Introduction
Adaptive behavior refers to the performance of daily activities necessary for personal and social sufficiency at an age-appropriate level (Harrison & Oakland, Reference Harrison and Oakland2003; Sparrow, Cicchetti, & Balla, Reference Sparrow, Cicchetti and Balla2005), and has been associated with long-term outcomes such as employment and residential independence (Woolf, Woolf, & Oakland, Reference Woolf, Woolf and Oakland2010). It requires the integration of cognitive, emotional, and behavioral abilities into coherent behavior that is able to meet the variable demands of different environments and situations. Perhaps because of the importance of adaptive behavior/functioning in the diagnostic criteria for intellectual disability (formerly mental retardation), the majority of studies involving adaptive functioning include IQ as a central variable of interest (e.g., Carpentieri & Morgan, Reference Carpentieri and Morgan1996; Liss et al., Reference Liss, Harel, Fein, Allen, Dunn, Feinstein and Rapin2001; Poggi et al., Reference Poggi, Liscio, Galbiati, Adduci, Massimino, Gandola and Castelli2005; Schatz & Hamdan-Allen, Reference Schatz and Hamdan-Allen1995). Although scores on measures of adaptive and intellectual functioning are thought to be closely linked, correlation coefficients vary widely (ranging from .03 to .91), with the majority of correlations in the moderate range (Harrison, Reference Harrison1987). Barkley and colleagues have advocated for the idea of adaptive disability as a construct in which other behavioral factors (e.g., conduct problems, inattention, aggression) are associated with adaptive dysfunction in the context of broadly intact intelligence (Barkley et al., Reference Barkley, Shelton, Crosswait, Moorehouse, Fletcher, Barrett and Metevia2002; Shelton et al., Reference Shelton, Barkley, Crosswait, Moorehouse, Fletcher, Barrett and Metevia1998).
This trend toward investigation into additional variables, over and above intelligence, which might contribute to adaptive impairment is ongoing and could have implications for both diagnosis and treatment planning. These emerging lines of inquiry have been particularly fruitful when focused upon a variety of distinct behavioral, developmental, and medical conditions (e.g., Barkley, Fischer, Smallish, & Fletcher, Reference Barkley, Fischer, Smallish and Fletcher2006; Liss et al., Reference Liss, Harel, Fein, Allen, Dunn, Feinstein and Rapin2001; Papazoglou, King, Morris, & Krawiecki, Reference Papazoglou, King, Morris and Krawiecki2008). Several variables thought to increase the adaptive burden upon these youth have been identified, including executive dysfunction, disruptive/interfering behaviors, and internalizing/affective conditions. This is consistent with DSM-IV criteria (Diagnostic and Statistical Manual, Fourth Edition, American Psychiatric Association, 2000), which currently requires evidence of functional impairment (social, occupational, academic, or other important areas) for many diagnoses including behavioral (e.g., ADHD, disruptive behavior disorder) and mood disorders, although, unlike criteria for intellectual disability/mental retardation, there is no specified method for quantifying this functional impairment.
In children with epilepsy, executive functioning skills appear to be closely linked to adaptive functioning (Culhane-Shelburne, Chapieski, Hiscock, & Glaze, Reference Culhane-Shelburne, Chapieski, Hiscock and Glaze2002). Similarly, parent-report of metacognitive skills in children with myelomeningocele and hydrocephalus is strongly correlated with parent report of self-care skills (Jacobson, Tarazi, Levy, Mahone, & Zabel, Reference Jacobson, Tarazi, Levy, Mahone and Zabel2012; McCurdy, Jacobson, Tarazi, Mahone, & Zabel, Reference McCurdy, Jacobson, Tarazi, Mahone and Zabel2012; Ries, Zabel, Mahone, Reference Ries, Zabel and Mahone2003). In children with ADHD and disruptive behaviors, adaptive functioning has been shown to be impaired across domains, with deficits persisting into adulthood and exceeding the level of impairment expected based on intellectual functioning alone (Barkley et al., Reference Barkley, Fischer, Smallish and Fletcher2006; Crocker, Vaurio, Riley, & Mattson, Reference Crocker, Vaurio, Riley and Mattson2009; Roizen, Blondis, Irwin, & Stein, Reference Roizen, Blondis, Irwin and Stein1994; Stein, Szumowski, Blondis, & Roizen, Reference Stein, Szumowski, Blondis and Roizen1995). Both externalizing and internalizing problems have been linked with adaptive deficits, specifically in the social realm, in youth with epilepsy (Austin, Smith, Risinger, & McNelis, Reference Austin, Smith, Risinger and McNelis1994).
The various streams of research described above highlight adaptive dysfunction across clinical/medical groups and suggest several potential contributors/etiologies. Much of the research to this point has linked distinct clinical/medical populations (e.g., spina bifida) with unique contributors to adaptive dysfunction (e.g., executive dysfunction). While shared group characteristics can be useful for a general treatment planning approach, the heterogeneity that exists within clinical groups as well as the potential for unique cognitive/behavioral profiles across clinical groups likely have diagnostic and treatment planning relevance as well. In short, both clinical/medical group status and cognitive/behavioral profile may have relevance for treatment and intervention planning targeting adaptive dysfunction. Identification of poor adaptive functioning across clinical/medical groups has clinical practice implications, including highlighting the need for uniform assessment of adaptive functioning and helping to justify the need for increasing support for the development and maintenance of functional skills in children who may have a neurobehavioral disorder without frank intellectual impairment. Although not well-documented in the literature, evidence is emerging that impaired adaptive functioning places children at significant risk of delayed achievement of adult milestones (e.g., living independently, holding down a job, developing meaningful relationships) or failing to achieve them altogether (e.g., Davis, Shurtleff, Walker, Seidel, & Duguay, Reference Davis, Shurtleff, Walker, Seidel and Duguay2004). As such, identifying and recognizing children most at risk for adaptive dysfunction should be a priority of assessment professionals in general.
One method for characterizing cognitive/behavioral profile, regardless of clinical/medical group status, is to organize new groups of cases according to shared cognitive/behavioral characteristics using cluster analysis (Everitt, Landau, Leese, & Stahl, Reference Everitt, Landau, Leese and Stahl2011). This technique allows researchers to maximize similarity within groups and differences across groups, such that individuals within the same cluster resemble each other and are different in some respect from individuals in other clusters (Everitt et al., Reference Everitt, Landau, Leese and Stahl2011). The aim of this study was to determine whether there were distinct cognitive/behavioral profiles associated with adaptive functioning within a large, clinically referred, heterogeneous sample. While adaptive dysfunction is often associated with impaired intellectual ability, we hypothesized that children characterized by dysregulated behavioral and emotional presentation would have comparable levels of adaptive dysfunction relative to children with isolated intellectual deficits.
Methods
Participants
For the purposes of this study, de-identified patient records were accessed from the clinical database of the Department of Neuropsychology at Kennedy Krieger Institute (KKI). Data are routinely entered into this database by department clinicians via the electronic health record, and securely maintained by the Information Systems department at KKI. Data were collected from 2006 to 2010. Research was conducted in accordance with the Helsinki Declaration. Upon receiving approval from the Institutional Review Board of the Johns Hopkins University School of Medicine, the de-identified clinical database was queried, and a limited dataset was constructed of patients between the ages of 6 and 16 years of age for whom valid scores were available for adaptive (Adaptive Behavioral Assessment System—Second Edition [ABAS-II], Harrison & Oakland, Reference Harrison and Oakland2003), intellectual (Wechsler Intelligence Scales for Children—Fourth Edition [WISC-IV], Wechsler, Reference Wechsler2003), and behavioral measures (Behavior Rating Inventory of Executive Functioning [BRIEF], Gioia, Isquith, Guy, & Kenworthy, Reference Gioia, Isquith, Guy and Kenworthy2000, and Behavior Assessment Scale for Children—Second Edition [BASC-2], Reynolds & Kamphaus, Reference Reynolds and Kamphaus2004). No participants were explicitly excluded from the study; however, all participants were administered a WISC-IV, meaning that they could appropriately complete this measure with regard to language, motor, and cognitive functioning. Please see Table 1 for a correlation matrix of all variables used in the cluster analysis as well as the ABAS-II GAC.
Table 1 Correlation matrix for variables used to create the clusters as well as the ABAS-II General Adaptive Composite.

Note. ABAS-II = Adaptive Behavior Assessment System, Second Edition; GAC = General Adaptive Composite; WISC-IV = Wechsler Intelligence Scale for Children, Fourth Edition; VCI = Verbal Comprehension Index; PRI = Perceptual Reasoning Index; PSI = Processing Speed Index; WMI = Working Memory Index; BASC-2 = Behavior Assessment Scale for Children, Second Edition (BASC-2); Ext. Prob. = Externalizing Problems; Int. Prob. =Internalizing Problems; BRIEF = Behavior Rating Inventory of Executive Function.
*p < .001. ABAS-II and WISC-IV scores are standard scores; BRIEF and BASC-2 scores are T-scores, with higher scores indicating more problematic functioning.
The final sample included 348 children (68% male; Mean age = 10.16; SD = 2.77; Range = 6–16 years), for whom records included the aforementioned measures given at the same time point, age at time of assessment, sex, and billing diagnosis. All patients included in the dataset had been referred for outpatient neuropsychological assessment. Descriptive information is presented in Table 2. Most frequent billing diagnoses in this mixed clinical sample included ADHD (54%), adjustment reaction (9%), and encephalopathy (8%).
Table 2 Descriptive statistics for the four clusters
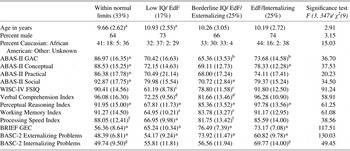
Note. ABAS-II and WISC-IV scores are presented as standard scores; BRIEF and BASC-2 scores are presented as T-scores, with higher scores indicating more problematic functioning. Superscript letters denote clusters with significantly different means. Abbreviations: % refers to the percent of the 348 children included in this study in each cluster; EdF, executive dysfunction; ABAS-II, Adaptive Behavior Assessment System, Second Edition; GAC, General Adaptive Composite; BASC-2, Behavior Assessment Scale for Children, Second Edition; BRIEF, Behavior Rating Inventory of Executive Function; GEC, General Executive Composite; WISC-IV, Wechsler Intelligence Scale for Children, Fourth Edition; FSIQ, Full Scale IQ; Within Normal Limits Cluster: broadly age-appropriate intelligence, executive functioning, and behavioral/emotional functioning; Low IQ/ EdF Cluster: impaired intelligence and mild executive dysfunction without overt internalizing or externalizing behavioral/emotional symptoms; Borderline IQ/EdF/Externalizing Cluster: borderline-impaired intelligence, high levels of executive dysfunction, and more externalizing than internalizing behavioral problems; EdF/Internalizing Cluster: broadly average intelligence, high levels of executive dysfunction, and more internalizing than externalizing behavior problems).
* Denotes a mean score that is significantly different from all other groups.
a–gSuperscript letters denote significant differences between groups.
Measures
Adaptive Behavior Assessment System—Second Edition (ABAS-II, Harrison & Oakland, Reference Harrison and Oakland2003)
The ABAS-II is a parent-report questionnaire assessing functional daily living skills. For children in the age range employed by this study, the ABAS-II divides adaptive functioning into nine skill areas, which are subsumed under three theoretically derived domains: the Conceptual domain (Communication, Functional Academics, and Self-Direction skill areas), Social domain (Leisure and Social areas), and Practical domain (Community Use, Home Living, Health and Safety, and Self-Care skill areas). All of the individual skill areas contribute to a General Adaptive Composite (GAC). A tenth skill area, Work Skills, can be administered to older adolescents and young adults, but was not part of this study given the age range of the sample. The ABAS-II GAC has strong internal consistency (Cronbach's α = .98) as do the domain (Cronbach's α = .86–.93) and skill area scores (Cronbach's α = .95–.97). Stability over time also is strong (GAC corrected test–retest reliability r = .93, domain corrected test–retest r = .89–.93, skill area corrected test–retest r = .84–.92).
Behavior Rating Inventory of Executive Function (BRIEF, Gioia et al., Reference Gioia, Isquith, Guy and Kenworthy2000)
The BRIEF is a parent questionnaire assessing executive functioning behaviors in children 5–18 years old. Executive functions involve the management of cognitive, emotional, and behavioral functions, which are typically involved in problem-solving behavior. The 86 BRIEF items are organized into eight individual scales, and are further organized into two factors and one overall composite score. The Behavioral Regulation Index (BRI) is the first factor and reflects the child's ability to shift cognitive set (Shift scale), use inhibitory control (Inhibit scale), and modulate emotions and behavior (Emotional Control scale). The Metacognition Index (MI) is the second factor, and reflects a child's ability to initiate, plan, organize, and sustain future-oriented problem solving in working memory. This index is comprised of the Initiate, Working Memory, Plan/Organize, Monitor, and Organization of Materials scales. The Global Executive Composite (GEC) is a composite of the BRI and MI. Internal consistency for the GEC is high (rα = .98), with good test–retest reliability (r = .81), and results are similar for the two indices.
Behavior Assessment System for Children-Second Edition (BASC-2, Reynolds & Kamphaus, Reference Reynolds and Kamphaus2004)
The BASC-2, parent form is a caregiver-report questionnaire that measures many aspects of behavior and child personality. This study used the Externalizing and Internalizing Problems composite scores of the BASC-2. The Externalizing Problems composite is comprised of the Hyperactivity, Aggression, and Conduct Problems scales, which are all characterized by disruptive behavior. The Internalizing Problems composite consists of the Anxiety, Depression, and Somatization scales. Symptoms of externalizing behaviors are often more observable than those of internalized distress, which may account for slightly higher levels of inter-rater agreement on the Externalizing Problems composite (Reynolds & Kamphaus, Reference Reynolds and Kamphaus2004). Internal consistency for the Internalizing and Externalizing Problems composites is high (rα ranging from .89 to .94), with good test–retest reliability for both Externalizing Behaviors (r from .81 to .91) and Internalizing Behaviors (r from .77 to .92).
Wechsler Intelligence Scale for Children—Fourth Edition (WISC-IV, Wechsler, Reference Wechsler2003)
The WISC-IV is a widely used, standardized measure of intellectual functioning. In addition to providing a Full Scale IQ (FSIQ), this measure provides four Index scores: Verbal Comprehension, Perceptual Reasoning, Working Memory, and Processing Speed. Internal consistency for the Index scores and FSIQ is good (rα ranging from .81 to .95), with good test–retest reliability (r from .86 to .93).
Statistical Methodology
Chi-square analysis was used to determine if the observed number of children with reports of adaptive dysfunction (i.e., GAC ≤ 70) was consistent with expectations based upon the number of children displaying intellectual impairment (i.e., FSIQ ≤ 70). Examination of the correlations between the variables proposed for inclusion in the cluster analysis (the four WISC-IV Index scores, the Internalizing and Externalizing Problem composite scores from the BASC-2, and the BRI and the MI composite scores of the BRIEF) showed a high correlation between the BRI and the MI of the BRIEF (r = .66), therefore, the BRIEF's GEC was used instead as a measure of executive dysfunction (EdF). Before conducting the cluster analysis, all scores were standardized (converted to Z-scores) and scores from the BRIEF and BASC-2 were reversed so that lower scores on all measures were indicative of impairment. These Z-scores were used in the cluster analysis. ABAS-II scores were not used in the determination of clusters.
Data were screened for outliers (Z score > ± 4.0). Twenty children had a score ± 4.0 (five elevated on the BRIEF GEC, six elevated on the BASC-2 Internalizing Scale, eight elevated on the BASC-2 Externalizing scale, and one elevated on the BASC-2 Internalizing and Externalizing scales). Examination of histograms revealed clear approximation of the bell curve with some skew across measures in the expected directions for a clinically referred sample (negative skew for the BASC-2 and BRIEF T-scores indicating a tendency toward more problems on these scales; positive skew on the WISC-IV indicating a tendency toward lower scores across Index scores). When results were re-run without these outliers, the clusters did not change appreciably. Additionally, scores of this nature are frequently encountered in the children we see for neuropsychological evaluation and were believed to accurately reflect the nature of impairment. Consequently, these data were retained in the analyses.
To test for relatively distinct clinical groups, a hierarchical cluster analysis using Ward's method with a squared Euclidean distance measure was conducted to cluster patients with similar cognitive/behavioral profiles using IBM SPSS Statistics 19. Our methodology was similar to that used in other studies (e.g., Hermens et al., Reference Hermens, Redoblado Hodge, Naismith, Kaur, Scott and Hickie2011; Soenen, Van Berckelaer-Onnes, & Scholte, Reference Soenen, Van Berckelaer-Onnes and Scholte2009; Thaler et al., Reference Thaler, Bello, Randall, Goldstein, Mayfield and Allen2010). The number of clusters was determined by examining the agglomeration coefficients and dendrogram for three to five clusters. This indicated that a four cluster solution was best for distinguishing cases. These clusters were subsequently judged on their clinical meaningfulness. The reliability of the clusters found using Ward's method was confirmed using average linkage, with 78% agreement in group membership across the two hierarchical methodologies and a high degree of clinical similarity across the clusters created. Additionally, k-medians iterative partitioning using results from Ward's method as initial starting seed points showed moderate agreement with Ward's method (66%), and, again, the clusters were highly similar in their pattern of clinical strengths and weaknesses to those obtained using Ward's and average linkage methodologies.
One-way between-subject analyses of variance (ANOVAs) were used to test for differences between the clusters on demographic variables and on the ABAS-II. The Tukey's honestly significant difference test was used to determine which means differed significantly. The χ2 test was used to test for differences between the clusters on sex and ethnicity.
RESULTS
In this mixed clinical sample of 348 children referred for neuropsychological assessment, overall adaptive functioning (ABAS-II GAC) fell at least one standard deviation below the normative mean for the majority (71%; n = 246), with the GAC falling at least two standard deviations below the normative mean in 156 of these children (45% of the sample). In contrast, fewer children had FSIQ scores that fell either 1 (n = 194; 56%) or 2 (n = 79; 23%) standard deviations below the normative mean. Far more children presented with reports of adaptive dysfunction than would be expected based upon low FSIQ alone (χ2 = 20.48; p < .001). As would be expected, there was a high number of children for whom parent report of behavioral problems resulted in scores that were one or two standard deviations above the mean, respectively, for internalizing (41%; 18%), externalizing (42%; 20%), or executive (76%; 42%) concerns (before our having reversed the behavioral scores).
Mean scores and statistically significant differences between the clusters are presented in Table 2. Cluster profiles are presented in Figure 1. For ease of interpretation, clusters were named using a criteria of impairment defined as the mean Z score ≤ −1.5 (n.b., BASC-2 and BRIEF scores were reversed).

Fig. 1 Profile of cluster mean scores (with standard error bars) across measures. Note. All scores were converted to z-scores, and scores on the BASC-2 and BRIEF were reverse scored, such that lower scores on all measures indicated poorer functioning. Abbreviation: WNL = Within Normal Limits. Within Normal Limits Cluster: broadly age-appropriate intelligence, executive functioning, and behavioral/emotional functioning; Low IQ/ EdF Cluster: impaired intelligence and mild executive dysfunction without overt internalizing or externalizing behavioral/emotional symptoms; Borderline IQ/EdF/Externalizing Cluster: borderline-impaired intelligence, high levels of executive dysfunction, and more externalizing than internalizing behavioral problems; EdF/Internalizing Cluster: broadly average intelligence, high levels of executive dysfunction, and more internalizing than externalizing behavior problems).
The four clusters were best distinguished by various levels of intellectual ability (IQ), executive functioning (i.e., executive dysfunction [EdF]), and emotional/behavioral functioning (i.e., externalizing and internalizing behavior problems). The mean scores of one cluster fell broadly within normal limits (i.e., the Within Normal Limits [WNL] Cluster) on measures of intelligence (FSIQ M = 90.41), executive functioning, and behavioral/emotional functioning. The Low IQ/ EdF Cluster was characterized by low intelligence (FSIQ M = 61.19) and mild executive dysfunction (without overt internalizing or externalizing behavioral/emotional symptoms). The Borderline IQ/EdF/Externalizing Cluster was characterized by borderline-impaired intelligence (FSIQ M = 78.80), high levels of reported executive dysfunction, and markedly disruptive behavior (more externalizing than internalizing behavioral problems). The EdF/Internalizing Cluster was characterized by broadly average intelligence (FSIQ M = 91.80), high levels of reported executive dysfunction, and high levels of emotional dysregulation (more internalizing than externalizing behavior problems).
Adaptive functioning (ABAS-II GAC) was most intact in the cluster characterized by a generally intact cognitive and behavioral profile (WNL Cluster), although the mean GAC was still almost one standard deviation below the mean of the ABAS-II normative sample. In contrast, mean scores suggestive of impaired adaptive functioning were noted in the other three clusters, with the mean GAC of the Borderline IQ/EdF/Externalizing Cluster significantly more impaired than that of the EdF/Internalizing Cluster. One-way ANOVA showed large effect sizes for the ABAS-II and three domains (GAC partial η 2 = .24, Conceptual partial η 2 = .25, Social partial η 2 = .23, Practical partial η 2 = .15). There were significant differences on the GAC and three domains between the WNL Cluster and all other clusters. The EdF/Internalizing Cluster had significantly stronger, although still in the borderline-impaired range, scores on the GAC compared to the Borderline IQ/EdF/Externalizing Cluster. The EdF/Internalizing Cluster also had significantly different scores on the Conceptual domain compared to the other groups. Finally, the Borderline IQ/EdF/Externalizing Cluster had significantly lower scores on the Social domain than all other clusters. There were no significant differences between the clusters associated with sex or ethnicity (see Table 2). One-way ANOVA indicated a significant difference in mean age between the WNL and Low IQ/ EdF Clusters, with children in the Low IQ/ EdF Cluster being significantly older.
Impairments in adaptive functioning have traditionally been associated with low intellectual functioning as conceptualized in the diagnosis of mental retardation/intellectual disability and, as expected, report of low adaptive ability was characteristic of the Low IQ/EdF Cluster. Consistent with our hypotheses, comparable levels of adaptive dysfunction were also seen in children in the Borderline IQ/EdF/Externalizing and EdF/Internalizing Clusters, despite the fact that children in these clusters had significantly higher IQ scores than children in the Low IQ/EdF Cluster. Consequently, we examined the executive and behavioral profiles of children in these two clusters (i.e., the Borderline IQ/EdF/Externalizing and EdF/Internalizing Clusters) in greater detail in an effort to better characterize them (see Table 3). Although largely comparable in terms of executive dysfunction, the Borderline IQ/EdF/Externalizing Cluster had significantly more symptoms of disinhibition (BRIEF) than the EdF/Internalizing Cluster. However, both clusters had clinically significant elevations on all scales of the BRIEF, with the exception of one scale, Organization of Materials, which was not elevated in either cluster. As expected, all externalizing scales were significantly more elevated in the Borderline IQ/EdF/Externalizing Cluster, while the internalizing scales were more elevated in the EdF/Internalizing Cluster. Notably, both clusters had elevated scores on scales of attention problems and hyperactivity, with significantly more problems noted in the Borderline IQ/EdF/Externalizing Cluster.
Table 3 Descriptive statistics on the BRIEF and BASC-2 for the Borderline IQ/EdF/Externalizing and EdF/Internalizing Clusters

Note. BRIEF and BASC-2 scores are presented as T-scores, with higher scores indicating more problematic functioning. ABAS-II skill area scores are presented as scaled scores, with higher scores indicating more intact functioning. EdF, executive dysfunction; Behavior Assessment Scale for Children, Second Edition (BASC-2); Behavior Rating Inventory of Executive Function (BRIEF); ABAS-II, Adaptive Behavior Assessment System, Second Edition. Low IQ/ EdF Cluster: impaired intelligence and mild executive dysfunction without overt internalizing or externalizing behavioral/emotional symptoms; Borderline IQ/EdF/Externalizing Cluster: borderline-impaired intelligence, high levels of executive dysfunction, and more externalizing than internalizing behavioral problems.
Discussion
The results of this study highlight the prevalence of adaptive dysfunction within a mixed clinical sample. The vast majority of these referred youth presented with at least mild adaptive dysfunction based upon parent report (71%), with indication of significant and multi-domain adaptive impairment in approximately half of the sample (45%). The frequency and extent of adaptive dysfunction was far greater than would be expected based on intellectual ability alone, as the mean FSIQ was 82.97 (SD = 16.68) for the entire sample and only 23% of cases met criteria for intellectual impairment (i.e., FSIQ ≤ 70). To address this type of IQ/adaptive functioning discrepancy often seen in clinical practice (e.g., Barkley et al., Reference Barkley, Fischer, Smallish and Fletcher2006; Liss et al., Reference Liss, Harel, Fein, Allen, Dunn, Feinstein and Rapin2001; Papazoglou et al., Reference Papazoglou, King, Morris and Krawiecki2008), the current study examined a collection of additional variables that were proposed to be associated with adaptive dysfunction in clinically referred children, either in combination with global intellectual functioning or in addition to it. This investigation allowed us to explore the possibility of different cognitive/behavioral symptom clusters/profiles and their possible association with adaptive dysfunction in general. While this approach does not establish causality between these variables and adaptive dysfunction, it does help identify variables and/or combinations of variables that might contribute to adaptive dysfunction in a unique and clinically-relevant manner. As a first step, the current study sought to identify discrete cognitive/behavioral symptom clusters/profiles associated with global adaptive dysfunction.
To this end, the results of this study showed that the children within our clinically referred sample could be divided into relatively distinct clusters with cognitive/behavioral profiles distinguished by patterns of intellectual, behavioral, emotional, and executive functioning. Consistent with our hypothesis, significant adaptive impairment was evident across three of the four clinical clusters (i.e., the Low IQ/ EdF cluster, the Borderline IQ/EdF/Externalizing cluster, and the EdF/Internalizing cluster), highlighting the pervasive nature of impaired adaptive functioning in children referred for neuropsychological assessment and the association between behavioral and emotional regulation difficulties and adaptive impairment. Adaptive scores were below the fifth percentile for these three clusters, while they were within one standard deviation from the mean within the WNL cluster.
The one cluster of children, who were found to have age-appropriate adaptive functioning in general, the WNL cluster, was characterized by age-appropriate mean scores on both performance measures (WISC-IV) and parent-report measures. While educational diagnoses were not available in this limited dataset, we suspect that children in the WNL cluster were likely referred for more specific attention or learning concerns (e.g., a learning disability) which may have less overt intellectual, behavioral, or emotional features as well as a more circumscribed and/or less pronounced negative effect upon daily adaptive functioning.
Low intellectual ability was the primary characteristic of one of the symptom clusters, and scores of children in this group (i.e., Low IQ/EdF) were the most consistent with a “classic” intellectual disability/mental retardation presentation characterized by co-occurring intellectual and adaptive impairments. Although significant adaptive impairments also were evident in children in the Borderline IQ/EdF/Externalizing and EdF/Internalizing clusters, mean IQ scores in both of these groups did not suggest significant intellectual deficits. Children in these clusters were better characterized when both IQ and their broader emotional, behavioral, and executive phenotype were taken into account. Despite their grossly intact intelligence, children with emotional, behavioral, and executive dysfunction demonstrated comparable (and potentially worse) adaptive functioning relative to those children characterized primarily by low IQ. Indeed, the Borderline IQ/EdF/Externalizing cluster had the lowest mean scores on the ABAS-II of all of the symptom cluster groups, suggesting that behavioral and executive difficulties combined with borderline-impaired intellectual functioning may have a cumulative, and particularly disruptive, effect on adaptive functioning.
Between the Borderline IQ/EdF/Externalizing cluster and the EdF/Internalizing cluster there were differences in the behavioral/emotional presentation that contributed to their stratification to different clusters. Specifically, the Borderline IQ/EdF/Externalizing cluster had significantly higher symptom report of behavioral disinhibition, conduct problems, and aggression, while the EdF/Internalizing cluster had significantly higher symptom report of anxiety, depression, and somatization (suggestive of comorbid affective dysregulation). While both groups showed adaptive dysfunction, post hoc comparison of individual ABAS-II skill areas revealed that children in the Borderline IQ/EdF/Externalizing were significantly more impaired in the majority of adaptive skill areas. As such, among all of the patient groups in this clinically referred sample, this cluster of patients with borderline IQ, executive dysfunction, and externalizing behavioral problems appears to have the greatest relative risk of adaptive dysfunction.
Future inquiry will be necessary to determine if the manifestation of adaptive dysfunction is qualitatively different when children from these two symptom clusters are compared. For example, do the socially based symptoms of adaptive dysfunction in children from the Borderline IQ/EdF/Externalizing cluster (e.g., potentially intrusive/impulsive social interactions) differ qualitatively from the social symptoms of children from the EdF/Internalizing cluster (e.g., potential symptoms of social anxiety/avoidance)? If the manifestation of adaptive dysfunction is qualitatively different across these two clusters, it would underscore the need for recommendations to address child-specific areas of adaptive impairment. Better characterization of children within these clusters may help to identify relevant school-based recommendations and support the use of different types of intervention designed to address the specific manifestations of adaptive dysfunction.
The results of this study lend support to our proposal that there may be multiple clinical contributors to an impaired adaptive presentation, with executive dysfunction along with emotional/behavioral dysfunction playing key roles in adaptive dysfunction in children without intellectual disability. Evidence of significant adaptive impairment in the absence of intellectual impairment suggests that assessment of adaptive functioning should not be limited simply to children for whom there is a question of intellectual disability. Instead, these findings support expanding the conceptualization of adaptive impairment to include children with cognitive, executive, or behavioral/mood symptoms. Doing so would be consistent with the DSM-IV criteria (American Psychiatric Association, 2000), which requires evidence of functional impairment (social, occupational, academic, or other important areas) for many diagnoses including behavioral and mood disorders. There is, however, debate about the criterion of functional impairment in the upcoming DSM-5. Some argue (e.g., Achenbach, Reference Achenbach2009; Maser et al., Reference Maser, Norman, Zisook, Everall, Stein, Schettler and Judd2009) that impairment should not be required in order for a diagnosis to be made. This argument stems from several areas of concern, including how to quantify impairment and confirm that it is due to the disorder in question as well as the potential that this criterion prevents people from being diagnosed with a disorder if they do not experience (or have not yet experienced) a functional impact. The results of this study suggest that the functional impact of childhood neurobehavioral disorders can be substantial and that clinicians should directly assess adaptive impairment in children, but determining the necessity of this component for diagnosis is beyond the scope of this study.
There is emerging research demonstrating that impaired adaptive functioning in childhood is associated with delayed achievement of adult milestones or failure to achieve them altogether (e.g., Davis et al., Reference Davis, Shurtleff, Walker, Seidel and Duguay2004). Consequently, identifying children most at risk for adaptive dysfunction should be a priority of assessment professionals in general. Moreover, although our current model cannot decisively speak to the cause of adaptive impairment, it does raise the possibility that there may be different avenues to remediating adaptive dysfunction depending on the associated (and possibly causative) variables. On a very simple level, increased structure at home and/or a stimulant medication might be most helpful in boosting adaptive skills in children within the Borderline IQ/EdF/Externalizing cluster. In contrast, children presenting in the EdF/Internalizing cluster might require intervention to decrease symptoms of anxiety and depression such as cognitive-behavioral therapy or psychotropic medication in addition to behavioral intervention. In children with adaptive difficulties associated with low IQ, remediation efforts might be best directed toward rote learning of adaptive tasks. There is currently a paucity of research examining not only remediation of adaptive skills, but also changes in adaptive functioning over time and how these skills may be associated with important adult milestones including completion of higher education, holding down a job, living independently, getting married, and raising a family. These are critical areas for future research.
This study has several limitations. Most importantly, our four cluster solution has only modest reliability across methodologies, and further research is needed to assess the reliability of these cluster profiles and subsequently to assess their predictive validity with respect to identifying children who continue to demonstrate adaptive impairments over time. Additionally, while we are assuming some contributing effect of behavioral variables on adaptive functioning, the data in this study are correlational and it is unclear whether, or in what manner, the relationship between adaptive functioning, intelligence, and behavioral regulation may change over time. Limited medical/diagnostic information was available about this sample. Medical information would allow for the examination of whether certain diagnoses are strongly associated with a specific cluster profile, and could allow for more tailored assessment of areas of possible impairment. Family factors including parental expectations, level of parent education, and socio-economic status may affect the development of adaptive skills; however, information about these variables was not available. This was a clinically referred sample, so the results may not generalize to a less symptomatic population. Future research should seek to address these limitations as well as to replicate these findings using other methodologies (e.g., self-report of behavioral symptoms, teacher report of adaptive functioning). Research also should examine the role contextual factors, including family functioning and parental expectations, play in the development of adaptive skills.
Acknowledgments
This work was supported by P30 HD-24061 (Intellectual and Developmental Disabilities Research Center) and the Johns Hopkins University School of Medicine Institute for Clinical and Translational Research, an NIH/NCRR CTSA Program. There are no conflicts of interest. This research received no specific grant from any funding agency, commercial or not-for-profit sectors. We thank Gayane Yenokyan, Ph.D., from the Johns Hopkins School of Public Health for her statistical consultation.






