Published online by Cambridge University Press: 21 January 2005
Objectives: We sought to determine trends, and outcomes, for a cohort of patients with pulmonary atresia with intact ventricular septum born between 1965 and 1998. Background: Pulmonary atresia with intact ventricular septum is a complex lesion that remains a therapeutic challenge, particularly regarding the suitability for biventricular repair. Methods: We identified 210 consecutive patients, and reviewed their medical records, initial angiograms, and echocardiograms, along with the relevant surgical and pathology reports. Results: The mean initial Z-score for the diameter of the tricuspid valve was −0.99 ± 1.95, with Ebstein's malformation in 8%. A right ventricular dependent coronary arterial circulation was found in 23%. The proportion of patients who received treatment increased over time, although placement of an arterial shunt was the predominant initial procedure throughout the experience. At the last follow-up, 107 patients had not reached the planned final stage of their repair, and 79% of these had died. Of the 103 reaching the final stage of planned repair, 58 had undergone attempted biventricular repair, with 34% dying; 14 had undergone attempted one and a half ventricular repair, with 7% dying, and 31 had undergone attempted functionally univentricular repair, with 10% dying. Overall, survival was 57% at the age of 1 year, 48% at 5 years, and 43% at 10 years. Survival improved over time, with survival of 75% at 1 year, and 67% at 5 years, for patients born between 1992 and 1998. An earlier date of birth, the presence of Ebstein's malformation, and prematurity were all significant independent factors associated with decreased survival. A greater severity of coronary arterial abnormalities was significantly associated with a greater likelihood of left ventricular dysfunction during follow-up. Conclusions: The outcomes for patients born with pulmonary atresia with intact ventricular septum have improved over time, albeit that careful initial management, and better selection, is still indicated for those planned to undergo biventricular repair.
Pulmonary atresia with intact ventricular septum is an uncommon and extremely heterogeneous congenital cardiac anomaly.1 Even nowadays, survival after surgical intervention is poor2–4 albeit that several recent studies have reported improved survival5–7 in selected subsets of patients. As the outcomes for the entire spectrum of patients were not presented in these selected series, the reported survival may be biased. Selection of the initial intervention has an important impact on the suitability for subsequent procedures, and the eventual outcomes.3, 5, 7–11 There is, nonetheless, a wide range of reported algorithms for management.3–5, 7–9, 11–20 Emerging from these experiences is the recognition that right ventricular dependent coronary arterial circulation is an important factor determining the initial management, with right ventricular decompression being contraindicated. As the strategies for management become more advanced, it is possible to neutralize the impact on survival of risk factors such as tricuspid valvar size and characteristics, the ratio of the diameter of the tricuspid to the mitral valve, the ratio of right to left ventricular systolic pressure, and the right ventricular dependent coronary arterial circulation.2, 8, 21–23 Such improvement, however, has not been noted in more recent studies that focused on the need to demonstrate improved survival.5 Furthermore, previous studies based on outcomes have not documented changing trends in management and outcome. We sought to address all these problems by analyzing the management and outcomes for a large cohort of patients seen in a single institution, seeking to determine the factors underscoring outcomes, particularly time-related mortality.
From the Cardiology and Cardiovascular Surgery Databases of the Hospital for Sick Children, Toronto, we identified 210 patients with pulmonary atresia with intact ventricular septum as having been assessed from January 1965 to December 1998. Diagnoses were verified by reviewing medical records, angiograms, echocardiograms, surgical reports, and pathology reports. All consecutive patients with pulmonary atresia with intact ventricular septum were reviewed, including those with associated Ebstein's malformation of the tricuspid valve, and a ventricular septal defect if of no haemodynamic significance. Patients with either discordant atrioventricular and/or ventriculoarterial connections were excluded, as were patients with other major associated cardiovascular anomalies.
The initial Z-score for the diameter of the tricuspid valve was calculated from the nomograms assembled by Rowlatt et al.24 Echocardiograms were not available for the majority of the period, and thus we aborted the use of echo-based nomograms.25 Right ventricular morphology was classified according to the tripartite, bipartite, or unipartite nature of the ventricular cavity as reported by Bull et al.26 The concept acknowledges that the inlet, apical trabecular, and outlet ventricular components are always present in this condition, but that variable mural hypertrophy obliterates parts of the ventricular cavity, particularly the apical trabecular and outlet components.27 The presence of right ventricular coronary arterial sinusoids, right ventricular to coronary arterial fistulous communications, and right ventricular dependent coronary arterial circulation were all identified if present.28, 29 As assessed from right ventricular angiograms, we defined sinusoids as intramyocardial vascular spaces continuous with the ventricular lumen, but without any communication with the epicardial coronary arteries. Fistulous communications were considered present if there was angiographic evidence of communications between the intramyocardial vascular spaces and the epicardial coronary arteries. When intrinsic lesions of the epicardial coronary arteries were observed, such as stenosis, atresia or absence of connection to the aorta, and these lesions were proximal to a fistulous connection between that coronary artery and the right ventricle, then the distal coronary arterial flow was presumed to be partially or completely dependent on the right ventricle. Assessment of dynamic obstruction of the left ventricular outflow tract from leftward bulging of the ventricular septum was assessed by review of angiograms and echocardiograms. This was graded subjectively as no bulging of the septum into left ventricular outflow tract, a mild bulge, or a moderate bulge.
Patients were classified as being in their final end-states if they had undergone attempted biventricular, one and a half ventricular, or functionally univentricular repair. Patients who had not achieved one of these three defined end-states at the time of their last follow-up were classified as being in an intermediate stage.
Initial angiograms were reviewed to determine the size of the tricuspid valve, the diameter of the proximal right and left pulmonary arteries, and the morphology of the right ventricle, and to seek the presence of right ventricular sinusoids, fistulous communications, and Ebstein's malformation of the tricuspid valve. Angiographic review of the proximal and distal coronary arteries was performed to determine the presence or absence of arterial irregularities, stenoses, or interruption. For patients born in the more recent years, pre-intervention echocardiograms were reviewed to obtain the size of the tricuspid valvar annulus and the proximal right and left pulmonary arteries. The ventricular septum was reviewed to detect the presence of any leftward bulging, which was graded as absent, mild, or moderate as described above.
Data are described as frequencies, medians with ranges, and mean values with standard deviations as appropriate. Where there is missing data, the values are given for the number of patients with available data. All analyses were performed using SAS Version 6.12 statistical software (SAS Institute, Inc., Cary, North Carolina) with default settings. A p-value of less than 0.05 was set as the level of statistical significance. Trends over consecutive birth cohorts were sought with Mantel–Haentsel χ2 and Kruskal–Wallis ANOVA. Overall survival was estimated using the Kaplan–Meier method. Factors associated with overall mortality were sought by parametric modelling of time-related death in the hazard domain as described by Blackstone et al.30
In the period from January 1965 to December 1998, we identified 210 consecutive patients, 49% of whom were male, as presenting with pulmonary atresia and an intact ventricular septum. Of these patients, 182 patients (87%) were born at term, while 28 were born prematurely at less than 37 weeks gestation. There were six patients who were products of twin gestations. The “other” twin was normal for five of these patients, whilst in the final patient, the twin had died in-utero at 28 weeks gestation. Weight at birth was available for 197 newborns, with the mean weight being 3.13 ± 0.69 kg. An antenatal diagnosis had been made in 8 patients (4%), with 171 (81%) diagnosed on the first day of life. Almost all patients (94%) had been diagnosed within 6 days of birth. At presentation, cyanosis was noted in 208 patients (98%), with associated respiratory distress in 25 (12%).
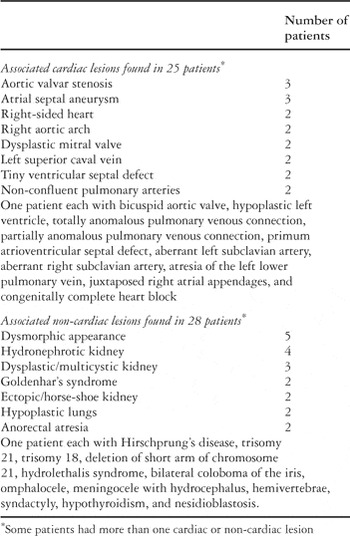
Ebstein's malformation of the tricuspid valve was noted in 16 patients (8%). Other associated cardiac lesions were identified in 25 patients (12%), with extracardiac lesions or syndromes seen in 28 patients (13%, Table 1).
Table 1. Associated cardiac and non-cardiac lesions.
Initial data from cardiac catheterization was available for 198 patients (94%), although angiograms were available for review in only 169 patients (81%). Right ventricular systolic pressures had been measured in 171 cases, with the median right ventricular pressure being 110 mmHg, with a range from 15 to 188 mm. Data relating to left ventricular or systemic arterial systolic pressure was available for 172 patients, with a median pressure of 70 mmHg, with a range from 42 to 120 mm. The median right ventricular to systemic pressure ratio was 0.53 as calculated for 170 patients, with a range from 0.28 to 3.07. We were able to measure accurately the diameter of the tricuspid valve from the angiograms of 137 patients, and the median value was 9.2 mm, with the range from 4 to 33 mm. The median Z-score for these values was −1.25, with a range from −5 to 2. Right pulmonary arterial diameter was available in 129 patients, with the median being 4.9 mm, with a range from 3 to 7.5 mm. The comparable diameter of the left pulmonary artery was available for 127 patients, with a median diameter of 4.7 mm, with a range from 3 to 7.2 mm. Right ventricular morphology could be assessed in 183 patients, being tripartite in 152 patients (83%), bipartite in 27 (15%), and unipartite in only 4 patients (2%). The right ventricular infundibulum was identified in 176 patients, being well developed in 69 patients (39%), narrowed in 75 (43%), and atretic in 32 (18%). We were able to assess the extent of septal bulging in 155 angiograms, finding no septal bulge in 103 (67%), mild bulging in 41 (26%), and moderate bulging in 11 patients (7%). In 7 patients (3%), the right ventricle was dilated with poor systolic function. Of these patients, 4 died prior to any palliative procedure, 2 being found to have Ebstein's malformation. All of these patients had “wall-to-wall” hearts as seen on the chest radiogram.
The information regarding right ventricular sinusoids was available in 182 patients, and sinusoids were seen in 125 (69%) (Table 2). Fistulous communications could be assessed in 180 patients, being seen in 100 (55%). In 95 of these, it proved possible to identify the location of the fistulas, which were confined to the left coronary artery in 13 patients (14%), to the right coronary artery in 5 (5%), but involved both coronary arteries in 77 patients (81%). Detailed analysis of coronary arterial anatomy was possible in 172 patients. Normal coronary arteries were seen in 118 of these patients (69%). Proximal stenoses were found in 20 (12%), dilated arteries in 4 (2%), and proximal interruption in 29 patients (17%). In 39 patients (23%), we identified a right ventricular dependent coronary arterial circulation.
Table 2. Associated coronary arterial anomalies.

When grading the severity of the coronary arterial anomalies on an ascending scale, from no obvious anomalies through the presence of sinusoids only, fistulous communications without stenoses, those with associated stenoses, absence of connection to the aorta with proximal or distal arterial interruption, and finally associated large coronary cameral fistulas, we found that an increasing grade of coronary arterial abnormalities was significantly associated with a greater likelihood of uni- or bipartite right ventricular morphology (p = 0.001), a greater likelihood of muscular infundibular stenosis or atresia (p = 0.001), a greater likelihood of obstruction within the left ventricular outflow tract (p = 0.034), a lower Z-score for the tricuspid valve (p < 0.001), a higher ratio of right to left ventricular systolic pressure (p < 0.001), and a greater likelihood of left ventricular dysfunction noted at follow-up (p = 0.042).
Pre-intervention echocardiograms were reviewed in 76 patients (36%) to measure the diameters of the tricuspid valve and the proximal right and left pulmonary arteries. The tricuspid valvar diameter was measured in 67 patients, with the median value being 7.3 mm, with a range from 3.2 to 21, and with a median tricuspid valvar Z-score of −2.4, with a range from −5.3 to +2. Then median diameter of the left pulmonary artery was 4.35 mm, with a range from 2 to 6.3 mm, and the right pulmonary artery measured 4.30 mm, with a range from 2 to 7.8 mm. Systolic bulging of the septum into the left ventricular outflow tract, with the potential to produce obstruction, was absent in 41 patients (55%), mild in 34 (44%), and moderate in 1 patient.
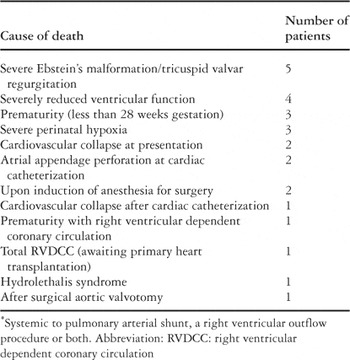
We have used infusions of prostaglandin E2 prior to surgical or catheter intervention since 1976. Death before any intervention, such as construction of an arterial shunt, or reconstruction of the right ventricular outflow tract, occurred in 26 patients (12%). The causes for death are shown in Table 3. Among 184 patients treated surgically, 83 patients died, while 101 patients were alive at the latest follow-up at a median age of 6.2 years, with a range from 13 days to 23.8 years. Initial balloon atrial septostomy had been performed in 124 patients (59%). A systemic to pulmonary arterial shunt was initially placed in 96 patients (52%), 49 of whom (51%) subsequently died. Placement of a shunt together with reconstruction of the right ventricular outflow tract was initially performed in 45 patients (25%), 18 of whom (40%) subsequently died. A surgical procedure to enlarge the right ventricular outflow tract in isolation was initially performed in 24 patients (13%), 13 of whom (54%) subsequently died. Transcatheter radio frequency assisted perforation of the atretic pulmonary valve followed by balloon dilatation was initially attempted in 17 patients seen recently (9%), 3 of whom (17%) died subsequently. A cavopulmonary connection, together with an atrial septectomy, was performed in 1 patient who presented for the first time at 17 months of age with severe cyanosis. Another patient who presented at 23 months of age underwent a cavopulmonary connection along with reconstruction of the right ventricular outflow tract as the initial procedure. Both of these patients were alive at latest follow-up.
Table 3. Reasons for death before any intervention (26 patients)*.
Of the 96 patients who had placement of a shunt as the sole initial procedure, 15 died without any other subsequent intervention. Subsequent procedures included placement of a second shunt, or revision of the original shunt, in 20 patients, with 3 patients having a third shunt or revision. Obliteration of the cavity of the right ventricle with closure of the tricuspid valve was performed as an intermediate procedure in 14 patients, with reconstruction of the right ventricular outflow tract performed in 16 patients, and a cavopulmonary connection constructed in 11 patients.
At the time of latest follow-up of the initial 96 patients, 40 had died without having achieved an end-state, and there were 16 survivors in various intermediate states. There were 28 patients who had achieved the final end-state of functionally univentricular repair, 2 of whom had subsequently died. Biventricular repair was attempted in 8 patients, with 6 deaths, and 4 patients were submitted to a one and a half ventricular repair, with 1 death.
Of the 45 patients who initially underwent a combination of placement of a shunt and attempted enlargement of the right ventricular outflow tract, 16 died without any subsequent procedures. Biventricular repair was performed in 18 patients, with 2 subsequent deaths. One and a half ventricular repair was performed in 6 patients, with no deaths. The remaining 5 patients were alive at last follow-up, albeit awaiting their final treatment.
Reconstruction of the right ventricular outflow tract as the sole procedure was performed in 24 patients. A shunt was then placed subsequently in 5 patients, with 1 patient having a second shunt, with 1 of these patients dying. In 17 patients, the right ventricular outflow tract was opened by transcatheter radio frequency assisted perforation, followed by balloon dilatation of the atretic pulmonary valve. The attempt failed in 2 patients, with 1 subsequent hospital death. Of the 15 where the procedure was successful, a shunt was required subsequently before discharge from hospital in 11 patients. Infective endocarditis occurred in 1 patient, who subsequently died after surgical removal of vegetations and reconstruction of the right ventricular outflow tract.
Overall, at latest follow-up, 3 patients had died whilst awaiting definitive treatment. Of the remaining patients, biventricular repair had been attempted in 32 patients, with 12 deaths, a one and a half ventricular repair had been performed in 4 patients, with no deaths, and 3 patients had undergone functionally univentricular repair, with 1 death.
Death occurred in 26 patients before any intervention was performed, with support being withdrawn in some. A total of 103 patients have had their definitive procedure. Of these, biventricular repair had been attempted in 58 patients, with 20 (34%) deaths. Univentricular palliation was achieved in 31 patients, with 3 patients dying (10%), and one and a half ventricular repair had been performed in 14 patients, with 1 death (7%). The remaining 107 patients had non-definitive procedures and have not yet achieved the planned definitive option, albeit that 59 patients have died (55%).
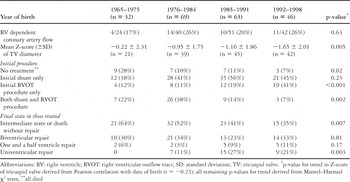
In order to determine trends over time, we divided our cohort into four groups according to their date of birth. Thus, 32 patients had been born from 1965 to 1975, 69 from 1976 to 1984, 63 from 1985 to 1991, and 46 between 1992 and 1998. Table 4 shows trends in anatomy, management, and outcomes. The proportion of patients who received treatment significantly increased over time. There was no significant change in anatomic characteristics, although there was some suggestion of a trend towards greater tricuspid valvar hypoplasia. This was further evident when date of birth was related to the tricuspid valvar Z-score, with a Pearson correlation coefficient of r — 0.20 (p = 0.02). Placement of an arterial shunt was the predominant initial procedure across the cohorts. In the earlier three cohorts, this was sometimes accompanied by surgical enlargement of the right ventricular outflow tract, but in the most recent cohort, this was replaced by transcatheter radio frequency assisted perforation of the atretic pulmonary valve with balloon dilatation, many of these patients subsequently needing placement of an arterial shunt.
Table 4. Trends with consecutive birth cohorts.
Time-related survival after birth as calculated with the Kaplan–Meier method gave estimates of survival of 72% at 1 month, 57% at 1 year, and 50% at 5 years up to 23.8 years (Fig. 1). To determine incremental risk factors for time-related survival, we developed a parametric multivariable model with a single early hazard phase using the methods of Blackstone et al.30 Significant independent factors for mortality included an earlier date of birth, presence of Ebstein’s malformation, and prematurity (Table 5). After controlling for these factors, no other factor was significantly associated with time-related mortality, including the severity of coronary arterial anomalies, right ventricular characteristics, and tricuspid valvar Z-score. Predictions of time-related survival from birth for the consecutive birth cohorts for patients without Ebstein’s malformation or prematurity are shown in Figure 2.
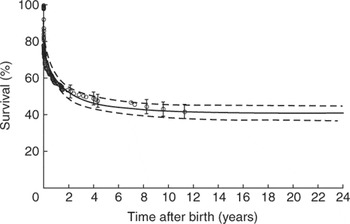
Figure 1. Survival from birth.
Table 5. Incremental risk factors for time-related mortality since birth.
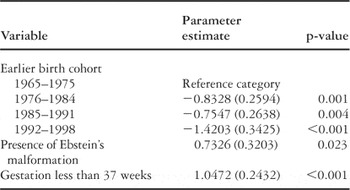
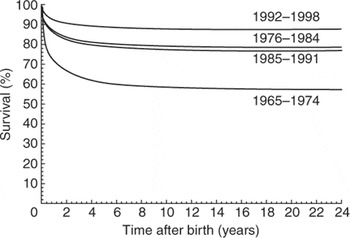
Figure 2. Survival from birth stratified by consecutive birth cohort.
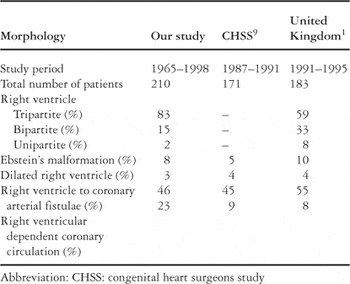
Our study, to the best of our knowledge, is the largest series of cases reported from a single institution, in terms of numbers being comparable only to the population-based morphologic study from the United Kingdom.1 Thus, in our study, based on all patients admitted to the hospital over the selected time frame, we have been able to analyse the overall management, outcomes, trends, and risk factors for a large cohort of patients with pulmonary atresia and intact ventricular septum. Daubeney and colleagues,1 in their population-based study, were able to analyze the range of morphology seen in patients with this heterogeneous lesion. There are certain morphological similarities, as well as differences, between these two and another large study,9 as shown in Table 6. These differences could reflect factors such as patterns of referral, the effect of antenatal diagnosis and termination of pregnancy, as well as difficulties and variability in qualifying the morphological details.
Table 6. Morphological comparison between our series, the CHSS study, and the United Kingdom study.
Improved understanding of the anatomy and the management of these patients have led to improving outcomes. The introduction of intravenous infusion of prostaglandin31 in 1976 contributed to improved neonatal survival and preoperative stabilization. Historically, the surgical palliation began with development of systemic-to-pulmonary arterial shunts, followed by open and closed pulmonary valvotomy, reconstruction of the right ventricular outflow tract with a transjunctional patch, use of cavopulmonary connections and the Fontan procedure, transcatheter pulmonary valvar perforation and balloon valvotomy, and the one and a half ventricular repair.3, 4, 9, 11, 14, 16–18, 20, 32–35 The recognition of the disordered coronary arterial circulation, particularly the concept of a right ventricular dependent coronary arterial circulation, and its adverse impact on ventricular function, has led to this being an important consideration in selecting optimal strategies for management. The concept of right ventricular overhaul has been reported to benefit some of these patients.35 In neonates with severe tricuspid valvar dysplasia and regurgitation, with severe cardiomegaly, the outlook is still poor, despite the development of an approach involving surgical creation of tricuspid atresia.36 The so-called “wall to wall” heart as seen on the chest radiograph, even though seen in a small number of patients, is due to gross dilatation of the right atrium, often with concomitant dilatation of the poorly functioning right ventricle, and carries a very high risk of death, even prior to any intervention.
Transcatheter interventions have recently been incorporated into the algorithms for management, with perforation and balloon dilatation of the atretic pulmonary valve used as an initial alternative for right ventricular decompression.20 In earlier years, balloon atrial septostomy was performed in the majority of patients.12 Currently, this would be reserved for those patients with severely hypoplastic right ventricles, with or without a right ventricular dependent coronary arterial circulation, who are deemed to be on the functionally univentricular pathway.20 Decompression of the right ventricle is now known to be best avoided in such patients.3, 5, 6, 9, 11, 15–22 Use of the one and a half ventricular repair has helped avoid the early mortality that can follow an attempted biventricular repair in borderline cases, and similarly avoids the late morbidity and mortality of functionally univentricular palliation.32 Recognition of morphological and physiological aspects has directed management, and impacted on outcomes, particularly for patients with severe or complex anatomy.5,7,10,15–18
Our series is unique in that we have defined the outcomes of all the patients admitted to our institution, not just the initial intervention. Some patients may die prior to an intervention, or are deemed inoperable. This is a portion of the overall mortality that may, in future, be ameliorated by improved antenatal services and counselling.37 Elective termination of pregnancy has resulted in a decrease in the live-born incidence of this lesion.38 Prenatal counselling, however, must be based on both evolving and current trends in recognizing risk factors and their impact on management and outcome. At our institution, we increasingly favour the functionally univentricular and the one and a half ventricular approaches to repair, and have noted an increase in the number of patients who are offered treatment. Further improvement in outcomes is likely to be achieved by more stringent selection of the patients deemed feasible for biventricular repair, as we lost one-third of our patients put forward for this type of repair.
The one and a half ventricular repair provides relief of the obstruction in the right ventricular outflow tract, as well as partially unloading the right heart by the cavopulmonary anastomosis. We report a low mortality with this approach, below that occurring following attempted functionally univentricular repair, and appreciably lower than the mortality of biventricular repair. While long-term outcomes have yet to be defined, the intermediate-term outcome of the one and a half ventricular strategy appears to be encouraging.32
There is a great deal of variability in the coronary arterial circulation of the patients, which is correlated with the severity of right ventricular hypoplasia.9, 12, 15, 22, 23 We found coronary arterial anomalies in about one-third of our patients, a proportion comparable to previously published reports,1, 8, 15, 21 with right ventricular dependent coronary arterial circulation found in almost one-quarter, again comparable to the previously published case series,15 but a higher proportion when compared to the population-based study.1 In the presence of severe proximal coronary arterial stenoses or complete luminal interruption, the flow of blood to the distal coronary arterial circulation depends on flow from the right ventricle. In this setting, it is now accepted that surgical obliteration of the right ventricle, closure of the tricuspid valve, or decompression of the right ventricle must be avoided to prevent catastrophic myocardial infarction.3, 6, 8, 11 While it has been suggested that lesions involving only one coronary artery may not contraindicate right ventricular decompression,22 caution should be exercised before attempting biventricular repair in this setting. We found that higher grades of coronary arterial abnormalities are significantly associated with greater hypoplasia of the right heart, and a greater likelihood of subsequent left ventricular dysfunction. Given its importance, it is essential to make a careful and complete delineation of the coronary arterial circulation before making any decisions about management.5, 22
Adoption of the functionally univentricular repair has improved considerably the survival of those who have a right ventricular dependent coronary arterial circulation.5–7, 9, 10, 17, 18, 22, 34 Although the immediate mortality is reduced for such patients, they remain susceptible to long-term complications peculiar to the functionally univentricular palliation, as well as those that may result from the disordered coronary arterial circulation. Progressive left ventricular dysfunction, and dynamic obstruction of the left ventricular outflow tract, raise the possibility of ventricular dysrhythmias and sudden death.39, 40 Cardiac transplantation may become inevitable for such patients, particularly as improved results and survival make it an acceptable treatment option for patients with end-stage heart failure secondary to complex congenital cardiac disease.5
Hanley et al.9 reported data from a series of 171 neonates entered into a prospective multi-institutional study. Survival after the first intervention was 81% at 1 month, and 64% at 4 years. The incremental risk factors for death after entry were a lower weight at birth, smaller dimensions of the tricuspid valve, and a right ventricular dependent coronary arterial circulation. Only 8 patients in this series had severe right ventricular enlargement, and the outcome for these patients was unfavourable.
Rychik et al.10 reviewed 67 patients, and reported overall survival at 1, 5, and 8 years of 82%, 76%, and 76% respectively, with a strategy for treatment that incorporated an aortopulmonary shunt alone in 31 patients, right ventricular recruitment in 32, and cardiac transplantation in 4 patients. Mortality was highest in infancy, but was equivalent for all three strategies. While there was no significant difference in the Z-score for the tricuspid valve amongst survivors as opposed to non-survivors, those patients surviving a biventricular repair had a significantly higher score when compared to those who had been submitted to the Fontan operation.
Jahangiri et al.5 reported an overall survival of 98%, and Laks and Plunkett6 have reported early survival of 90% and late survival of 87%. While these reported contemporary results are excellent, they are each based on selected subgroups of patients. Our much lower overall survival relates to all patients presenting to our Institution with pulmonary atresia and intact ventricular septum over a much longer period of time. The improved survival noted in our most recent birth cohort, nonetheless, is comparable to the selective studies.
Patients with pulmonary atresia and intact ventricular septum continue to present complex problems in management, primarily related to the broad anatomic spectrum of abnormalities afflicting the right ventricle, and the coronary arterial involvement. Outcomes have improved considerably, as has the scope for treatment. Further improvement in overall survival may result from development of strategies addressing the two independent factors identified in our study associated with decreased survival, namely Ebstein's malformation of the tricuspid valve and prematurity. Identification of predictors of developmental and functional capacity of survivors in each of the different end-states will contribute to improving the long-term outcome and quality of life for these patients.
We acknowledge the assistance of Cameron Slorach in reviewing the echocardiograms.

Table 1.

Table 2.

Table 3.

Table 4.

Survival from birth.

Table 5.

Survival from birth stratified by consecutive birth cohort.

Table 6.