Introduction
Supracricoid laryngectomy with cricohyoidoepiglottopexy is a function preservation surgery for laryngeal cancer. Nowadays, supracricoid laryngectomy with cricohyoidoepiglottopexy is widely recognised as a useful surgical treatment because of established surgical technique and oncological safety.Reference Laccourreye, Laccourreye, Weinstein, Menard and Brasnu1,Reference Nakayama, Laccourreye, Holsinger, Okamoto and Hayakawa2 This procedure allows patients to breathe without a permanent tracheostoma and restores voice and swallowing.Reference Weinstein, El-Sawy, Ruiz, Dooley, Chalian and El-Sayed3–Reference Farrag, Koch, Cummings, Goldenberg, Abou-Jaoude and Califano6 Post-operative outcomes including satisfactory swallowing function or risk factors for pulmonary complications have been investigated in some studies.Reference Nakayama, Yao, Nishiyama, Nagai, Ito and Yokobori7–Reference Piquet and Chevalier10
In the Department of Otorhinolaryngology of Kitasato University Hospital, swallowing rehabilitation is performed for all patients to enhance restoration of swallowing function after the surgery. In following these patients, particularly in terms of swallowing function, we have evaluated post-operative deglutition using a videofluoroscopic swallowing study protocol. In our experience, the patients can maintain sufficient swallowing function once acquired. Furthermore there is a trend for their swallowing function to improve after the surgery. Even patients over 65 years old showed gradual improvement and stable long-term swallowing. However, laryngeal aspiration or penetration persisted for a long time in a few elderly patients. There are several reports that severe aspiration is an important indicator of pulmonary complications after supracricoid laryngectomy with cricohyoidoepiglottopexy.Reference Alajmo, Fini-Storchi, Agostini and Polli11,Reference Alicandri-Ciufelli, Piccinini, Bergamini, Ruberto, Ghidini and Marchioni12
Until now, there have been few quantitative kinematic analyses to detect which physiological factors lead to unfavourable events, such as laryngeal penetration or aspiration after supracricoid laryngectomy with cricohyoidoepiglottopexy. Therefore, in this study, we focused on patients over 65 years old and attempted to identify factors impacting swallowing safety by analysis of videofluoroscopic swallowing studies and to identify compensatory swallowing mechanisms in patients who underwent supracricoid laryngectomy with cricohyoidoepiglottopexy.
Materials and methods
Measurement and analysis were performed after study approval from the Institutional Review Board of Kitasato University Hospital (approval number: B ethics 11-107).
Patients
Patients who had undergone supracricoid laryngectomy with cricohyoidoepiglottopexy at the Department of Otorhinolaryngology of Kitasato University Hospital between April 1997 and January 2012 were included. Videofluoroscopic swallowing studies from these patients to evaluate post-surgical deglutition five years after supracricoid laryngectomy with cricohyoidoepiglottopexy were sorted. Subsequently, we reviewed videofluoroscopic swallowing studies that fulfilled the criteria for inclusion using the method that follows.
Videofluoroscopic swallowing study method
Radiographic studies were conducted on a properly collimated Finescope300 Fluorex unit (Toshiba, Otawara, Japan) that provided a 63 kV, 1.2 mA-type output for the full field of view mode (9-inch input phosphor diameter). Data from the fluoroscopy studies were recorded on a multidrive digital versatile disk (‘DVD’) and hard disk recorder (‘HDD') RD-XS31 (Toshiba, Minato, Japan). The swallowing studies were recorded at 30 frames per second. Patients received a modified barium swallowing study with videofluoroscopy. Patients were asked to swallow a 20 cc bolus of Barytgen® (barium sulfate; 80 per cent weight-to-volume ratio; Fushimi Pharmaceutical, Marugame, Japan) from a cup. Some patients performed less than 20 cc bolus swallowing in order to maintain safety. We excluded such patients from the analysis. In this paper, ‘penetration’ is defined as the entry of barium sulfate into the neoglottis (between the preserved arytenoids and the tongue base) with or without residue, and ‘aspiration’ is defined as the entry of contrast medium into the airway (top of air column just below the neoglottis) with or without residue.
Measurement protocol
We performed measurements on the fluoroscopy study data based on the method published by Leonard and Kendall.Reference Kendall and Leonard13 Identification information was erased from each videofluoroscopic swallowing study video file, and only the period necessary for the measurement was trimmed. At the time of image measurement, laryngeal penetration and aspiration were automatically known. However, pre-operative patient information, surgical details and the peri-operative period were hidden from the raters.
All quantitative measures were made from lateral views. We obtained timing measures by observing the video studies in slow motion and frame-by-frame (forward, reverse) modes on a computer. The timings of both bolus transit and selected swallowing gestures were determined. Each timing measurement was detected by the time counter embedded in QuickTime Player 7 (version 7.6.6; Apple, Cupertino, USA). Duration was also measured with this timer.
Timing measures included: (1) the duration of hyoid bone remaining in maximum superior or anterior displacement; (2) the duration of initial opening of the pharyngoesophageal sphincter to the time of first entrance of the bolus through the pharyngoesophageal sphincter; (3) the duration of pharyngoesophageal sphincter opening; (4) the duration from onset of swallowing to airway closure start, which was detected by the first anterior movement of the arytenoid, to an end by firm contact of the arytenoid to the epiglottis (tongue base); (5) the duration from first firm contact of arytenoid-epiglottis to close the neoglottis (between the preserved arytenoids and the tongue base) to the point of airway re-opening; (6) oropharyngeal transit time: bolus transit time through oral-pharyngeal section, which is the duration from first movement of the bolus head past the posterior nasal spine that represents swallowing transit onset to first exit of the bolus from the valleculae; and (7) hypopharyngeal transit time: bolus transit time through the hypopharynx, which is the duration from first exit of bolus from the valleculae to clearance of the bolus tail from the pharyngoesophageal sphincter (Figure 1).

Fig. 1. Timing measures for bolus movements and swallow gestures: definitions. (a) Swallow gesture time. Hmax = the duration of the hyoid bone remaining in maximum superior or anterior displacement. (b) Swallow gesture time. PESstart = the duration of initial opening of the pharyngoesophageal sphincter (PES) to the time of first entrance of the bolus through the pharyngoesophageal sphincter; PESopen = the duration of pharyngoesophageal sphincter opening. (c) Swallow gesture time. AEstart = the duration from onset of swallowing to airway closure start, which was detected by the first anterior movement of the arytenoid, to an end by firm contact of the arytenoid to the epiglottis (tongue base); AEclose = the duration from first firm contact of arytenoid-epiglottis to close the neoglottis to the point of airway re-opening. (d) Bolus transit time. OPT = bolus transit time through oral-pharyngeal section, that is the duration from first movement of the bolus head past the posterior nasal spine that represents swallowing transit onset to first exit of the bolus from the valleculae; HPT = bolus transit time through the hypopharynx, that is the duration from first exit of bolus from the valleculae to clearance of the bolus tail from the PES.
Displacement measures were performed on a MacBook Air computer (Apple). The Image J (version 1.45 National Institutes of Health) software program was utilised for analysis of fluoroscopic images. Area and distance measurements were made after calibration of the digitised image to a ruler positioned in front of the faces of the study participants during filming.
Displacement measures included: (1) distance between hyoid position at ‘hold’ (i.e. to the bolus held in the oral cavity) and at its point of maximal anterior and superior excursion during the swallow; (2) the distance from inferior hyoid bone to inferior cricoid cartilage or top of air column anteriorly, which represents larynx–hyoid distance; (3) the narrowest point of opening between C3 and C6 of cervical vertebra during maximal distention for bolus passage; (4) pharyngeal area holding the bolus in the mouth at rest; (5) pharyngeal area at maximum constriction; (6) pharyngeal constriction ratio: the ratio of the pharyngeal area at maximum constriction divided by the pharyngeal area holding the bolus in the mouth at rest to assess pharyngeal constriction (Figure 2).

Fig. 2. Displacement measures: definitions. (a) Hyoid maximum displacement (Hmax). The distance between hyoid position at ‘hold’ (i.e. to the bolus held in the oral cavity) and at its point of maximal anterior and superior excursion during the swallow. (b) Pharyngoesophageal sphincter (PES) opening. PESmax = the narrowest point of opening between C3 and C6 during maximal distention for bolus passage. (c) HLhold = distance from inferior hyoid bone to inferior cricoid cartilage or top of air column anteriorly that represents larynx–hyoid distance. (d) PAhold = pharyngeal area (cm2) measured in the lateral view during the ‘hold’ position. Its outline was defined posteriorly by the posterior pharyngeal wall from the mid-portion of the tubercle of the atlas down to the level corresponding to the height of the top of the arytenoid cartilages. Inferiorly the outline was carried forward from this point over the arytenoid cartilages and anteriorly to outline the epiglottis, vallecula, and tongue base to the point at which the soft palate came into contact with the tongue base. The outline was then carried over the pharyngeal surface of the soft palate to the level, superiorly, of the posterior nasal spine. The superior border was a straight line between the posterior nasal spine and the midpoint of the tubercle. (e) PAmax = the pharyngeal area at maximal constriction. It was defined by the outline of the same structures during maximal constriction.
Data analyses
All data are presented as mean and standard deviation. Baseline characteristics and each measurement's values between the patient groups were compared with the chi-square statistic and unpaired t-tests with Welch's correction were performed to compare differences for categorical and continuous variables, respectively.
Factors predicting laryngeal penetration and aspiration were first identified using univariate analysis. Those with p-values less than 0.25 were entered into a stepwise multiple logistic regression. Significant independent factors were considered when p < 0.05. We used receiver operating characteristic curves to anticipate the cutoff point, then considered the odds ratio, chi-square value, p-value and 95 per cent confidence interval (CI) to determine it. Additionally, the identified predicting factors of displacements were divided into two groups to show the differences: one with previous radiation history and the other without. We also examined the extracted factors of duration in the cases with unilateral and bilateral arytenoids to compare them with each other. Data were analysed using SPSS® (version 21) statistical software.
Results
Patients
Eighty-nine patients (87 male and 2 female) underwent supracricoid laryngectomy with cricohyoidoepiglottopexy at the Department of Otorhinolaryngology of Kitasato University Hospital between April 1997 and January 2012. We collected videofluoroscopic swallowing studies from 78 patients through swallow therapy in an attempt to regain their swallowing function. Fourteen patients aged under 65 years and 12 patients who had incomplete videofluoroscopic swallowing studies according to the criteria were excluded. Ultimately, 52 patients’ videofluoroscopic swallowing studies were analysed.
Baseline characteristics for all patients and the two subgroups are listed in Table 1. Baseline demographic information included age, the number of preserved arytenoids or radiation history before surgery, and the period from the surgery to videofluoroscopic swallowing study. All participants were male and over 65 years old. Studies were performed around five years after surgery. There were no demographic differences among the groups in age, the number of preserved arytenoids or radiation history, and the period from supracricoid laryngectomy to videofluoroscopic swallowing study. No patients had a tracheostoma, nasogastric tube or recurrent pulmonary infections at the time of videofluoroscopic swallowing study. No patients had uncontrolled systemic diseases when undergoing videofluoroscopic swallowing study. No patients received radiation therapy following supracricoid laryngectomy with cricohyoidoepiglottopexy. Seventeen patients (33 per cent) received supracricoid laryngectomy with cricohyoidoepiglottopexy as a salvage surgery for radiation failure.
Table 1. Participant demographic data
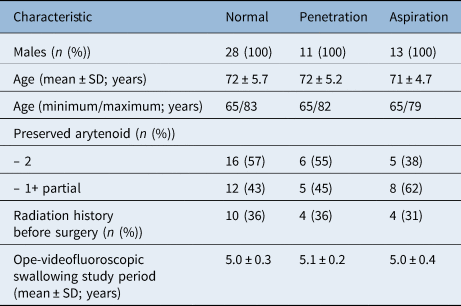
SD = standard deviation; Ope-videofluoroscopic swallowing study = time between surgery and the videofluoroscopic swallowing study test
Surgery and rehabilitation
Supracricoid laryngectomy with cricohyoidoepiglottopexy results in complete and bilateral resection of the paraglottic space including, when required, one arytenoid cartilage on the tumour-bearing side. The thyroarytenoid and cricothyroid muscles of intrinsic laryngeal muscles were removed by the present surgical procedure in all cases. Superior laryngeal nerves were preserved, and at least one cricoarytenoid unit was preserved and sutured in position anterosuperiorly. In order to prevent the posterior part of the cricoid cartilage from loosing, arytenoid cartilage fixation was a contraindication for supracricoid laryngectomy with cricohyoidoepiglottopexy. Early decannulation and early onset of swallowing rehabilitation should be considered. Swallowing rehabilitation was performed for all patients to optimise swallowing function. During the period of hospitalisation, intensive swallowing rehabilitation was performed under medical supervision and assessment by ENT doctors and speech pathologists. Swallowing rehabilitation progressed from level 3 to level 7 of the International Dysphagia Diet Standardisation Initiative descriptors provided at the hospital as early as possible. Therapy can continue after discharge, with duration depending on the quality of recovery of deglutition to a point of providing adequate nutritive needs and social adaptation.
Univariate analyses of duration and displacement measures
Table 2 shows the univariate analyses of duration measures. Normal patients, which means patients with no laryngeal penetration and aspiration, were compared with those with penetration and aspiration by univariate analysis. The measurement variables of pharyngoesophageal sphincter open (p = 0.0003), airway close (p = 0.005) and hypopharyngeal transit time (p = 0.022) were significantly related to aspiration. Table 3 shows univariate analyses of displacement measures. Significant differences were found for distance from inferior hyoid bone to inferior cricoid cartilage or top of air column anteriorly, representing larynx–hyoid distance (p = 0.023) and pharyngeal constriction ratio (p = 0.015) related to aspiration.
Table 2. Univariate analysis: swallowing gesture time factors related to penetration and aspiration

*n = 28; †n = 11; ‡n = 13. SD = standard deviation; Hmax = The distance between hyoid position at ‘hold’ (i.e. to the bolus held in the oral cavity) and at its point of maximal anterior and superior excursion during the swallow; PESopen = the duration of pharyngoesophageal sphincter opening ; Airway start = the duration from onset of swallowing to airway closure start, which was detected by the first anterior movement of the arytenoid, to an end by firm contact of the arytenoid to the epiglottis (tongue base); Airway close = the duration from first firm contact of arytenoid-epiglottis to close the neoglottis to the point of airway re-opening; Oropharyngeal transit time = bolus transit time through oral-pharyngeal section, that is the duration from first movement of the bolus head past the posterior nasal spine that represents swallowing transit onset to first exit of the bolus from the valleculae; Hypopharyngeal transit time = bolus transit time through the hypopharynx, that is the duration from first exit of bolus from the valleculae to clearance of the bolus tail from the PES.
Table 3. Univariate analysis: swallowing gesture displacement factors related to penetration and aspiration

*n = 28; †n = 11; ‡n = 13. Hmax = the distance between hyoid position at ‘hold’ (i.e. to the bolus held in the oral cavity) and at its point of maximal anterior and superior excursion during the swallow; HLhold = distance from inferior hyoid bone to inferior cricoid cartilage or top of air column anteriorly that represents larynx–hyoid distance; PESmax = narrowest point of opening between C3 and C6 cervical vertebra during maximal distention for bolus passage; PAhold = pharyngeal area holding the bolus in the mouth at rest; PAmax = pharyngeal area at maximum constriction
Risk factors predicting penetration and aspiration
Further analysis using a multiple stepwise logistic regression model demonstrated an elevated pharyngeal constriction ratio (if more than 0.0875, odds ratio = 5.2, chi-square = 5.8, p = 0.016, 95 per cent CI = 1.50–18.0), reduced pharyngoesophageal sphincter opening time (if less than 0.6 seconds, odds ratio = 11.6, chi-square = 14.0, p = 0.00018, 95 per cent CI = 3.02–44.2) and reduced airway closure time (if less than 0.6 seconds, odds ratio = 10.6, chi-square = 11.9, p = 0.00057, 95 per cent CI = 2.65–42.1) to be independent predictors of aspiration. Only elevated pharyngeal constriction ratio was significantly associated with penetration (if more than 0.075, odds ratio = 6.9, chi-square = 6.1, p = 0.014, 95 per cent CI = 1.68–28.4) without aspiration (Table 4). The expected cutoff point and odds ratio of each value are shown in Table 4.
Table 4. Risk factors predicting penetration and aspiration from multivariate analysis (logistic regression analysis) and receiver operating characteristic analysis

*n = 28; †n = 11; ‡n = 13; **if less than 0.075, odds ratio = 6.9, p = 0.014. PESopen = the duration of pharyngoesophageal sphincter opening; HLhold = distance from inferior hyoid bone to inferior cricoid cartilage or top of air column anteriorly that represents larynx–hyoid distance; Airway close = the duration from first firm contact of arytenoid-epiglottis to close the neoglottis to the point of airway re-opening” before the definition of PESopen.
Predicting factors related to radiation or arytenoids
In terms of pharyngeal constriction ratio measurement as a predicting factor, there was no statistical difference between one group with previous radiation history and the other without aspiration. Pharyngeal constriction ratio was statistically higher (worse) in the cases without radiation than in the radiated cases with laryngeal penetration. Airway closure duration and the pharyngoesophageal sphincter opening duration showed no statistical differences between the two groups in terms of penetration and aspiration (Table 5).
Table 5. Comparison between number of arytenoids in airway closure duration and between no irradiation and radiation failure in pharyngeal constriction ratio

*n = 11; †n = 13; ‡p = 0.009. PESopen = the duration of pharyngoesophageal sphincter opening
Discussion
Supracricoid laryngectomy with cricohyoidoepiglottopexy has been considered an effective technique for the treatment of selected laryngeal cancers because of preservation of physiological speech and swallowing function besides oncological safety. Some articles report that supracricoid laryngectomy with cricohyoidoepiglottopexy offers excellent functional results.Reference Nakayama, Laccourreye, Holsinger, Okamoto and Hayakawa2–Reference Nakayama, Yao, Nishiyama, Nagai, Ito and Yokobori7 However, swallowing impairment is still the most common functional problem following supracricoid laryngectomy with cricohyoidoepiglottopexy.Reference Naudo, Laccourreye, Weinstein, Hans, Laccourreye and Brasnu4,Reference Benito, Holsinger, Perez-Martin, Garcia, Weinstein and Laccourreye8 These studies were almost all about clinical outcomes of post-supracricoid laryngectomy deglutition with little analysis based on observations of neoglottis formation.Reference Alicandri-Ciufelli, Piccinini, Bergamini, Ruberto, Ghidini and Marchioni12 Therefore, our aim was to analyse videofluoroscopic swallowing studies to detect which factors lead to unfavourable events, such as laryngeal penetration or aspiration, after supracricoid laryngectomy with cricohyoidoepiglottopexy.
Generally speaking, videofluoroscopic swallowing studies are an ideal examination for identifying patients with post-operative aspiration because it provides both anatomical and physiological (dynamic) information for the evaluation of swallowing. The measurement method for videofluoroscopic swallowing study analysis published by Leonard and Kendall includes crucial elements likely to cast light on the minute mechanisms using values that are quantitative and reproducible for post-supracricoid laryngectomy dysphagia.Reference Kendall and Leonard13 Applying a standardised approach to the analysis of swallowing studies allowed us to perform reliable analyses to determine the differences between normal deglutition, laryngeal penetration and aspiration on the videofluoroscopic swallowing studies after supracricoid laryngectomy with cricohyoidoepiglottopexy.
Swallow gesture duration
In univariate and multivariate analysis of duration, it was shown that the durations of critical events such as pharyngoesophageal sphincter opening, airway closure and hypopharyngeal bolus transit time were shortened in those who aspirate. In particular, reduced pharyngoesophageal sphincter opening time and reduced airway closure time conferred the greatest risk of aspiration. In a previous study, pharyngoesophageal sphincter opening time was demonstrated to be prolonged after supracricoid laryngectomy with cricohyoidoepiglottopexy.Reference Yutomo, Shunsuke, Meijin and Taku14 We determined, however, that prolonged opening duration of the pharyngoesophageal sphincter relative to bolus transit was a compensatory mechanism in patients who did not aspirate following supracricoid laryngectomy with cricohyoidoepiglottopexy. Pharyngoesophageal sphincter opening duration in these patients was 0.68 seconds and declined to 0.53 seconds in patients who aspirated. However, pharyngoesophageal sphincter opening duration in patients who aspirate was as long as that in healthy volunteers at 0.50 seconds,Reference Kendall, McKenzie, Leonard, Goncalves and Walker15 whereas in terms of airway protection the airway closure duration of the post-supracricoid laryngectomy group was prolonged as a compensation to prevent bolus invasion into the airway.Reference Yutomo, Shunsuke, Meijin and Taku14
Similarly to pharyngoesophageal sphincter opening, the airway closure time in patients who aspirate, at 0.87 seconds, was as long as that in healthy volunteers at 0.85 seconds.Reference Kendall, McKenzie, Leonard, Goncalves and Walker15 These findings appear to indicate that the supracricoid laryngectomy with cricohyoidoepiglottopexy procedure can make patients enhance their airway protection and relaxation of pharyngoesophageal sphincter. Furthermore, it is necessary for post-supracricoid laryngectomy patients to prolong pharyngoesophageal sphincter opening and prolong airway closure to maintain sufficient deglutition. The number of preserved arytenoids has been reported to be significantly associated with swallowing outcomes in the short term.Reference Cho, Joo, Sun and Kim5,Reference Benito, Holsinger, Perez-Martin, Garcia, Weinstein and Laccourreye8,Reference Akbas and Demireller16,Reference Yüce, Çaglı, Bayram, Karasu, Satı and Güney17 Those with unilateral arytenoid may demonstrate worse neoglottic values than those with bilateral arytenoids. However, in our cohort, no differences were found in the durations of both airway closing and pharyngoesophageal sphincter opening.
It is accepted that prolonged hypopharyngeal transit time results in aspiration in dysphagia patients.Reference Leonard and McKenzie18,Reference Leonard, Kendall, Johnson and McKenzie19 This principle seems not to apply to post-supracricoid laryngectomy cases because the hypopharyngeal transit time of aspiration patients became shorter than that of normal patients and there was no significant difference in multivariate analysis. This may be because, according to a previous study, airway closure needs to begin far earlier than in normal patients to achieve firm contact between the tongue base (preserved epiglottis) and the arytenoid for acceptance of the bolus. Again, this is to compensate for changes in laryngeal function in supracricoid laryngectomy with cricohyoidoepiglottopexy patients.Reference Yutomo, Shunsuke, Meijin and Taku14 For that reason, prolonged hypopharyngeal transit time is preferable to avoid aspiration in post-supracricoid laryngectomy patients.
Swallow gesture displacement
It is interesting that no critical displacements, except for pharyngeal constriction ratio, deteriorated in patients who have laryngeal penetration or aspiration. Obviously, presentation of the characteristic that no displacements worsen is one of the great advantages of supracricoid laryngectomy with cricohyoidoepiglottopexy over other modalities, especially compared with radiotherapy where the pharyngeal constriction ratio deteriorates markedly, reflecting severe pharyngeal weakness. Only enlarged pharyngeal constriction ratio, which is associated with the presence of aspiration as reported by Leonard et al.Reference Leonard, Rees, Belafsky and Allen20 and Yip et al.Reference Yip, Leonard and Belafsky21 could lead to both penetration and aspiration.
With regard to penetration, when constriction of the pharyngeal space is not sufficient the residue mainly causes penetration, although patients could cough out a small amount of bolus invasion. Meanwhile, aspiration occurred when the bolus head reached the neoglottis before the neoglottis closed. From the lateral view morphology, the tongue base (attached to the epiglottis) contributed to narrowing of the pharyngeal space besides the constriction of pharyngeal posterior wall, almost simultaneously closing off the supraglottic portion. This means that patients who demonstrate elevated (deteriorated) pharyngeal constriction ratio with aspiration are likely to have insufficient neoglottis closure. This seems to be because the arytenoid cartilages sitting on the cricoid cartilage are already located in an elevated position because of the cricohyoidoepiglottopexy procedure removing the entire thyroid cartilage; the tongue base movement to the posterior direction can make the pharynx constrict and more directly make the airway close than in healthy cases.
It is well known that radiation therapy to the head and neck region damages the construction organs to some extent. The most frequent types of damage inducing elevated pharyngeal constriction ratio are: (1) pharyngeal hypocontractility and (2) reduced base of tongue impaction with the posterior pharyngeal wall primarily because of neuromuscular fibrosis and radiation-induced oedema.Reference Logemann, Rademaker, Pauloski, Lazarus, Mittal and Brockstein22 Although the radiation field for laryngeal cancer is relatively limited, pharyngeal constriction ratio impairment can still occur. In the current study, we divided the videofluoroscopic swallowing study patients into two groups: with or without previous radiation treatment. As a result, there was no difference in the cohort who aspirate. Unexpectedly, the radiated group exhibited superiority to the previously untreated group with laryngeal penetration. These results suggest that radiation-induced pharyngeal dysfunction in laryngeal cancer might be compensated for by the supracricoid laryngectomy with cricohyoidoepiglottopexy procedure. Moreover, this fact confirmed previous reports indicating that previous radiation history did not influence swallowing function after supracricoid laryngectomy with cricohyoidoepiglottopexy.Reference Nakayama, Laccourreye, Holsinger, Okamoto and Hayakawa2,Reference Pellini, Manciocco and Spriano23,Reference Marioni, Marchese-Ragona, Pastore and Staffieri24
Swallowing treatments
This study focused on the predicting factors that imply possible anti-aspiration remedies, such as surgical procedures and evidence-based rehabilitation. If patients demonstrate a duration of airway closure time of less than 0.8 seconds on videofluoroscopic swallowing study, the risk of aspiration is approximately 10 times as high as in normal patients. Thus, first of all, it is also crucial to adjust the food viscosity to slow down the bolus flow during the first stage of rehabilitation to prevent pulmonary complications. Rehabilitation may be directed toward manoeuvres and exercises that improve anterior to posterior tongue movement, for instance supraglottic swallowing and effortful swallowing. In cases of shortened pharyngoesophageal sphincter opening duration, which is less than 0.6 seconds, the possibility of aspiration is more than 10 times higher than in normal patients. Procedures directed at the pharyngoesophageal sphincter may assist in preventing aspiration. Options for such interventions include pharyngeal dilatation, botulinum toxin and myotomy. Allen et al. reported that pharyngoesophageal sphincter opening improved more with cricopharyngeal myotomy than with dilatation.Reference Allen, White, Leonard and Belafsky25 Conservative treatment seems to be useful for post-supracricoid laryngectomy patients because they do not have severe pharyngoesophageal sphincter dysfunction. Allen et al. reported that even the mean maximal opening value of the pharyngoesophageal sphincter after conservative treatments was as wide as that of normal patients after supracricoid laryngectomy with cricohyoidoepiglottopexy. If dilatation were not effective, endoscopic or open myotomy could be considered.
Ideally, the pharyngeal constriction ratio should be less than 0.09 seconds. However, swallowing treatment should focus on two significant facets: tongue movement (airway closure) and pharyngoesophageal sphincter opening. In patients demonstrating elevated pharyngeal constriction ratio and aspiration, treatment to enhance airway closure could improve both aspiration and pharyngeal constriction. In patients demonstrating elevated pharyngeal constriction ratio and laryngeal penetration, procedures that prolong pharyngoesophageal sphincter opening duration may reduce penetration by facilitating bolus transit. Chin tuck swallows can compensate for deteriorated pharyngeal constriction by reducing the pharyngeal area.
Overall, it is possible to tailor a deglutition treatment strategy to compensate for post-surgical effects if post-supracricoid laryngectomy patients have insufficient swallowing function by taking advantage of the videofluoroscopic swallowing study measurements.
Limitations of study
The present study was basically focused on durations and displacements. Consequently, we did not evaluate how strongly the airway was closed. In other words, it is possible that aspiration was caused not only by timing failure but also weakness of neoglottic closure, such as insufficient arytenoid volume or neoglottis anomaly. Although pre-operative data are a predictor of post-operative swallowing function, this study does not include many descriptions of the pre-operative period. However, in principle, this procedure targets patients who are approximately 70 years old or younger at the time of surgery, with all patients eating regular food without any problems, so it can be said that this is a relatively homogeneous target group.
The results may have been affected by limiting the patients to those who could swallow a 20 cc bolus from a cup, to maintain measurement consistency. However, as a detailed comparative analysis of the swallowing manoeuvres in the post-operative state, we believe the current study offers valuable information for the successful management of post-supracricoid laryngectomy patients. Improved rehabilitation techniques can contribute to a safer and stable swallowing function.
• This study is the first analysis of factors predicting aspiration after supracricoid laryngectomy with cricohyoidoepiglottopexy by videofluoroscopic swallowing study
• Digital analysis of videofluoroscopic swallowing study included measurements of displacement and timing related to swallowing safety
• Shortened airway closure time, shortened pharyngeal pharyngoesophageal sphincter opening time and deteriorated pharyngeal constriction were identified as predicting factors
• Not all critical displacements deteriorated after supracricoid laryngectomy with cricohyoidoepiglottopexy
• Swallowing treatments can be tailored to the patient based on measurement analysis of videofluoroscopic swallowing study to improve swallowing safety
All cutoff points were detected considering receiver operating characteristic curve and other statistical data comprehensively. However, it is possible that the number of patients was insufficient in view of detecting factors predicting post-operative complications.
Conclusion
Supracricoid laryngectomy with cricohyoidoepiglottopexy can achieve control of advanced stage laryngeal neoplasms and sufficient laryngeal function. One of the greatest post-operative complications is aspiration. This study is the first analysis of factors predicting aspiration as assessed by videofluoroscopic swallowing study after supracricoid laryngectomy with cricohyoidoepiglottopexy. Although we identified shortened airway closure time, shortened pharyngoesophageal sphincter opening time and elevated pharyngeal constriction ratio as predicting factors, we also noted that not all critical displacements deteriorated after supracricoid laryngectomy with cricohyoidoepiglottopexy. Swallowing treatments can be tailored to the patient based on measurement analysis of videofluoroscopic swallowing study to improve swallowing safety.
Competing interests
None declared









