A neural diathesis-stress conception of psychosis (Walker & Diforio, Reference Walker and Diforio1997; Walker, Mittal, & Tessner, Reference Walker, Mittal and Tessner2008) suggests that vulnerabilities during the pre-illness (i.e., premorbid) period in childhood and early adolescence interact with normative/pathological development and environmental stressors throughout adolescence and young adulthood to drive the onset of psychosis. However, while the earliest premorbid stage of the illness is generally viewed as an important time for understanding etiology, and for intervention, research in this area has been surprisingly limited. As a result, we know there are nonspecific signs of social, cognitive, and motor dysfunction (Lieberman et al., Reference Lieberman, Perkins, Belger, Chakos, Jarskog, Boteva and Gilmore2001; Schenkel & Silverstein, Reference Schenkel and Silverstein2004; Tandon, Keshavan, & Nasrallah, Reference Tandon, Keshavan and Nasrallah2008), but areas of specific dysfunction in critical domains remain poorly understood. For example, social communication (i.e., verbal and nonverbal social behaviors required for successful social interactions; Brekke, Kay, Lee, & Green, Reference Brekke, Kay, Lee and Green2005; Dickinson, Bellack, & Gold, Reference Dickinson, Bellack and Gold2006) is significantly impaired in psychosis (Kohler et al., Reference Kohler, Martin, Stolar, Barrett, Verma, Brensinger and Gur2008; Mattes, Schneider, Heimann, & Birbaumer, Reference Mattes, Schneider, Heimann and Birbaumer1995; Walther et al., Reference Walther, Stegmayer, Sulzbacher, Vanbellingen, Müri, Strik and Bohlhalter2015), and related foundational skills are in ascendance in the developmental stages overlapping with the premorbid period (Darling-Churchill & Lippman, Reference Darling-Churchill and Lippman2016; Masten et al., Reference Masten, Desjardins, McCormick, Sally, Kuo and Long2010; McCabe & Altamura, Reference McCabe and Altamura2011; Mikami, Szwedo, Allen, Evans, & Hare, Reference Mikami, Szwedo, Allen, Evans and Hare2010), but to date, there have been no studies aimed to determine normative from pathological development, or to determine how this may ultimately impact later risk in the adolescent/young-adult prodromal period. The present study investigates early premorbid social skill impairment (ages 4–5) in adolescents and young adults diagnosed with a prodromal syndrome and aims to determine if impairments occur at this early stage and how they may impact later susceptibility to psychosis in the high-risk prodromal period.
Neurodevelopment and Risk for Psychosis
Current neurodevelopmental models of schizophrenia posit that the fundamental pathophysiology underlying the illness is present in childhood and early adolescence before distinct positive symptomology and marked functional decline become evident in late adolescence and early adulthood (Pruessner, Cullen, Aas, & Walker, Reference Pruessner, Cullen, Aas and Walker2017). Several lines of evidence from cross-sectional research in children and adolescents, as well as prospective longitudinal cohort studies, support this assertion (see Liu, Keshavan, Tronick, & Seidman, Reference Liu, Keshavan, Tronick and Seidman2015,)for a review). For example, a myriad of abnormal motor behaviors have been used to identify toddlers and children who ultimately develop adult schizophrenia, including delays in achieving motor milestones (Filatova et al., Reference Filatova, Koivumaa-Honkanen, Hirvonen, Freeman, Ivandic, Hurtig and Miettunen2017; Sørensen et al., Reference Sørensen, Mortensen, Schiffman, Reinisch, Maeda and Mednick2010), unusual movements and clumsiness (Walker & Lewine, Reference Walker and Lewine1990), neuromotor deficits and involuntary movements (Kindler et al., Reference Kindler, Schultze-Lutter, Michel, Martz-Irngartinger, Linder, Schmidt and Walther2016; Schiffman et al., Reference Schiffman, Sorensen, Maeda, Mortensen, Victoroff, Hayashi and Mednick2009), and neurological soft signs (Crow, Done, & Sacker, Reference Crow, Done and Sacker1995; Rosso et al., Reference Rosso, Bearden, Hollister, Gasperoni, Sanchez, Hadley and Cannon2000). Moreover, childhood neurocognitive deficits are well evidenced (see Woodberry, Giuliano, & Seidman, Reference Woodberry, Giuliano and Seidman2008,)for a review) and are present as early as age 4 in children who develop schizophrenia spectrum disorders in adulthood (Agnew-Blais et al., Reference Agnew-Blais, Seidman, Fitzmaurice, Smoller, Goldstein and Buka2017; Seidman et al., Reference Seidman, Cherkerzian, Goldstein, Agnew-Blais, Tsuang and Buka2013). Together, early cognitive deficits and behavioral abnormalities are considered to characterize the asymptomatic premorbid stage of the illness wherein children and adolescents harbor a biological vulnerability for developing future psychosis but do not yet manifest the clinical symptomology (e.g., hallucinations or delusions) and significant functional impairment characteristic of the illness. However, it is important to note that the age period comprising the premorbid stage in neurodevelopmental models of psychosis is conceptual in nature and does not always reflect the considerable heterogeneity evident in individuals who develop psychosis. Thus, conceptual definitions of the premorbid period typically span from gestation to early adolescence whereas it is not uncommon for the premorbid period to last into adolescence for some affected individuals. For the present paper, we define the premorbid period as spanning through early adolescence; however, we will focus on early childhood as deficits during this period have been less well defined.
In contrast to the premorbid period, the prodromal stage of the illness is characterized by attenuated positive (e.g., momentarily formed hallucinations or loosely held delusions) and negative (e.g., blunted affect or amotivation) symptoms that are accompanied by a functional and neurocognitive decline (Miller et al., Reference Miller, McGlashan, Rosen, Cadenhead, Ventura, McFarlane and Woods2003). Because increased duration of untreated psychosis results in poorer prognosis (Penttilä, Jääskeläinen, Hirvonen, Isohanni, & Miettunen, Reference Penttilä, Jääskeläinen, Hirvonen, Isohanni and Miettunen2014), research aimed at identifying who is most likely to transition to a psychotic disorder has become a priority. Consistent with this effort, the clinical high-risk (CHR) approach (Miller et al., Reference Miller, McGlashan, Rosen, Cadenhead, Ventura, McFarlane and Woods2003) is often utilized to identify factors that predict conversion in order to implement early interventions aimed at reducing transition. Youth at CHR for psychosis are considered to be exhibiting a putative prodromal syndrome. However, research indicates that only 35% of individuals identified as CHR will ultimately transition to a psychotic disorder (Addington et al., Reference Addington, Liu, Buchy, Cadenhead, Cannon, Cornblatt and Walker2015), leading many to suggest a need for the development of vulnerability markers that will aid in refining identification and enhancing prediction (Mittal & Walker, Reference Mittal, Walker and Ritsner2009). To date, prediction models (see Schmidt et al., Reference Schmidt, Cappucciati, Radua, Rutigliano, Rocchetti, Dell'Osso and Valmaggia2017) have emphasized current risk markers (e.g., prodromal symptoms and neurocognition) and do not typically include premorbid vulnerability markers in risk indices. Given that recent evidence indicates that the inclusion of premorbid social functioning in early adolescence improves prediction of conversion in individuals at CHR for psychosis (Tarbox et al., Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013; Walder et al., Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013), examining the utility of other premorbid social behaviors, such as early childhood social communication, may be valuable.
Premorbid Social Dysfunction in Psychosis Populations
General social dysfunction in the premorbid period of psychosis is well evidenced. Preference for solitary play at ages 4 and 6 is associated with adult-onset schizophrenia (Jones, Murray, & Rodgers, Reference Jones, Murray, Rodgers, Mednick and Hollister1995). Prospective population cohort studies have shown that social maladjustment at age 7 predicts adult-onset schizophrenia (Bearden et al., Reference Bearden, Rosso, Hollister, Sanchez, Hadley and Cannon2000; Done, Crow, Johnstone, & Sacker, Reference Done, Crow, Johnstone and Sacker1994). Tarbox and Pogue-Geile (Reference Tarbox and Pogue-Geile2008) conducted a systematic review of prospective and retrospective studies examining domains of social functioning in genetic high-risk samples and the general population. Results indicated that undifferentiated social functioning (i.e., measures that did not distinguish among social behaviors) at age 7 to 8 predicted adult-onset schizophrenia in the general population, and even earlier (age 5 to 6) in genetic high-risk samples. Social withdrawal-internalizing behavior (e.g., preference for solitary activities or social anxiety) was predictive from age 11 in the general population, but not in genetic high-risk samples. Using retrospective reporting, it has been shown that patients with schizophrenia exhibit more impairments in sociability (e.g., social withdrawal, poor peer relationships, and asociality) in both childhood (ages 5–11) and adolescence (age 12–16) compared to controls (Cannon et al., Reference Cannon, Jones, Gilvarry, Rifkin, McKenzie, Foerster and Murray1997). In addition, premorbid social withdrawal and impairments in peer relationships are present in over 50% of children with early onset schizophrenia (i.e., by the age of 15; Kolvin, Reference Kolvin1971; Nicolson et al., Reference Nicolson, Lenane, Singaracharlu, Malaspina, Giedd, Hamburger and Fernandez2000). Furthermore, social maladjustment in both early (age 12–15) and late (age 16–18) adolescence predicts conversion to schizophrenia in CHR youth (Dragt et al., Reference Dragt, Nieman, Veltman, Becker, van de Fliert, de Haan and Linszen2011; Lyngberg et al., Reference Lyngberg, Buchy, Liu, Perkins, Woods and Addington2015; Tarbox et al., Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013, Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2014; Walder et al., Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013).
In addition to predicting conversion, several studies have used retrospective self-report to examine the relationship between premorbid social dysfunction in childhood and later symptom severity and functioning in CHR youth and patients with schizophrenia. Using cluster analysis, it has been shown that CHR youth who had deteriorating overall premorbid functioning (which includes social and role measures) from childhood to late adolescence exhibited more severe negative symptoms and poorer social functioning than CHR youth with more stable premorbid developmental trajectories (Lyngberg et al., Reference Lyngberg, Buchy, Liu, Perkins, Woods and Addington2015). Similarly, when examining developmental trajectories of overall premorbid adjustment, patients who had a deteriorating course from childhood to adulthood developed prodromal syndromes approximately 5 years earlier, achieved a lower level of education (1.5 years less), and had more severe impairments in processing speed and psychosocial functioning (Cole, Apud, Weinberger, & Dickinson, Reference Cole, Apud, Weinberger and Dickinson2012). Similar classification methods have demonstrated associations with various premorbid social impairment trajectories and both positive and negative symptom severity in patients with schizophrenia (Addington & Addington, Reference Addington and Addington2005; Addington, van Mastrigt, & Addington, Reference Addington and Addington2003; Chang et al., Reference Chang, Tang, Hui, Wong, Chan, Lee and Chen2013; Horton, Tarbox, Olino, & Haas, Reference Horton, Tarbox, Olino and Haas2015; Strauss et al., Reference Strauss, Allen, Miski, Buchanan, Kirkpatrick and Carpenter2012; Walder et al., Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013); however, associations with positive symptoms were found less consistently (Addington & Addington, Reference Addington and Addington2005; Addington et al., Reference Addington, van Mastrigt and Addington2003; Walder et al., Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013). Taken together, once present, premorbid social impairments in early childhood appear to either persist or progress throughout development and are closely associated with symptom severity and functional outcomes (Childers & Harding, Reference Childers and Harding1990). Despite evidence for general social dysfunction in the premorbid period, very little research has examined impairments in specific critical domains that facilitate effective social functioning that are in ascendance during early childhood, such as social communication. Furthermore, early childhood social communication is a broad construct that encompasses several domains of behavior, such as social reciprocity (e.g., smiling, eye gaze, and group play) and communication (e.g., gesture and imitation), that have yet to be examined in early childhood in a CHR sample.
Social Communication Across Stages of Psychosis
Social communication comprises both specific verbal and nonverbal behaviors that facilitate effective and appropriate interpersonal communication (Rao, Beidel, & Murray, Reference Rao, Beidel and Murray2008). Examples of social communication in early childhood include behaviors such as responding to questions, making eye contact, smiling, spontaneous play, offering to share or comfort, social interest, imitation, and gestures (Rutter, Bailey, & Lord, Reference Rutter, Bailey and Lord2003). These social skills are often divided into distinct domains such as reciprocal social interaction (e.g., seeking to share enjoyment, offering comfort, and interest in other children) and communication (e.g., social chat, gestures, and imitation; Martínez-Pedraza & Carter, Reference Martínez-Pedraza and Carter2009; Rutter et al., Reference Rutter, Bailey and Lord2003; Solomon et al., Reference Solomon, Olsen, Niendam, Ragland, Yoon, Minzenberg and Carter2011). Currently, only a handful of studies have investigated premorbid social communication in psychosis spectrum populations. For example, impairments have been shown in language and speech development, with delays in speech acquisition and abnormal language use present from toddlerhood to late adolescence (Jones, Murray, Rodgers, & Marmot, Reference Jones, Murray, Rodgers and Marmot1994). Furthermore, Esterberg, Trotman, Brasfield, Compton, and Walker (Reference Esterberg, Trotman, Brasfield, Compton and Walker2008) used parent interviews to examine several domains of childhood social communication in adolescents with schizotypal personality disorder. Schizotypal personality disorder is on the mildest end of the schizophrenia spectrum and is characterized by trait-level psychotic-like experiences (e.g., magical thinking or suspiciousness) that do not typically result in the prolonged functional impairment seen in psychosis (Chemerinski, Triebwasser, Roussos, & Siever, Reference Chemerinski, Triebwasser, Roussos and Siever2013; Esterberg et al., Reference Esterberg, Trotman, Brasfield, Compton and Walker2008). They found that, compared to controls, adolescents with schizotypal personality disorder exhibited more impairments in a wide range of childhood reciprocal social interaction behaviors, such as social smiling, range of facial expressions, sharing, eye gaze, spontaneous group play, and social avoidance. However, early childhood social communication was not associated with positive or negative symptoms or conversion to formal psychosis in schizotypal personality disorder adolescents. Schiffman et al. (Reference Schiffman, Walker, Ekstrom, Schulsinger, Sorensen and Mednick2004) used videos of children (ages 11–13) eating lunch to determine if social communication behaviors discriminate among children who ultimately develop schizophrenia. Children who developed schizophrenia exhibited significantly less social reciprocity and communication (e.g., number of smiles and laughs, or vocalization initiated by child) during the videotaped social interactions compared to both children who did not develop a psychiatric disorder and those who developed other psychiatric illnesses.
Although research on social communication deficits in the premorbid period is limited, deficits in these domains are well evidenced in individuals at CHR for psychosis and in schizophrenia patients. Using parent report, Solomon et al. (Reference Solomon, Olsen, Niendam, Ragland, Yoon, Minzenberg and Carter2011) demonstrated that individuals at CHR for psychosis reported substantially more impairments in communication and social reciprocity than typically developing adolescents. For example, CHR youth reported deficits in interpersonal expressiveness, conversational give-and-take, interest in socialization, and ability to interpret and respond to social cues. In addition, Gibson, Penn, Prinstein, Perkins, and Belger (Reference Gibson, Penn, Prinstein, Perkins and Belger2010) found that individuals at genetic high-risk for psychosis exhibited impairments in subdomains of social communication behaviors, such as fluency of speech, nonverbal affect, eye gaze, social anxiety, and engagement during a mock audition. Furthermore, gesture abnormalities, including both mismatched gestures and decreased gesture use, are present in CHR populations (Millman et al., Reference Millman, Goss, Schiffman, Mejias, Gupta and Mittal2014; Osborne et al., Reference Osborne, Bernard, Gupta, Dean, Millman, Vargas and Mittal2017). Pinkham, Penn, Perkins, Graham, and Siegel (Reference Pinkham, Penn, Perkins, Graham and Siegel2007) showed that CHR young adults exhibited poorer global and nonverbal social skills compared to nonclinical controls. Furthermore, patients with schizophrenia are impaired in a wide array of verbal and nonverbal social communication behaviors, such as reciprocal prosocial behavior, spontaneous imitation, facial expressions, eye contact, and gesture use (Kohler et al., Reference Kohler, Martin, Stolar, Barrett, Verma, Brensinger and Gur2008; Mattes et al., Reference Mattes, Schneider, Heimann and Birbaumer1995; Walther et al., Reference Walther, Stegmayer, Sulzbacher, Vanbellingen, Müri, Strik and Bohlhalter2015). Moreover, abnormal nonverbal synchrony (i.e., dynamic imitation during interpersonal conversation) in patients with schizophrenia has been associated with symptom severity and poorer social functioning, as well as poorer therapeutic outcomes (Kupper, Ramseyer, Hoffmann, & Tschacher, Reference Kupper, Ramseyer, Hoffmann and Tschacher2015; Ramseyer & Tschacher, Reference Ramseyer and Tschacher2011; Vail et al., Reference Vail, Baltrušaitis, Pennant, Liebson, Baker and Morency2017), indicating that real-world social communication impairments have important implications for treatment outcomes.
Rationale for Present Study
While there has been little work done to examine how social communication may be impacted in the premorbid period in schizophrenia spectrum disorders, it is important to consider that this stage overlaps with a critical developmental period where skills underlying social development are in ascendance. Early childhood, particularly the 3- to 5-year period, is critical for the development of social skills required for effective communication and reciprocal social interaction, such as nonverbal communication (e.g., gesture and facial expressions; Dil, Reference Dil1984; Knott, Reference Knott1979), imitation (Dickerson, Gerhardstein, Zack, & Barr, Reference Dickerson, Gerhardstein, Zack and Barr2013; DiYanni, Nini, Rheel, & Livelli, Reference DiYanni, Nini, Rheel and Livelli2012), prosocial behavior (i.e., sharing and responding to social engagement; Caprara, Barbaranelli, Pastorelli, Bandura, & Zimbardo, Reference Caprara, Barbaranelli, Pastorelli, Bandura and Zimbardo2000; Findlay, Girardi, & Coplan, Reference Findlay, Girardi and Coplan2006), and spontaneous play (Johnson, Ershler, & Lawton, Reference Johnson, Ershler and Lawton1982). Developing effective social skills in early childhood then sets the stage for social functioning throughout adolescence and early adulthood (Caprara et al., Reference Caprara, Barbaranelli, Pastorelli, Bandura and Zimbardo2000; Darling-Churchill & Lippman, Reference Darling-Churchill and Lippman2016; McCabe & Altamura, Reference McCabe and Altamura2011; Mikami et al., Reference Mikami, Szwedo, Allen, Evans and Hare2010). Given that evidence suggests that premorbid social dysfunction present in early childhood persists throughout development in CHR youth and patients with schizophrenia (Dragt et al., Reference Dragt, Nieman, Veltman, Becker, van de Fliert, de Haan and Linszen2011; Lyngberg et al., Reference Lyngberg, Buchy, Liu, Perkins, Woods and Addington2015; Tarbox et al., Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013, Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2014), and that these trajectories are associated with functional outcomes and symptom severity (Dragt et al., Reference Dragt, Nieman, Veltman, Becker, van de Fliert, de Haan and Linszen2011; Lyngberg et al., Reference Lyngberg, Buchy, Liu, Perkins, Woods and Addington2015; Tarbox et al., Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013, Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2014), examining if similar relationships are present with premorbid social communication deficits is warranted. In particular, examining early childhood social communication in CHR youth (i.e., whether these skills develop differently in high-risk and typically developing populations, and whether deficits predict later functioning and psychosis risk) stands to inform the field's understanding of the etiology and pathophysiology of psychosis during critical developmental periods overlapping with the premorbid and prodromal stages of psychosis.
The present study is the first to examine social communication deficits in the early premorbid period (i.e., early childhood) in a CHR sample in the putative prodromal stage of the illness, and their association with CHR youth's current social and role functioning, symptom severity, and risk for developing psychosis. Although distinct domains of premorbid early childhood social communication (i.e., reciprocal social interaction and communication) have been examined in youth with schizotypal personality disorder (Esterberg et al., Reference Esterberg, Trotman, Brasfield, Compton and Walker2008), no such research has been conducted in adolescents and young adults at CHR for psychosis. Furthermore, no research to date has linked social communication deficits in the early childhood premorbid stage with functioning and symptom severity in the prodromal stage or examined their utility for understanding additive risk in the prodromal period.
Based on findings indicating that premorbid deficits in reciprocal social interaction and communication are present in early adolescence among individuals that later develop psychosis (Schiffman et al., Reference Schiffman, Walker, Ekstrom, Schulsinger, Sorensen and Mednick2004), coupled with research showing similar social communication deficits in CHR and schizophrenia samples (Pinkham et al., Reference Pinkham, Penn, Perkins, Graham and Siegel2007; Solomon et al., Reference Solomon, Olsen, Niendam, Ragland, Yoon, Minzenberg and Carter2011; Walther & Mittal, Reference Walther and Mittal2016), we predicted that parents of CHR adolescents and young adults would report more early childhood social communication deficits compared to parents of healthy controls. Moreover, we predicted that deficits would be present in specific social communication domains including communication and reciprocal social interaction. Relatedly, the study examined if early childhood social communication deficits contributed to current deficits in social functioning in the CHR adolescents and young adults. Based on findings that CHR youth with declines in overall premorbid functioning from childhood to late adolescence exhibit poorer social functioning than those with stable trajectories (Lyngberg et al., Reference Lyngberg, Buchy, Liu, Perkins, Woods and Addington2015), and that social skills in early childhood predict functioning throughout adolescence and early adulthood in typically developing children (Caprara et al., Reference Caprara, Barbaranelli, Pastorelli, Bandura and Zimbardo2000; Darling-Churchill & Lippman, Reference Darling-Churchill and Lippman2016; McCabe & Altamura, Reference McCabe and Altamura2011; Mikami et al., Reference Mikami, Szwedo, Allen, Evans and Hare2010), we predicted that more early childhood social communication deficits would be associated with poorer current social functioning in CHR youth. Given that early childhood social functioning predicts later academic achievement in typically developing children (Arnold, Kupersmidt, Voegler-Lee, & Marshall, Reference Arnold, Kupersmidt, Voegler-Lee and Marshall2012; McCabe & Altamura, Reference McCabe and Altamura2011; Rabiner, Godwin, & Dodge, Reference Rabiner, Godwin and Dodge2016), and that social and role functioning (i.e., academic and work functioning) are typically examined together in CHR research (Cornblatt et al., Reference Cornblatt, Auther, Niendam, Smith, Zinberg, Bearden and Cannon2007; Meyer et al., Reference Meyer, Carrión, Cornblatt, Addington, Cadenhead, Cannon and Walker2014; Mittal et al., Reference Mittal, Jalbrzikowski, Daley, Roman, Bearden and Cannon2011; Walder et al., Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013), we also examined if early childhood social communication deficits were associated with current role functioning. Finally, we aimed to examine if including early risk factors, such as social communication, occurring prior to the CHR period, might enhance predictive ability, highlighting those CHR individuals at highest risk for transitioning to a psychotic disorder. Based on findings showing the utility of premorbid social functioning in early adolescence for improving conversion prediction (Tarbox et al., Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013; Walder et al., Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013), we predicted that early childhood social communication deficits would be associated with symptom severity and increased risk for conversion in CHR youth.
Method
Participants
Data for the present study were obtained from 44 CHR and 38 healthy control (HC) youth (total N = 82) and their primary caregivers during their participation in a study of motor behavior and psychosis risk (see Table 1 for demographic characteristics). CHR participants were required to meet the Structured Interview for Prodromal Syndromes (SIPS; Miller et al., Reference Miller, McGlashan, Woods, Stein, Driesen, Corcoran and Davidson1999) criteria for a prodromal syndrome (i.e., clinical high-risk) in order to be included in the study. Criteria for a prodromal syndrome included one or more of the following: (a) progression or recent onset of attenuated positive symptoms, (b) the presence of a first-degree relative with a psychotic disorder accompanied by a recent decline in global functioning, or (c) a decline in global functioning with the presence of schizotypal personality disorder (Miller et al., Reference Miller, McGlashan, Woods, Stein, Driesen, Corcoran and Davidson1999). Exclusion criteria for both groups included any neurological disorder, history of head injury, lifetime substance dependence, or any past or current psychotic disorder (e.g., schizophrenia, etc.). For HCs, the presence of a psychotic disorder in a first-degree relative and any past or current Axis I disorders were additional exclusionary criterions. Because we are interested in examining social communication deficits putatively specific to psychosis, we also excluded participants with any diagnosis of autism spectrum disorder (n = 1 CHR). Thus, the final sample consisted of 43 CHR and 38 HC participants (total N = 81). CHR and HC individuals were recruited via newspaper ads, Craigslist, e-mail postings, and community professional referrals. Informed consent was obtained in accordance with the protocol approved by the institutional review board. Assent was obtained for individuals younger than 18 with informed consent obtained from their legal guardian.
Table 1. Demographic characteristics with group comparisons

Note: CHR, clinical high-risk. HC, healthy controls. Statistic reflects test of group differences for each demographic variable. ns, nonsignificant.
Materials and procedure
Semistructured clinical and socio-occupational functioning interviews were administered to CHR and HC adolescents and young adults at the Adolescent Development and Preventative Treatment Program. Parents or legal guardians completed self-report questionnaires.
Clinical interviews
The SIPS (Miller et al., Reference Miller, McGlashan, Woods, Stein, Driesen, Corcoran and Davidson1999) was administered to determine if a prodromal syndrome was present (as noted above) and to quantify attenuated psychosis symptoms. The SIPS assesses several dimensions of attenuated positive and negative symptomology. SIPS positive symptomology is composed of dimensions reflecting unusual thought content, perceptual abnormalities, grandiosity, disorganized communication, and suspiciousness. Negative symptom dimensions include avolition, social anhedonia, ideational richness, emotional expressiveness, blunted affect, and occupational functioning. All symptoms are rated on 0 to 6 scales. Scores for the positive symptom domain range from absent (score of 0) to severe and psychotic (score of 6; e.g., delusional conviction and/or hallucinations perceived as real that persistently interfere with thinking, feeling, and behavior). Negative symptoms range from absent (score of 0) to extreme (score of 6; e.g., absence of any goal directed activities, no feelings, or flat affect). Sum scores for each symptom domain were used to quantify the severity of positive and negative symptoms. In addition, the Structured Clinical Interview for Axis I DSM-IV Disorders (SCID; First, Spitzer, Gibbon, & Williams, Reference First, Spitzer, Gibbon and Williams1995) was administered in order to rule out an Axis I psychotic disorder and to note the occurrence of any comorbid conditions. Clinical interviews were administered by advanced doctoral students with interrater reliabilities that exceeded the minimum study criterion of κ ≥ 80. Both the SIPS (Cannon et al., Reference Cannon, Cadenhead, Cornblatt, Woods, Addington, Walker and McGlashan2008; Miller et al., Reference Miller, McGlashan, Rosen, Cadenhead, Ventura, McFarlane and Woods2003; Miller et al., Reference Miller, McGlashan, Rosen, Somjee, Markovich, Stein and Woods2002) and the SCID (Lobbestael, Leurgans, & Arntz, Reference Lobbestael, Leurgans and Arntz2011) have high validity, adequate to excellent interrater reliability, and have been used extensively in studies with CHR adolescents and young adults.
Social and role functioning
Social and role functioning were measured using two scales explicitly designed for CHR populations: the Global Functioning Scale: Social (GFS-S; Auther, Smith, & Cornblatt, Reference Auther, Smith and Cornblatt2006) and Global Functioning Scale: Role (GFS-R; Niendam, Bearden, Johnson, & Cannon, Reference Niendam, Bearden, Johnson and Cannon2006). Scores on both scales range from 1 to 10. A score of 1 on the GFS-S indicates extreme social isolation (e.g., no friends or contact with family), whereas a score of 10 reflects superior social/interpersonal functioning (e.g., multiple satisfying close and casual interpersonal relationships or frequently seeks out others). On the GFS-R, a score of 1 indicates extreme role dysfunction (e.g., on disability or equivalent nonindependent status) and a score of 10 represents superior role functioning (e.g., superior performance in competitive school or work placement). These scales were developed to be used with adolescents and young adults and have been shown to be valid and reliable in CHR populations (Cornblatt et al., Reference Cornblatt, Auther, Niendam, Smith, Zinberg, Bearden and Cannon2007).
Early premorbid social communication
Because there are currently no scales designed for evaluating early social communication developmental deficits in the premorbid period, the present investigation adapted the Social Communication Questionnaire Lifetime Form (SCQ; Rutter et al., Reference Rutter, Bailey and Lord2003), a well-validated, parent-report questionnaire developed as a screening measure for social dysfunction associated with autism spectrum disorder. Although the scale was developed for autism, it has been used in other research in schizophrenia spectrum populations (Solomon et al., Reference Solomon, Olsen, Niendam, Ragland, Yoon, Minzenberg and Carter2011), and contains several domains that overlap with early social communication behaviors that may be affected in the early premorbid period. For a subset of questions, parents are instructed to identify if a particular social communication deficit was present during their child's 4- to 5-year-old age period, whereas the rest of the items focus on the child's entire developmental history. For the purpose of the present study, the adaptation involved (a) administering the scale to parents of CHR and HC individuals instead of parents of individuals with autism, and (b) administering those SCQ items that specifically covered the early childhood (i.e., 4- to 5-age period) period of interest (see Table 3). Items on the questionnaire assess for qualitative deviance in children's social interactions (e.g., interest in other children, social responsiveness, and eye gaze) and verbal and nonverbal communication (e.g., reciprocal communication and conventional gesture use). These items comprise two distinct SCQ subdomains, reciprocal social interaction and communication, as well as an SCQ total score.
Conversion risk
Risk for conversion to psychosis was measured using a freely available risk calculator (http://riskcalc.org/napls/) developed by the North American Prodrome Longitudinal Study (NAPLS; Cannon et al., Reference Cannon, Yu, Addington, Bearden, Cadenhead, Cornblatt and McGlashan2016). The NAPLS risk calculator was designed to provide an individualized risk score indexing the probability of converting to formal psychosis specifically for individuals diagnosed as CHR based on the aforementioned SIPS criteria. The calculations are based on a multivariate proportional hazards regression model that includes several demographic, cognitive, and psychosocial variables, including age, Brief Assessment of Cognition in Schizophrenia symbol coding score (Keefe et al., Reference Keefe, Goldberg, Harvey, Gold, Poe and Coughenour2004), the Hopkins Verbal Learning Test-Revised sum score (Trials 1–3; Brandt & Benedict, Reference Brandt and Benedict2001), negative life event sum scores from the Research Interview Life Events Scale (Dohrenwend, Askenasy, Krasnoff, & Dohrenwend, Reference Dohrenwend, Askenasy, Krasnoff and Dohrenwend1978), change in GFS-S score from 12 months prior, severity of unusual thought content and suspiciousness (rescaled from SIPS scores), family history of psychosis, and the total number of lifetime experienced traumas (assessed during SCID interviews). Discriminant validity for classifying CHR individuals who did and did not convert was demonstrated in a well-powered study (Cannon et al., Reference Cannon, Yu, Addington, Bearden, Cadenhead, Cornblatt and McGlashan2016) that was replicated in an independent sample (Carrión et al., Reference Carrión, Cornblatt, Burton, Tso, Auther, Adelsheim and Sale2016). NAPLS risk scores are provided for both 12- and 24-month probabilities for developing psychosis. The present study used the 24-month probability to maintain consistency with past longitudinal risk research in CHR populations (Cannon et al., Reference Cannon, Cadenhead, Cornblatt, Woods, Addington, Walker and McGlashan2008).
Statistical approach
Chi-square tests and independent t tests were employed to examine group differences in demographic variables (see Table 1). To test for group differences in early childhood social communication deficits between CHR and HC youth (Aim 1), we used independent t tests. Mann–Whitney U tests were employed to examine group differences for social communication variables that were highly skewed (i.e.,±2; see Table 2 for statistics). To examine the relationship between early childhood social communication deficits and symptoms and functioning in the CHR period (Aim 2), we used Pearson product-moment correlations. Because results did not differ between parametric and nonparametric tests, with the exception of reciprocal social interaction group differences, parametric results are presented. To examine the utility of early childhood social communication deficits in predicting psychosis risk (Aim 3), we used Pearson product-moment correlations to examine the association between early childhood social communication deficits and a validated psychosis risk index. Although the ultimate purpose of CHR research is to identify the small proportion of those who do transition to psychosis, and in several important ways these individuals could be considered extreme data points, we also wanted to determine the influence that a few extreme scores (± 3 SD) had on the associations between early childhood social communication deficits and risk for conversion. In addition, we also examined all other analyses with and without values ± 3 SD from the mean on any social communication variable in order to determine if outlier data points were driving findings. All analyses used two-tailed tests with α = 0.05. Cohen's d (Cohen, Reference Cohen1988) is provided for all group comparisons.
Table 2. Descriptive statistics for parent-reported developmental deficits and outcome variables
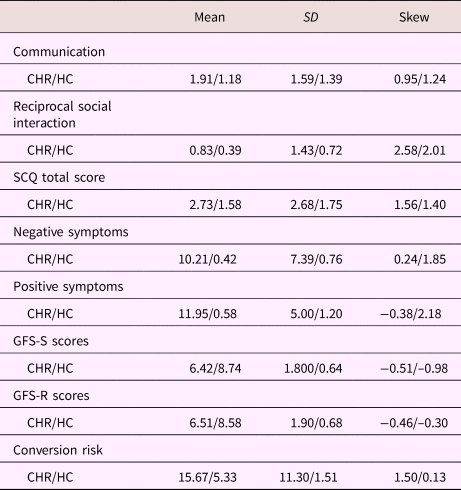
Note: CHR, clinical high-risk. HC, healthy control. SD, standard deviation. SCQ, Social Communication Questionnaire. GFS-S, Global Functioning Scale–Social. GFS-R, Global Functioning Scale–Role.
Table 3. Questions comprising the Social Communication Questionnaire Communication and Reciprocal Social Interaction Sum Scores specific to the 4- to 5-year age period

Results
There were no significant group differences observed for any of the demographic variables (see Table 1 for statistics). Descriptive statistics for early childhood social communication deficits and outcome variables are presented in Table 2. As detailed below, findings between early childhood social communication variables and psychosis risk were influenced by outliers. However, removal of outlier data points did not affect the results for any other analyses.
Group differences in early childhood social communication deficits
The first aim of the study was to determine if there were group differences in the number of total early childhood social communication deficits between CHR and HC youth, and then to examine if there were distinct deficits in the SCQ communication and reciprocal social interaction domains (see Figure 1). CHR participants had significantly more total early childhood social communication deficits than HC participants, t (79) = 2.26, p < .05, d = 0.56. Compared to HC participants, CHR participants also showed significantly more SCQ subdomain communication deficits, t (79) = 2.17, p < .05, d = 0.49. However, CHR participants did not exhibit more reciprocal social interaction deficits than HC participants, U = 695.00, p = .175, d = 0.44.

Figure 1. Group differences for the SCQ subdomains and the total SCQ sum scores. * = p < .05.
Early childhood social communication deficits, functioning, symptoms, and risk
Correlations between early childhood social communication variables and outcome measures are presented in Table 4. The second aim of the study was to examine associations between early childhood social communication deficits and social and role functioning within the CHR group and HCs. Higher total early childhood social communication deficits were negatively associated with both poorer GF-S (p < .01) and GF-R scores (p < .01). In addition, higher early childhood communication deficits were also associated with poorer GF-S (p < .05) and GF-R scores (p < .01). Finally, higher early childhood reciprocal social interaction deficits were also associated with poorer GF-S (p < .05) and GF-R scores (p < .01).
Table 4. Correlations between early childhood social communication sum scores and outcome variables

Note: GFS-S, Global Functioning Scale–Social. GFS-R, Global Functioning Scale–Role. SCQ, Social Communication Questionnaire. CHR, clinical high-risk. HC, healthy control. *p < .05. **p < .01. †p = .08.
The third aim of the study was to examine associations between early childhood social communication deficits, positive and negative symptoms, and the risk scores indexing probability for conversion to psychosis. Within the CHR group, higher total social communication deficits were significantly positively associated with increased negative symptom severity (p < .01), but not positive symptom severity (p = .60). Higher communication deficits were also significantly positively associated with increased negative symptom severity (p < .01) but not positive symptom severity (p = .42). There was a trend toward higher reciprocal social interaction deficits being significantly associated with more severe negative symptoms (p = .08), but not with positive symptoms (p = .91).
Higher total early childhood social communication deficits were significantly positively associated with greater probability for conversion to psychosis (p < .05; see Figure 2). Higher early childhood reciprocal social interaction deficits were also significantly positively associated with greater probability for conversion to psychosis (p < .05). There was no significant association between the SCQ communication domain subscore and risk for conversion (p = .14). Within the control group, there were no statistically significant associations between any of the early childhood social communication deficit variables and outcome measures.

Figure 2. Scatter plot representing the relationship between total parent-reported SCQ sum scores and probability of conversion risk scores.
Of note, as seen in Figure 2, the scatterplot indicates several outlier data points. When removing outlier cases on total and reciprocal social interaction variables (+ 3 SD; omitted 1 CHR and 1 HC participant), the associations with risk for conversion were no longer significant. However, it is notable that the direction and magnitude of the correlations (r of .23 for total and .26 for reciprocal social interaction) does still suggest a potentially important effect, and it will be necessary for future research to replicate and further examine this association.
Discussion
Investigating the nature of early childhood premorbid social communication deficits, and determining if they are associated with current functioning, symptom severity, and risk for conversion in CHR youth stands to inform the field's understanding of the etiology and progression of impairment and risk in psychosis. The present study suggests that social communication deficits are present during a critical period for social development (i.e., 4- to 5-year period) that overlaps with the premorbid stage of psychosis in CHR youth. Specifically, total early childhood social communication deficits were more prevalent in CHR youth than HC, and these deficits were associated with CHR youth's current level of social and role impairment, negative symptom severity, and risk for conversion. Furthermore, early childhood social communication deficits extended to the distinct communication subdomain (i.e., social initiation and interest, gesture, and imitation), with deficits being more frequent in CHR youth. Similar to total social communication deficits, distinct communication impairments were also associated with CHR youth's current social and role dysfunction and negative symptom severity. The expected impairment in CHR youth's early childhood reciprocal social interaction was not observed in the current study, and these behaviors may remain relatively more intact in the early premorbid period, at least in the present sample. These results are in line with extant research indicating that childhood premorbid deficits in social functioning are associated with illness risk (Liu et al., Reference Liu, Keshavan, Tronick and Seidman2015; Tarbox & Pogue-Geile, Reference Tarbox and Pogue-Geile2008), and extends these findings to early childhood social communication, supporting current neurodevelopmental models of schizophrenia.
Group differences in social communication
CHR youth exhibited more total and communication-specific social communication deficits in early childhood than HC youth. These findings are consistent with the broader literature in CHR and schizophrenia samples showing that social dysfunction is present throughout early premorbid development (Liu et al., Reference Liu, Keshavan, Tronick and Seidman2015; Tarbox & Pogue-Geile, Reference Tarbox and Pogue-Geile2008), and with findings indicating that patients with schizophrenia exhibit premorbid social communication deficits in early adolescence (Schiffman et al., Reference Schiffman, Walker, Ekstrom, Schulsinger, Sorensen and Mednick2004). In contrast to previous research in schizotypal personality disorder youth (Esterberg et al., Reference Esterberg, Trotman, Brasfield, Compton and Walker2008), expected group differences in reciprocal social interaction were not observed. Given that both social reciprocity and communication subdomain deficits are evident in CHR youth (Solomon et al., Reference Solomon, Olsen, Niendam, Ragland, Yoon, Minzenberg and Carter2011), lack of group differences in the reciprocal social interaction domain in the present study may be due to low endorsement of reciprocal social interaction deficits in the CHR sample (only 18 out 43 parents endorsed a deficit). It also may suggest potential phenotypic variation in reciprocal social interaction between schizotypal personality disorder and CHR populations. Consistent with this notion, it is also possible that reciprocal social interaction, as assessed by the SCQ, does not fully capture early deficits in social reciprocity in CHR youth. For example, many items on the SCQ ask if a child ever engages in a particular behavior during the 4- to 5-year age period, and thus may be less likely to capture potentially more subtle deficits in reciprocal social interaction such as reductions in social interest or emotional reciprocity rather than the absence of these behaviors. Furthermore, group differences in early childhood communication are consistent with findings in both CHR and schizophrenia samples showing impairments in verbal and nonverbal communication skills such as gesture and spontaneous imitation (Kohler et al., Reference Kohler, Martin, Stolar, Barrett, Verma, Brensinger and Gur2008; Mattes et al., Reference Mattes, Schneider, Heimann and Birbaumer1995; Vail et al., Reference Vail, Baltrušaitis, Pennant, Liebson, Baker and Morency2017; Walther et al., Reference Walther, Stegmayer, Sulzbacher, Vanbellingen, Müri, Strik and Bohlhalter2015).
Social communication and social and role functioning
Total and both communication- and reciprocal social interaction-specific early childhood social communication deficits were associated with CHR youth's current social and role functioning. These findings are consistent with research that has shown that early childhood social communication influences social functioning throughout adolescence and early adulthood (Darling-Churchill & Lippman, Reference Darling-Churchill and Lippman2016; McCabe & Altamura, Reference McCabe and Altamura2011; Mikami et al., Reference Mikami, Szwedo, Allen, Evans and Hare2010). The association between early childhood social communication and CHR youth's current social functioning in the present study suggests that examining specific social behaviors, such as social communication, that set the stage for social functioning in adolescence may be promising for elucidating social dysfunction throughout development in psychosis populations.
The current finding that early childhood social communication deficits were associated with CHR youth's current role functioning is also consistent with research showing that social competence in early childhood predicts academic and work achievement in adolescence and early adulthood (Caprara et al., Reference Caprara, Barbaranelli, Pastorelli, Bandura and Zimbardo2000; Collins & Van Dulmen, Reference Collins, Van Dulmen, Huston and Ripke2006; Masten et al., Reference Masten, Desjardins, McCormick, Sally, Kuo and Long2010). Furthermore, these findings are consistent with a recent meta-analysis demonstrating that social skills are a consistent predictor of role functioning outcomes in patients with schizophrenia (Tsang, Leung, Chung, Bell, & Cheung, Reference Tsang, Leung, Chung, Bell and Cheung2010). Evidence from retrospective studies examining premorbid social and academic functioning in schizophrenia populations suggest that individuals with childhood deficits in social functioning that persist or progress throughout adolescence and early adulthood also have similar trajectories for premorbid academic functioning (Allen, Frantom, Strauss, & van Kammen, Reference Allen, Frantom, Strauss and van Kammen2005; Monte, Goulding, & Compton, Reference Monte, Goulding and Compton2008; Strauss et al., Reference Strauss, Allen, Miski, Buchanan, Kirkpatrick and Carpenter2012). Given that social skills in early childhood are critical for establishing social and role functioning throughout development, similar parallel trajectories between social communication and social and role functioning may be present in psychosis populations.
Associations between early childhood reciprocal social interaction and CHR youth's current social and role functioning in the absence of group differences is important to consider. These findings are likely due to a subgroup within the CHR sample with early childhood reciprocal social interaction deficits whereas these behaviors are less impaired during early childhood in the larger sample. As mentioned earlier, only 18 out of 43 CHR youth exhibited reciprocal social interaction deficits in early childhood, and the number of deficits endorsed was relatively low (50% of the 18 only exhibited one deficit). In addition, 11 out of 38 HC youth exhibited reciprocal social interaction deficits in early childhood and 72% exhibited a single deficit. However, it is notable that the associations within the CHR sample did not change with outlier removal and group means were in the expected direction. Thus, it is possible that early childhood reciprocal social interaction deficits are less pronounced in CHR youth but still contribute additive impairment in social and role functioning in later developmental periods in a proportion of affected individuals. However, future studies will need to replicate and further examine these relationships.
The lack of associations between early childhood social communication and current social and role functioning in HC participants in the current study are surprising given robust evidence for similar relationships in typically developing children (Caprara et al., Reference Caprara, Barbaranelli, Pastorelli, Bandura and Zimbardo2000; Collins & Van Dulmen, Reference Collins, Van Dulmen, Huston and Ripke2006; Darling-Churchill & Lippman, Reference Darling-Churchill and Lippman2016; Masten et al., Reference Masten, Desjardins, McCormick, Sally, Kuo and Long2010; McCabe & Altamura, Reference McCabe and Altamura2011). This was most likely due to a restriction of range in social and role functioning measures in the current HC sample rather than evidence for specificity of associations in CHR youth. Specifically, means for GFS-S and GFS-R were high (8.74 and 8.58, respectively) and there was limited variability in the sample (0.64 SD for GFS-S and 0.68 for GFS-R).
Social communication, psychosis risk, and symptom severity
Early childhood total and reciprocal social interaction-specific social communication deficits were associated with an increased probability of converting to formal psychosis, as indexed by a well-validated risk calculator. These findings are consistent with research showing that premorbid social communication deficits in early adolescence differentiate children who develop schizophrenia from those who do not (Schiffman et al., Reference Schiffman, Walker, Ekstrom, Schulsinger, Sorensen and Mednick2004), as well as prospective longitudinal cohort studies indicating that childhood and adolescence premorbid socioemotional behaviors predict conversion to psychosis (Liu et al., Reference Liu, Keshavan, Tronick and Seidman2015). Moreover, this is consistent with evidence in individuals at CHR for psychosis showing premorbid social dysfunction differentiates converters from nonconverters (Cornblatt et al., Reference Cornblatt, Carrión, Addington, Seidman, Walker, Cannon and Tsuang2011; Dragt et al., Reference Dragt, Nieman, Veltman, Becker, van de Fliert, de Haan and Linszen2011; Velthorst et al., Reference Velthorst, Zinberg, Addington, Cadenhead, Cannon, Carrion and Mathalon2018), as well as predicts who is most likely to transition to psychosis (Cannon et al., Reference Cannon, Cadenhead, Cornblatt, Woods, Addington, Walker and McGlashan2008; Ruhrmann et al., Reference Ruhrmann, Schultze-Lutter, Salokangas, Heinimaa, Linszen, Dingemans and Heinz2010; Tarbox et al., Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013). However, a notable difference emerged between the current findings and premorbid prediction research in CHR youth. Specifically, early adolescent (12–15 age period) social dysfunction in CHR samples appears to be particularly predictive of transition to psychosis, whereas relationships between childhood (0–11 age period) social dysfunction and conversion have not been demonstrated (Dragt et al., Reference Dragt, Nieman, Veltman, Becker, van de Fliert, de Haan and Linszen2011; Tarbox et al., Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013).
Furthermore, associations between social dysfunction and conversion risk may be sexually dimorphic. For example, a recent study examined the relationship between early childhood (age 1–5 years) social dysfunction and the rate of conversion in a well-powered sample of CHR youth (Walder et al., Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013). Walder et al. (Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013) found that within males, current but not early childhood, social dysfunction predicted conversion to psychosis. In contrast, neither current nor early childhood social dysfunction was a significant predictor of conversion status within CHR females. Of note, findings from this study indicated that CHR males and females did not differ in severity of social dysfunction in early childhood. Taken together, previous findings suggest that relationships between social dysfunction and risk may develop in adolescence and confer greater risk for males than females at CHR for psychosis. Given social communication is in ascendance during early childhood and sets the stage for later social functioning (Darling-Churchill & Lippman, Reference Darling-Churchill and Lippman2016; McCabe & Altamura, Reference McCabe and Altamura2011; Mikami et al., Reference Mikami, Szwedo, Allen, Evans and Hare2010), differences between previous findings and the current findings suggest that examining specific early childhood social behaviors that underlie social functioning throughout development may aid in refining prediction in early childhood.
It is important to note that, although the direction and magnitude of the associations between early childhood total and reciprocal social interaction-specific social communication deficits and risk for conversion still suggest a potentially important effect, associations no longer reached conventional levels of significance after outlier removal. It is possible that these findings were driven by individuals at greatest risk for conversion. For example, extreme data points in early childhood social communication deficits may belong to the small portion of the sample who will convert to psychosis. Alternatively, it is also possible that the association between early childhood social communication deficits and risk for conversion is small and the current study was underpowered to detect this effect after outlier removal. Further research is needed to replicate these findings in larger samples, as well as using longitudinal designs that measure conversion status to test this possibility.
An association between early childhood social communication and CHR youth's current negative symptoms also emerged in the present study. Specifically, both higher total and communication-specific early childhood social communication deficits were associated with more severe current negative symptoms in CHR youth. In addition, there was a trend toward higher early childhood reciprocal social interaction deficits being associated with more severe negative symptoms in CHR youth. Negative symptoms of psychosis reflect a reduction or absence of normative behaviors and experiences and include deficits such as amotivation, asociality, and blunted verbal and nonverbal affect. These findings are largely consistent with extant research in CHR samples examining associations between premorbid adjustment and prodromal symptoms. For example, Tarbox et al. (Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013) found that social maladjustment in early adolescence was associated with CHR youth's current negative symptoms, including social anhedonia, amotivation, expression of emotion, and ideational richness. Moreover, it has been shown that CHR youth with poor premorbid adjustment in childhood that declines throughout development have more severe negative symptoms than those with better and more stable premorbid adjustment (Lyngberg et al., Reference Lyngberg, Buchy, Liu, Perkins, Woods and Addington2015). In addition, these findings are consistent with numerous studies indicating that declining premorbid social adjustment from childhood throughout adolescence is associated with more severe negative symptoms in first-episode and chronic psychosis populations (Addington & Addington, Reference Addington and Addington2005; Addington et al., Reference Addington, van Mastrigt and Addington2003; Chang et al., Reference Chang, Tang, Hui, Wong, Chan, Lee and Chen2013; Horton et al., Reference Horton, Tarbox, Olino and Haas2015; Larsen et al., Reference Larsen, Friis, Haahr, Johannessen, Melle, Opjordsmoen and McGlashan2004; Strauss et al., Reference Strauss, Allen, Miski, Buchanan, Kirkpatrick and Carpenter2012).
The lack of association between early childhood social communication and positive symptoms in the present study is largely consistent with studies of premorbid adjustment and symptoms in psychosis indicating that negative symptoms are more often associated with premorbid adjustment than positive symptoms (Chang et al., Reference Chang, Tang, Hui, Wong, Chan, Lee and Chen2013; Strous et al., Reference Strous, Alvir, Robinson, Gal, Sheitman, Chakos and Lieberman2004; Strauss et al., Reference Strauss, Allen, Miski, Buchanan, Kirkpatrick and Carpenter2012). Of note, associations between early adolescent social maladjustment and two positive symptom domains, suspiciousness and disorganized communication, have been observed (Tarbox et al., Reference Tarbox, Addington, Cadenhead, Cannon, Cornblatt, Perkins and Heinssen2013). The observed relationship between early childhood social communication deficits and symptom severity is intuitive given the overlap between early childhood social communicative behaviors and negative, but not positive, symptoms. For example, it is possible that social communication deficits in early childhood (such as poor nonverbal communication or social interest) and negative symptoms (such as blunted affect or asociality) may be the result of similar pathogenic processes that manifest differently across development, or manifestations of the same pathophysiological process that becomes more impaired across development.
Taken together, these findings suggest that social communication deficits present in early childhood may prove useful for informing our understanding of the pathophysiology of psychosis, social and role functioning in the prodromal period, and for improving prediction of those at greatest risk for conversion. In particular, the present research demonstrates that social communication deficits are present in CHR youth as early as the 4- to 5-year age period, a period earlier than has been shown in previous research.
Implications for neurodevelopmental models of psychosis
Consistent with neurodevelopmental models of psychosis (Pruessner et al., Reference Pruessner, Cullen, Aas and Walker2017; Walker et al., Reference Walker, Mittal and Tessner2008), the current findings suggest that early childhood social communication abnormalities are potentially early manifestations of an underlying liability for developing psychosis. Although the precise developmental trajectory between childhood premorbid social communication deficits and the emergence of prodromal syndromes is unknown, at least two possibilities exist. Early childhood social communication deficits, such as reductions in proactive social communication (e.g., range of emotions and interest in others), may be direct precursors to negative symptoms such as blunted affect or asociality. In addition, early childhood social communication deficits may reflect a developmental cascade (i.e., the cumulative process by which one domain of functioning affects or influences another domain of functioning throughout development; Masten & Cicchetti, Reference Masten and Cicchetti2010) wherein early social communicative behaviors directly contribute to functional outcomes and symptom severity in adolescence and early adulthood. For instance, nonverbal communication deficits (e.g., gesture) may contribute to peer rejection, thus resulting in social functioning deficits or negative symptoms, such as social isolation and withdrawal.
Such developmental cascades have been demonstrated in typically developing children. For example, Blair et al. (Reference Blair, Perry, O'brien, Calkins, Keane and Shanahan2015) demonstrated that in typically developing children, social skills at age 7 predicted friendship quality and peer acceptance at age 10. Furthermore, it has been shown that social competence (e.g., positive communication, social cognition, and prosocial relationships) at age 4 predicted internalizing behaviors, such as social withdrawal, at age 10 and 14 (Bornstein, Hahn, & Haynes, Reference Bornstein, Hahn and Haynes2010). It is possible that similar developmental cascades are present in CHR youth, and that social communication deficits present in early childhood contribute to the functional decline, symptom severity, and increased risk indicated in CHR youth.
Early identification and intervention: Importance and limitations
It is becoming evident that increased duration of untreated psychosis (i.e., time from first-episode until treatment) results in more severe symptomology, poorer functional outcomes, and less likelihood of symptom remission (Penttilä et al., Reference Penttilä, Jääskeläinen, Hirvonen, Isohanni and Miettunen2014). Even with treatment, full recovery rates are low (Robinson, Woerner, McMeniman, Mendelowitz, & Bilder, Reference Robinson, Woerner, McMeniman, Mendelowitz and Bilder2004) and relapse rates are high (Pelayo-Terán et al., Reference Pelayo-Terán, Galán, Martínez-García, Tabarés-Seisdedos, Crespo-Facorro and Ayesa-Arriola2017), leading many to emphasize early prevention aimed at delaying or preventing conversion (see Fusar-Poli, McGorry, & Kane, Reference Fusar-Poli, McGorry and Kane2017). Thus, early and accurate identification of individuals at greatest risk for developing a psychotic disorder is a critical priority. To date, early identification efforts have focused on prodromal risk markers, and do not typically include premorbid vulnerability markers in risk indices. The present findings suggest that the inclusion of premorbid factors, such as early childhood social communication deficits, have the potential to improve identification of those at high risk for conversion.
Moreover, intervention efforts to prevent conversion have also focused on the putative prodromal stage of the disorder. Although evidence suggests that early interventions in CHR populations reduced the risk for conversion by 50%, these effects diminished over a 2- to 4-year period (van der Gaag et al., Reference van der Gaag, Smit, Bechdolf, French, Linszen, Yung and Cuijpers2013), indicating more research is required to improve treatment outcomes. The presence of early childhood deficits, such as in social communication, provides initial evidence that identification, and thus intervention, may one day be possible before the prodromal stage. Interventions that specifically target social communication deficits may be particularly valuable given the importance of effective early childhood socialization for subsequent academic and social outcomes (McCabe & Altamura, Reference McCabe and Altamura2011). Given longitudinal evidence that the quality of early developmental childhood social interactions and peer experiences persists into adulthood, it is evident that early developmental social experiences lay the foundation for future peer relationships (Mikami et al., Reference Mikami, Szwedo, Allen, Evans and Hare2010). Social adversity (e.g., single-parent households and low socioeconomic status) is a key predictor for psychosis across the life span (Cantor-Graae, Reference Cantor-Graae2007; Heinz, Deserno, & Reininghaus, Reference Heinz, Deserno and Reininghaus2013), and interventions that may improve peer relationships could serve as a critical protective factor. Intervening to improve social communication early in childhood may thus improve social relationships throughout adolescence and into adulthood. Improved social functioning in turn may reduce risk for conversion and improve quality of life.
Limitations and future directions
The present findings are the first to suggest that early childhood social communication deficits are present in CHR youth. However, important limitations to the current study warrant discussion. First, the use of data obtained from retrospective reports from parents was a key limitation of this study. Retrospective reports are subject to errors in autobiographical memory and mood-congruent memory biases (Brewin, Andrews, & Gotlib, Reference Brewin, Andrews and Gotlib1993). Given that CHR youth in the current study exhibited current social impairments, parents’ reports of early childhood social communication deficits may have been unduly influenced by their child's current functioning. Moreover, evidence suggests that the agreement between retrospective and prospective reports varies widely across assessed domains (e.g., behavior problems, family conflict, and childhood trauma; Fisher et al., Reference Fisher, Craig, Fearon, Morgan, Dazzan, Lappin and McGuffin2009; Hassan, Reference Hassan2006; Henry, Moffitt, Caspi, Langley, & Silva, Reference Henry, Moffitt, Caspi, Langley and Silva1994), and may be particularly poor for psychological constructs that require specific events and dates (Henry et al., Reference Henry, Moffitt, Caspi, Langley and Silva1994). Thus, although the SCQ has been used extensively to obtain retrospective reports of childhood social communication deficits in a wide range of developmental and psychiatric populations (Granader et al., Reference Granader, Bender, Zemon, Rathi, Nass and MacAllister2010; Howlin & Karpf, Reference Howlin and Karpf2004; Magyar, Pandolfi, & Dill, Reference Magyar, Pandolfi and Dill2012; Mulligan, Richardson, Anney, & Gill, Reference Mulligan, Richardson, Anney and Gill2009; Pine, Guyer, Goldwin, Towbin, & Leibenluft, Reference Pine, Guyer, Goldwin, Towbin and Leibenluft2008; Snow & Lecavalier, Reference Snow and Lecavalier2008), including schizophrenia spectrum populations (Solomon et al., Reference Solomon, Olsen, Niendam, Ragland, Yoon, Minzenberg and Carter2011), the current findings should be viewed as preliminary and interpreted with caution. Taken together, future studies should examine the longitudinal relationship between early social communication deficits and later symptom severity and functioning to reduce the potential influence of retrospective bias. To better inform these resource-intensive longitudinal designs, further cross-sectional and retrospective research may be beneficial for understanding the specific relationships between different domains of social communication and distinct negative symptoms and social and role outcomes.
Second, although a questionnaire for premorbid social communication behaviors designed for psychosis populations would be ideal, the strategy of adapting a scale for examining childhood behaviors is a common practice the psychosis field employs when schizophrenia-specific, validated scales are unavailable. We used an autism scale because the items overlapped well with behaviors well evidenced to be impaired across the schizophrenia spectrum. We excluded the single participant with autism spectrum disorder, and thus do not believe that autism drove the findings. Furthermore, given that the communication and reciprocal social interaction subdomain scores were highly correlated with the total SCQ score (r = .90 and r = .83, respectively), and the relatively small sample size in the current study, we were unable to examine the unique effects of the two subdomain scores and the total scale, above and beyond the others. High intercorrelations between the total SCQ score and subdomain scores are inherent to the SCQ as a measure (see Rutter et al., Reference Rutter, Bailey and Lord2003), and as previously mentioned, development of a more sensitive measure specific to social communication deficits in psychosis may be beneficial for elucidating unique effects of distinct social behaviors in schizophrenia spectrum populations. Thus, although the current study provides initial evidence that distinct early childhood social behaviors are associated with illness features in CHR populations, future research with larger sample sizes will be needed to better understand the specificity of the observed associations between the social communication subdomains and the outcome measures in the current study.
Furthermore, as mentioned above, the use of more well-powered studies would allow for testing the unique relationships between specific domains of social communication, symptom severity, social and role functioning, and psychosis risk. In addition, larger sample sizes would also afford an examination of potential subgroups within CHR youth. For example, comparing those with a high number of social communication deficits in the communication and/or reciprocal social interaction domains to those with a low number or no deficits. Moreover, given that evidence suggests there may be sex-specific associations between early childhood social dysfunction and CHR youth's current symptoms and functional outcomes (Walder et al., Reference Walder, Holtzman, Addington, Cadenhead, Tsuang, Cornblatt and Perkins2013), larger samples would allow for an exploration of potential distinct associations within male and female CHR youth's social communication behaviors and outcomes. Finally, the present study used psychosis risk scores as a proxy for possible conversion to formal psychosis. Although the risk calculator has been validated and replicated in well-powered samples (Cannon et al., Reference Cannon, Yu, Addington, Bearden, Cadenhead, Cornblatt and McGlashan2016; Carrion et al., Reference Carrión, Cornblatt, Burton, Tso, Auther, Adelsheim and Sale2016), further longitudinal research is needed to test whether early social communication deficits predict conversion. Thus, although the current findings provide initial evidence for the potential benefit of examining the relationship(s) between early childhood premorbid social behaviors and psychosis risk, they should be interpreted as preliminary.
Conclusion
The present research showed that individuals at CHR for psychosis demonstrated social communication deficits in early childhood. Furthermore, early childhood social communication deficits were associated with increased negative symptom severity and worse social and role functioning during the CHR period. Finally, early childhood social communication deficits were associated with increased risk for psychosis. These findings are consistent with neurodevelopmental models of psychosis, which suggest that underlying liability for developing psychosis manifests in behavioral deficits in early childhood. Furthermore, they provide initial evidence that the inclusion of early childhood risk markers, such as social communication deficits, may inform our understanding of the prodromal period and improve prediction of those at greatest risk for conversion.
Financial support
This work was supported by National Institutes of Health Grant R01MH094650 and R21/R33MH103231 (to V.A.M.).








