment after 1 January 2012 at any facility in the Calgary Health Region. Health records were reviewed for basic demographic data including patient age, gender and diet allocation.
Dysphagia aetiology was assigned for each patient based on the listed reason for videofluoroscopic swallow study referral or admitting diagnosis and listed medical history. In cases with multiple potential aetiologies for dysphagia, the most severe or clinically relevant cause was selected. Fluoroscopic studies were performed according to regional Alberta Health Services standard protocols with patients challenged with barium swallow tests with consistencies that were thin, honey, nectar-thick, pureed, solid and mixed consistency, as deemed appropriate by the administering speech-language pathologist.
Videofluoroscopic swallow studies were evaluated according to the validated MBSImp™ protocol and penetration-aspiration scale scores were assigned for each trial consistency.Reference Martin-Harris, Brodsky, Michel, Castell, Schleicher and Sandidge16 Patients received barium paste in sandwich and cookie textures (EZ-Paste® 60 per cent w/w), barium powder in thick fluid textures (E-Z-HD™ 98 per cent w/w), and liquid barium with thin fluid textures (Polibar Plus® 105 per cent w/v). The fluoroscopic studies were recorded digitally with Siemens Artis Zee (Siemens Healthcare GmbH, Erlangen, Germany) or Siemens Axiom Luminos dRF (Siemens Healthcare GmbH, Erlangen, Germany).
Patients were categorised as low risk (penetration-aspiration scale = 1 or 2), medium risk (penetration-aspiration scale = 3 or 4) and high risk (penetration-aspiration scale more than 4) based on the highest risk, consistent videofluoroscopic swallow study observation. Patients’ dietary recommendations were assessed as a regular diet if no alterations were suggested. Any dietary modification in texture was categorised as a modified diet. Patients with nasogastric (NG) or percutaneous endoscopic gastrostomy (PEG) tubes were listed as nil per os. Pulmonary complications, PEG placement and surgical interventions occurring anytime in the 72-month study period were retrospectively obtained from Alberta Health Services analytics records and from patient charts. Pulmonary complications were defined as any emergency department visit or in-patient admission for pneumonia based on international classification of diseases 9 and international classification of diseases 10 codes that were noted on discharge records.
Statistical evaluation
Categorical data were summarised in tables and by frequencies. Descriptive statistics were reported as mean and standard deviation (SD) for continuous variables or frequencies and percentages for nominal variables. Statistically significant differences in repeated measurements at initial and final assessments within the groups were evaluated using the Wilcoxon signed rank test. The progression of penetration-aspiration scale score and dysphagia aetiology was investigated for the frequency of pulmonary events or other dysphagia-related complication and overall survival. Covariates of interest were compared between outcome groups using chi-square analysis and Fisher's exact test where appropriate. Probabilities for pneumonia development were calculated using the Kaplan–Meier estimator, and study groups were compared using the log rank test. Multivariable Cox proportional hazards regression was used to measure associations between the variables of interest (diet modification, age and sex) and penetration-aspiration scale score progression. All p-values were two sided, and the level of significance was set at less than 0.05. Statistical analysis was performed with Stata/MP (version 13.0) statistical software (StataCorp, College Park, USA).
Results
Patient demographic data
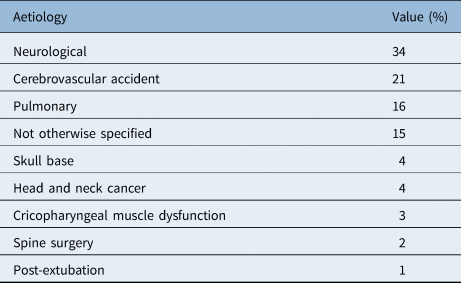
This study evaluated a total of 104 patients with videofluoroscopic swallow studies performed between 1 January 2018 and 31 December 2018 at our tertiary out-patient dysphagia centre who had completed a prior videofluoroscopic swallow study assessment after 1 January 2012 in the Calgary health region. Of the 104 patients reviewed, 55 patients were male (53 per cent) and 49 were female (47 per cent). The mean age of patients in our study population was 67.6 years (SD = 15.01) at their initial videofluoroscopic swallow study and 69.3 years (SD = 14.65) of age at their most recent videofluoroscopic swallow study assessment (Table 1). Table 2 shows that the most common diagnosis associated with dysphagia in our cohort was degenerative neurological condition (34 per cent), followed by stroke (cerebrovascular accident, 21 per cent), then respiratory condition (16 per cent). The aetiology of dysphagia was not otherwise specified in 15 per cent of our patients.
Table 1. Patient demographic data
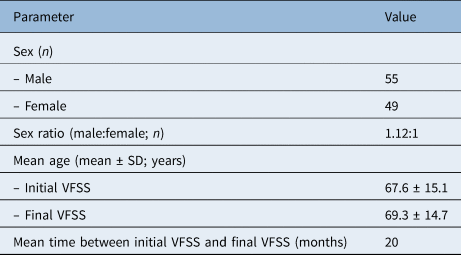
SD = standard deviation; VFSS = videofluoroscopic swallow
Table 2. Primary dysphagia aetiology
Risk categorisation and progression over time
Initial videofluoroscopic swallow study results placed 45.5 per cent of patients as high risk, whereas medium and low-risk patients comprised 9.9 per cent and 44.6 per cent of patients, respectively. Over time, the proportions shifted to high-risk in 51.5 per cent of the cohort, whereas medium-risk patients made up 11.9 per cent and low-risk patients were 36.6 per cent of the cohort (Table 3). When stratified by initial risk category, mean penetration-aspiration scale scores significantly increased in aspiration risk (p < 0.001; Table 3).
Table 3. Penetration-aspiration scale score progression

PAS = penetration-aspiration scale
Effect of dietary modification
Two-way measures of association to assess the relationship between dietary modification and the development of pneumonia compared patients with regular diets and diets with modified textures (Table 4). Fisher's exact test showed no association between presence of diet modification and the rates of pneumonia (p = 0.726).
Table 4. Association of diet modification and pneumonia

Pulmonary event and gastrostomy tube insertion
Univariate Kaplan–Meier analysis was performed for the duration of the study period to evaluate time to first pulmonary event and time to gastrostomy tube insertion for penetration-aspiration scale risk categories. Data demonstrating the relationship between penetration-aspiration scale score and pneumonia are demonstrated in Figure 1. All three risk category groups developed pneumonia at similar rates and there was no statistically significant difference on univariate analysis (p = 0.880). Moreover, there was no statistically significant difference between progression of penetration-aspiration scale score to a higher risk category and the development of pneumonia (Table 5). Figure 2 demonstrates penetration-aspiration scale risk stratification was not statistically significantly associated with time to gastrostomy tube insertion on univariate analysis (p = 0.796).

Fig. 1. Kaplan–Meier plot of time (months) to pulmonary event (pneumonia). Vertical lines indicate affected patients. Plot compares time to occurrence between patients at low (penetration-aspiration scale 1 or 2), medium (penetration-aspiration scale 3 or 4) and high risk (penetration-aspiration scale 5–8) for aspiration. Log-rank test, p = 0.880. PAS = penetration-aspiration scale
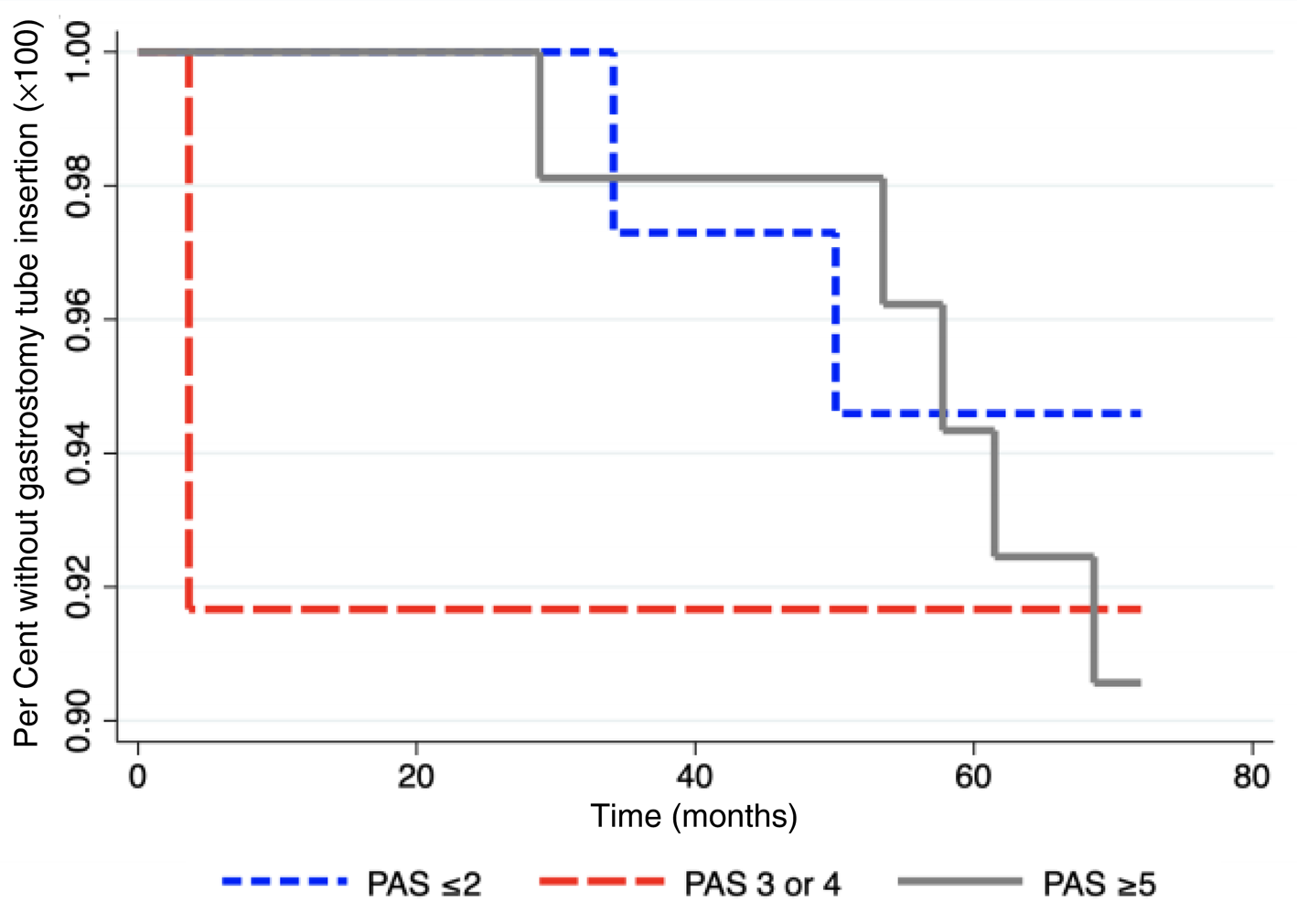
Fig. 2. Kaplan–Meier plot of time (months) to gastrostomy tube insertion. Vertical lines indicate affected patients. Plot compares time to occurrence between patients at low (penetration-aspiration scale 1 or 2), medium (penetration-aspiration scale 3 or 4) and high risk (penetration-aspiration scale 5–8) for aspiration. Log-rank test, p = 0.796. PAS = penetration-aspiration scale
Table 5. Association of penetration-aspiration scale score progression and pneumonia

PAS = penetration-aspiration scale
Dysphagia progression and aetiology
Two-way measures of association to evaluate correlation between the progression of dysphagia from a low or moderate risk category to a more severe category did not identify underlying diagnoses associated with worsening penetration-aspiration scale scores over time (Table 6). Fisher's exact test showed no association between presence of any of the nine dysphagia aetiologies present in our cohort and progression of penetration-aspiration scale risk categories (p = 0.758). Multivariate analysis to evaluate penetration-aspiration scale risk category progression demonstrated no significant differences in risk of progression when stratified by age or sex, although a trend (p = 0.052) for protective effect with dietary modification was observed (Table 7).
Table 6. Association of penetration-aspiration scale score progression and dysphagia aetiology

PAS = penetration-aspiration scale
Table 7. Multivariate analysis model for dysphagia progression

Discussion
Although it is assumed that patients with abnormal fluoroscopic swallowing studies are at risk for dysphagia complications, little is written in the literature demonstrating the clinical course of patients with dysphagia. In particular, sparse data exist to demonstrate the predictive power of videofluoroscopic swallow study in the progression of dysphagia and its complications. Given the wide range of pathology that may result in swallowing dysfunction, it is not clear whether the presence of particular risk factors enhance aspiration risk, nor is it understood what constitutes the most effective methods to predict aspiration events.Reference Bock, Varadarajan, Brawley and Blumin15
Our study followed 104 patients who underwent a videofluoroscopic swallow study in 2018 in addition to a previous study completed within the preceding 6 years. We found that for a subset of patients swallowing function deteriorates, but this is less than half of the total population. Worsening of swallowing function was independent of age, sex and diet modification in a multivariate model. We also attempted to correlate the underlying aetiology with worsening aspiration score; however, no dysphagia aetiologies differed significantly in the rate of progression.
The videofluoroscopic swallow study is the most robust and frequently used swallowing investigation to determine aspiration risk and appropriate diet allocation, with most practitioners utilising the penetration-aspiration scale because of its strong inter- and intra-rater reliability regardless of clinician experience and retest interval.Reference Martin-Harris, Brodsky, Michel, Castell, Schleicher and Sandidge16 Prior studies have investigated association between dysphagia and aspiration risk, although only high-risk patients were included in the data sets. A significant association was not detected for high-risk penetration-aspiration scale score and pulmonary events; therefore, there remains controversy regarding penetration-aspiration scale scores as predictors of pulmonary events and subsequent mortality.Reference Bock, Varadarajan, Brawley and Blumin15,Reference Butler, Markley, Sanders and Stuart17 Our data were in accordance with the available literature and suggest that during our study period the penetration-aspiration scale score categories were poor predictors of pneumonia development.
In our analysis, we attempted to identify if penetration-aspiration scale risk scores could predict the need for PEG tubes, which is a controversial topic. No correlation was identified between penetration-aspiration scale risk categories and the need for surgical intervention. In contrast, in a retrospective analysis of patients with neurological dysphagia, a statistically significant decrease in the number of pneumonia episodes among patients receiving PEG feeds was observed when compared to NG feeds.Reference Azzopardi and Ellul18 Brown et al. (2018) evaluated the utility of the penetration-aspiration scale in predicting PEG tube placement among a sub-group of patients with ischemic stroke who had failed an initial bedside evaluation by a speech-language pathologist. They found high penetration-aspiration scale scores of 6–8 and moderate penetration-aspiration scale scores of 3–5 were associated with increased odds of PEG tube placement, but their study was not able to evaluate long-term clinical outcomes or swallow function.Reference Brown, Cai, Barreto, Shoemaker, Woellner and Vu19
Limited data are available regarding the efficacy of intervention in the prevention of pulmonary events, changes in patient's perception of swallowing severity over time and long-term outcomes following treatments.Reference Pitts20,Reference Altman21 The use of modified diet textures and thickened liquids has become a cornerstone of clinical practice to address swallowing dysfunction, yet the efficacy of this has been brought into question in the literature.Reference Bock, Varadarajan, Brawley and Blumin15,Reference Garcia, Chambers and Molander22 Furthermore, although modification of food texture has been shown to alter food bolus transit time, theoretically reducing the risk of aspiration, the correlation to reduced rates of pneumonia development is modest.Reference Barbon and Steele23 Our data did not show any correlation with rates of pneumonia with nil per os status or diet texture modification, albeit with a low incidence of pneumonia in our cohort. Given the drastic effect on patient quality of life that a restrictive diet or nil per os status may have and the controversy regarding the efficacy of its potential protective mechanism against aspiration, diet modification recommendations may play a smaller role in the management of the dysphagia patient.
There are several limitations in our study that should be considered. First, it is difficult to draw conclusions regarding risk of pneumonia based on diet allocation because patients are placed on modified diet or nil by mouth restrictions because of swallowing dysfunction, and this intervention should reduce the risk of developing pneumonia. Our data indicate no correlation between diet allocation and pneumonia development, which could represent a protective effect of diet changes or lack of therapeutic effectiveness to prevent pneumonia. We are unable to evaluate diet allocation adherence and whether patients who developed pneumonia followed the recommended diets. Our analysis was retrospective in nature and lacks the ability of a prospective study to follow the effect of diet modification and predict risk categorisation by penetration-aspiration scale scores. In addition, there are clinical parameters that may contribute to swallowing dysfunction over time in this population, but these parameters were unavailable or insufficiently completed in the health records, including subjective swallowing scores such as the eating assessment tool-10, reflux symptom index, adherence to dietary recommendations and frailty scores. Finally, our patient population was derived from a tertiary out-patient dysphagia clinic and had clinical concern prompting a repeat videofluoroscopic swallow study independent of the original study indication, which suggests this cohort may be at higher risk for progressive swallow decline compared with the general population. This potentially limits generalisability to a wider population.
• Changes in fluoroscopic outcomes for individual patients have not been previously investigated
• This study demonstrated mean worsening of swallowing impairment over time using radiological assessment
• Severity of aspiration defined by penetration-aspiration scale did not identify differences in survival
• Dietary modifications showed no association with occurrence of pulmonary events or aspiration
• Correlation between potential prognostic factors and risk of progressive swallowing difficulty is needed
Conclusion
We identified a cohort of 104 patients who had undergone multiple videofluoroscopic swallow studies, which were on average more than 18 months apart. Overall, our findings suggest that penetration-aspiration scale scores used in videofluoroscopic swallow study do not predict clinical outcomes, and no individual risk factor predicted the likelihood for penetration-aspiration scale severity to progress over time.
Acknowledgements
The authors acknowledge the Speech Language Pathologists of the Peter Lougheed Outpatient Dysphagia Clinic involved in interpreting the fluoroscopic studies, Mark Lychak for assistance with cohort identification and Mu Lin for data extraction through Alberta Health Services Analytics.
Competing interests
None declared











