Historical Background
Twenty-five years ago, world policy makers began to formalize relationships between health, sustainable development, and disaster management and began to implement this alignment within international strategies for risk management. 1 The outputs of these meetings (furthered by subsequent development of international standards for risk management) have since contributed to a global doctrine for disaster risk management for all sectors, including health. 2 Table 1 1 , 3 - 9 lists key events in the development of international policies for managing disaster-related health risk according to a comprehensive approach.
Disaster Risk Management
Risk
Risk can be viewed as a representation of the degree of uncertainty involving the interaction between an event and its outcome. Uncertainty adversely effects ability to predict the risk of outcome.
Management
Processes that decrease the degree of uncertainty among activities are known to improve the likelihood of accomplishing the outcome (or objective). Management is a process used to reduce the uncertainty of outcomes through organization and coordination of the activities intended to achieve defined objectives.
Process Management
A process is a set of activities that interact to achieve a result (or outcome). Process management is an approach based upon systems to measure and control processes to achieve an intended goal or outcome. Here, process is considered as an input which accomplishes an outcome. These outcomes are represented in terms of goals or objectives and are thus considered as outputs of the system. Similarly, risk management systems apply inputs (referred to as capacity) which accomplish an output (known as capability).
Table 2 illustrates the relationship between inputs used for risk management, process management, and performance management. The significance of these concepts is based upon the recognition that risk management activities (ie, risk assessment) are part of an integrated management system with measurable inputs and outputs that may be controlled for efficiency and effectiveness.
Table 2 A Comparison of Systems for Managing Process, Risk, and Performance

Risk Management
Risk management is activity directed toward assessing, controlling, and monitoring risks. In risk management, evidence on risk factors is collected and analyzed, contexts are assessed, and risk treatment measures are implemented using standard strategies. 2
Strategies for risk management include risk assessment and risk treatment measures. Risk assessment typically involves application of an analytical risk assessment used to guide the most cost-effective options for treatment of the risk.
These control measures include: avoiding the risk; reducing the negative effect of the risk; transferring the risk to another party; and accepting some or all of the consequences of a particular risk. ISO 31000 is a set of international standards relating to risk management as codified by the International Organization for Standardization (Geneva, Switzerland). 2
Disaster Risk Management
Disaster risk management applies the general principles of risk management to disasters. It is a comprehensive approach that entails developing and implementing strategies for the entire disaster life cycle, before and after hazard impact.Reference Keim 10 Disaster risk management includes pre-impact risk avoidance, reduction and transfer measures, as well as post-impact measures including risk transfer and risk retention.
Once risks have been identified and assessed, techniques to manage or “treat” the risk fall into one or more of these four major categories described in Table 3 Reference Dorfman 11 (note that that efficiency and cost effectiveness tend to decrease for strategies listed lower in the table).
Table 3 Four Strategies for Treating Disaster RiskReference Dorfman 11

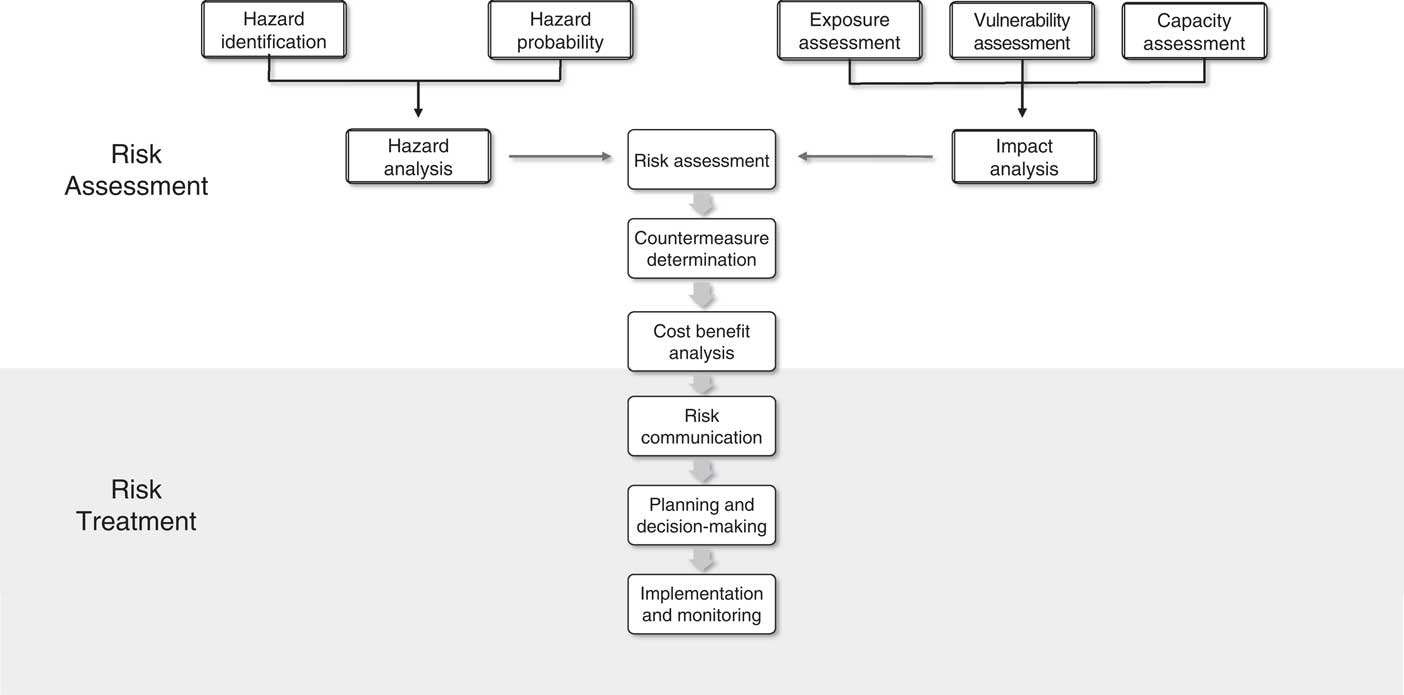
Figure 1 and Table 4 Reference Keim 12 , Reference Keim 13 describe the components of disaster risk management, in terms of risk assessment and risk treatment.

Figure 1 Schematic Overview of Disaster Risk Management Process.Reference Keim 10 , Reference Keim 12 , Reference Keim 13
Table 4 Key Components of Disaster Risk ManagementReference Keim 10 , Reference Keim 12 , Reference Keim 13

Natural History of Disaster-Related Disease
Natural History of Disease
The fundamental principle upon which disease management is based recognizes that development of any disease (which also includes injury) progresses through a natural history that can be broken into a series of stages. If left untreated, a disease will evolve through a series of stages that characterize its natural history. But if an intervention is applied, the natural history is modified to improve the outcome. Preventive measures can be applied at any stage along the natural history of a disease, with the goal of preventing further progression of the condition. 14
Figure 2 represents the “natural history of disease,” the concept of health and disaster-related disease as processes that unfold over time in a series of steps. Effective disease management requires management of the immediate problem, then of the patient’s risk factors, and finally, of the underlying determinants.
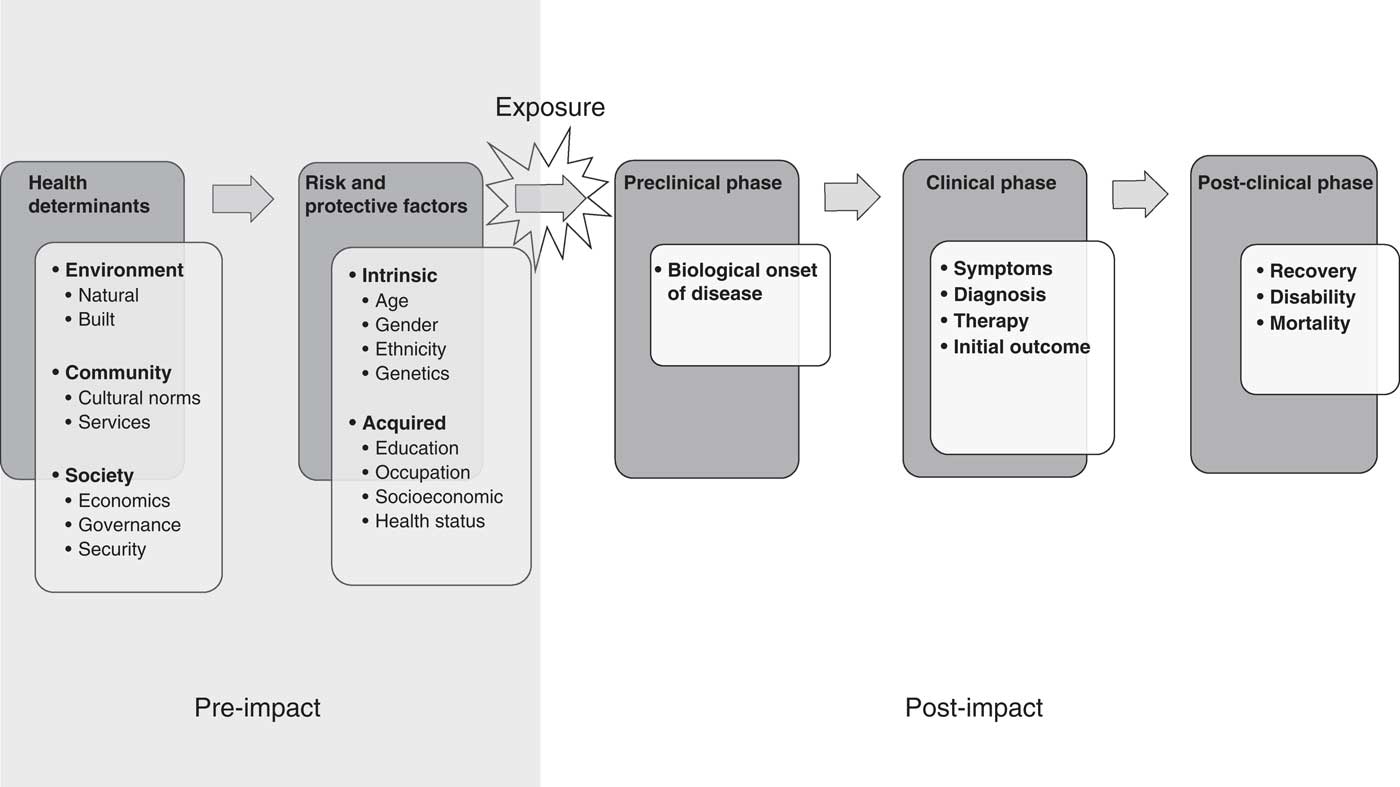
Figure 2 Natural History of Disease. 14
Casual Factors for Disease
Disease does not occur randomly. It is caused when vulnerable hosts are exposed to an environment containing agents that are hazardous to health. It is therefore possible to study the causal factors involving the agent, host, and environment, including both risk and protective factors. Figure 3 Reference Frost 15 illustrates how disease is caused by a complex interaction between the person (host), the disease agent (hazard), and the environment (exposure).
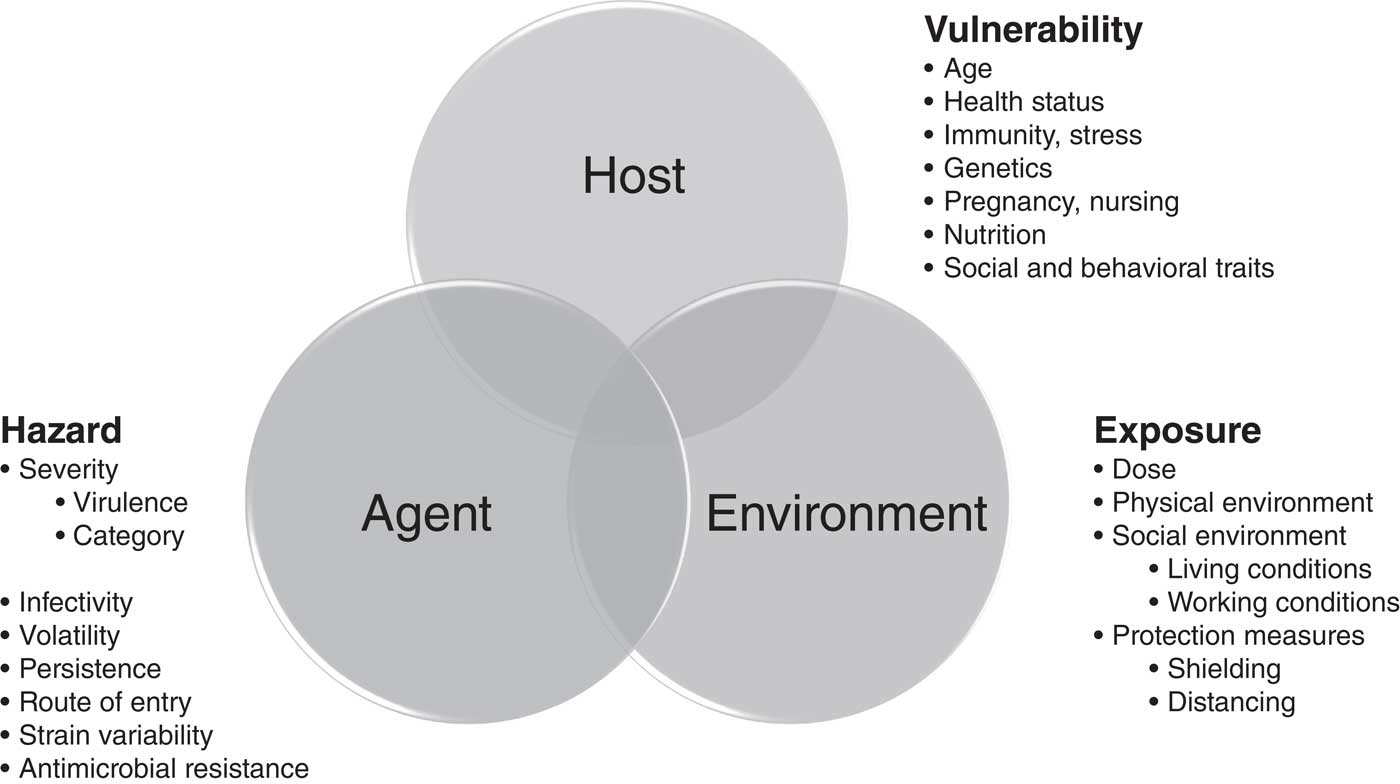
Figure 3 Causal Factors for Disease.Reference Frost 15
The Natural History of Disaster-Related Injuries
The time between exposure to the hazard and onset of disease (the “incubation period”) is of critical importance when prioritizing public health activities intended to reduce disaster-related mortality.
The period for developing a life-threatening injury is commonly measured in minutes to hours, whereas this period for outbreaks of disease is most commonly measured in days to weeks. This rapid onset of disaster-related injuries markedly limits the effectiveness of secondary and tertiary prevention (eg, response and recovery interventions). For example, the outcome of traumatic injuries is highly dependent upon the rapid availability of definitive surgical care within one hour from exposure (commonly known as the “golden hour” due to its valuable critical impact on survival outcome; Figure 4).

Figure 4 Natural History of Disaster-Related Injuries.
However, the character of most large-scale, environmental (eg, technological, hydro-meteorological, and geophysical) disasters commonly precludes accessibility of life-saving surgical care for the overwhelming majority of patients. This is of critical significance considering that 60% of the world’s disaster deaths during the past 50 years were due to injury caused by these same environmental hazards. 16
Thus, the natural history of disaster-related injuries often limits the effectiveness of secondary and tertiary prevention following disasters from technological, geophysical, and hydro-meteorological hazards, emphasizing the importance of primary prevention before the event occurs. On the other hand, the comparably slower onset and chronic nature of events caused by biological and societal hazards does allow more time for effective mortality reduction through secondary and tertiary prevention measures during response and recovery. In order to be effective in reducing mortality, health-related actions must be applied during the appropriate window of opportunity. It is important to recognize the value of a comprehensive approach to the prevention for disaster-related mortality.
Primary prevention of the exposure (before injury can occur) is therefore of critical importance to reducing mortality risk from these environmental hazards. In outbreaks and societal disasters, there is frequently more time available to allow for effective clinical and public health intervention before significant disease, disability, or death occurs.
Disease Prevention
Disease prevention includes a wide range of activities aimed at reducing health risks and improving health outcomes. Prevention occurs in four main stages: primordial, primary, secondary, and tertiary. 14 Primordial prevention involves preventing health hazards from occurring. Primary prevention involves preventing exposure, given that hazards exist. Secondary prevention involves preventing disease, given exposure has occurred. Tertiary prevention involves preventing further progression (eg, prolonged impairment; permanent disability; or death) given that disease (including injury) has occurred.
Primordial prevention seeks to modify the fundamental health determinants (“the cause of the cause” of disease). Primary, secondary, and tertiary prevention seek to modify risk and protective factors. Primary prevention focuses on reducing risk factors for exposure to the disaster hazard. Secondary and tertiary prevention focus on reducing the risk factors for vulnerability to disease. Secondary prevention seeks to prevent disease by reducing disease susceptibility. Tertiary prevention seeks to prevent disability and death by reducing disease severity. Table 5 represents a model for integration of approaches for managing disease, disaster risk, and emergencies.
Table 5 Public Health Prevention as an Integrated Approach for Managing the Risk of Disease

Primordial Prevention
Primordial prevention involves preventing the hazard occurrence and thus avoiding the environmental, economic, health, social, behavioral, and cultural factors of vulnerability known to amplify the risk of disease. It addresses broad health determinants rather than preventing personal exposure to risk factors, which is the goal of primary prevention. 14 Primordial prevention seeks first to prevent the disaster hazard from ever occurring. For example, floodplain management in an area of frequent flooding may actually prevent future flood hazards altogether, and therefore aligns with the disaster risk management activity of hazard avoidance. In examples where the hazard cannot be prevented, primordial prevention may be used to guide developmental decisions that avoid placing critical infrastructure and human settlements within hazardous areas.
Primary Prevention
The adverse health effect of a hazard is often characterized by a dose-response relationship. Typically, as the degree of exposure to a health hazard increases, the adverse health effect appears in more of the population. In the case of natural and infectious disease disasters, the degree of exposure of a given population to the hazard (eg, extremes of wind, temperature, precipitation, seismicity, volcanism, or biological agent) has a direct relationship to the incidence and severity of adverse health outcomes. Persons receiving a higher dose (magnitude of exposure to the disaster hazard over time) of the hazardous agent have a higher risk for adverse health outcomes as compared with those less exposed.
Primary prevention involves preventing exposures that would lead to disease. The goal of primary prevention is to prevent population exposure to risk factors.Reference Keim, Abrahams and Castilla-Echenique 17 It involves an interdisciplinary approach for identifying, characterizing, monitoring, and avoiding exposure to human health hazards. This includes those investigational aspects (like monitoring, forecasting, modeling, and dose reconstruction), as well as structural (eg, engineering controls, construction methods, and architectural design) and nonstructural (eg, public policy, education, and population protection measures) means for reducing exposures.Reference Keim 12
Secondary Prevention
The goal of secondary prevention is to prevent disease, given that exposure has already occurred.Reference Keim, Abrahams and Castilla-Echenique 17 These activities typically involve emergency response activities, such as search and rescue, mass-casualty response, disease control, and hazardous material response, that enable early diagnosis and appropriate management of disease. Disaster response is predominantly focused on immediate and short-term needs and is sometimes called “disaster relief.” Response usually includes those actions immediately necessary to remove the affected population from ongoing exposure or risk of harm. Effective response reduces adverse health impacts.
This element of risk retention accepts the risk of disease and seeks to prepare and respond to disease incidence with ameliorative and curative approaches. Risk retention involves accepting disaster loss when it occurs and then attempting to respond and recover (if possible). By default, all residual risks that are not avoided or transferred are retained and will require allocation of resources at some time in the future. Risk acceptance is not considered sustainable since the likelihood of future losses created by current developmental decisions is, in effect, being transferred to future generations for subsequently more expensive ad hoc emergency resource allocations.
Tertiary Prevention
The goal of tertiary prevention is to prevent the progression of impairment, disability, and death given that disease has occurred.Reference Keim, Abrahams and Castilla-Echenique 17 Tertiary prevention includes capabilities that reduce vulnerability as applied to disease severity, thus minimizing the risk of additional risk in the form of protracted illness, medical complications, disability, and death.
The capabilities involved in the tertiary prevention of disaster-related morbidity and mortality largely involve a network of curative health, rehabilitative health, communication, and social services intended to prevent additional or ongoing disability and death after the disease or injury occurs. This rehabilitation and recovery phase is characteristically long in duration and often an opportune time to initiate new aspects of primary prevention as the society attempts to “build back better” and reduce future risk.
Tertiary prevention of disaster risk involves measures taken during the recovery and rehabilitation phase as a component of risk retention. Recovery and rehabilitation begin soon after the emergency phase has ended, and should be based on pre-existing strategies and policies that facilitate clear institutional responsibilities for recovery action and enable public participation. The division between the response stage and the subsequent recovery stage is not clear-cut. Some response actions, such as the supply of temporary housing and health care, may extend well into the recovery stage.
Public health has systematically developed significant state, national, and international capabilities to address the effects of disasters (eg, mortality, morbidity, displacement, or loss of livelihood), but less so for addressing the root causes (hazards, exposures, and vulnerability). Figure 5 compares these root causes with the associated outcomes of disaster-related health effects.

Figure 5 Relationship between Causal Factors and Outcomes for Disaster-Related Health Risk.
Table 6 reveals the means by which disease prevention may be integrated to achieve the mutual goal of reducing disaster-related health risk. All stages of prevention begin with an assessment of the health risk. These data are collected from routine health surveillance as well as other disaster-specific outreach activities involving enhanced surveillance, needs, hazard characterization, risk analysis, and communication.
Table 6 Examples of Capabilities for Preventing Disaster-Related Health EffectsReference Keim, Abrahams and Castilla-Echenique 17 Abbreviations: PPE, personal protective equipment; WASH, water, sanitation, and hygiene.

Conclusion
Effective disaster risk management requires not only management of the immediate problem (disaster-related injuries and disease), but also of the patient’s risk factors and of the underlying health determinants. This requires the involvement of many sectors and disciplines which contribute to the management of health risks associated with emergencies and disasters. Disaster-related deaths are effectively reduced by health interventions and other measures that occur within a framework of: primary prevention (preventing hazards and exposures); secondary prevention (preventing injury or disease following exposure); and tertiary prevention (preventing disability and death following injury/disease).
The natural history of disaster-related injuries often limits the effectiveness of secondary and tertiary prevention following disasters from technological, geophysical, and hydro-meteorological hazards, emphasizing the importance of primary prevention before the event occurs. On the other hand, the relatively slower onset and often chronic nature of events caused by biological and societal hazards does allow more time for effective mortality reduction through secondary and tertiary prevention measures during response and recovery. In order to be effective in reducing mortality, health-related actions must be applied during the appropriate window of opportunity. It is important to recognize the value of a comprehensive approach to the prevention for disaster-related mortality.