Introduction
Cerebrospinal fluid (CSF) rhinorrhoea is a well documented entity. The value of endonasal repair of CSF fistulae is well established. With improvements in techniques and instrumentation, traditional external surgical approaches have largely been replaced by newer, endoscopic methods. These endoscopic approaches have the advantage of minimal invasiveness, good visualisation of the defect and shorter operating times.
However, superiorly and laterally placed defects in the posterior wall of the frontal sinus are not accessible via an endonasal endoscopic approach. Previously, such defects have been managed via an external osteoplastic flap, with obliteration of the sinus, cranialisation of the frontal sinus or simple closure, using neurosurgical approaches.
Here, we present a novel technique of endoscopic repair of such defects, involving two access holes drilled into the anterior wall of the frontal sinus, one for the endoscope and one for instruments. The defect is visualised directly via the endoscope introduced through one port, and the repair carried out with instruments passed through the other port. The external sinusotomy also allows insertion of Merocel® (Medtronic ENT, Jacksonville, Florida, USA) for graft support, together with a plastic sheet to prevent graft adherence to the Merocel. Both are removed through the nose after seven days.
This paper represents a preliminary report of this new technique.
Materials and methods
Between 2006 and 2010, nine patients were referred to us with frontal sinus CSF rhinorrhoea. All were referred with a diagnosis of CSF rhinorrhoea. Our diagnostic investigation included demonstration of CSF leakage, biochemical analysis of CSF for glucose and (in doubtful cases) β2 transferrin, and high resolution computed tomography. All the patients underwent a diagnostic nasal endoscopy during their first consultation to identify the site of leakage. Fluorescein studies were not used in any of the patients.
All procedures were performed under general anaesthesia with the patient in a supine position.
Firstly, all patients underwent an endonasal endoscopic Draf I, II or III type frontal sinusotomy, which is a prerequisite for our new technique since the graft supporting packs are delivered through these openings. Initially, a template of the frontal sinus was made using an occipito-frontal view X-ray plate. The outline of the frontal sinus was marked using the template.
Next, a 2 cm, curvilinear incision was made on the side of the leak. For medial defects, this incision was made above and as close as possible to the upper eyebrow, and medial to the supraorbital notch in order to prevent injury to the nerve; for lateral defects, a lateral eyebrow incision was used. The incision was deepened down to the bone. The periosteum was elevated above and below to expose the bone.
Using a 6 mm cutting burr, two ports were made in the frontal sinus anterior wall, separated by an island of bone (Figures 1 and 2). These bony ports could be bevelled for better access and angulation of instruments. One port served as the endoscope port and the other as the instrument port.
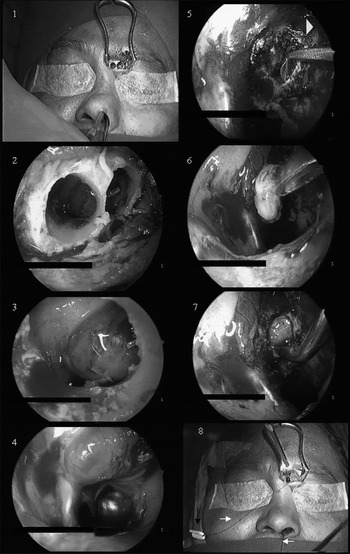
Fig. 1 Operative photographs showing surgical process.
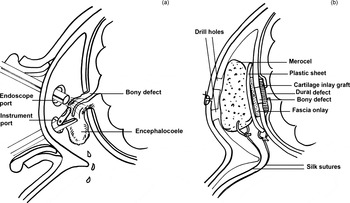
Fig. 2 Diagrams showing surgical technique.
The endoscope was introduced into the port closest to the site of the defect, and the site of leakage was identified (Figures 1 and 2). Usually, an encephalocoele, meningocoele or arachnoid cyst was identified, and removed either by debrider or by diathermy reduction and forceps removal.
Monopolar, insulated suction diathermy was used to cauterise the soft tissue in the vicinity of the bony defect, to delineate it. This step was essential to ascertain the size of the defect. The mucosa around the bony defect was also cauterised to a width of a few millimetres.
Fine micro-ear instruments were used to elevate the dura on the cranial side, to create a pocket for the cartilage graft.
Next, a piece of tragal cartilage was harvested along with its perichondrium. A piece of temporalis fascia was also harvested. The tragal cartilage was shaped such that it was slightly bigger than the defect size in at least two opposing dimensions. The cartilage was then folded and introduced into the frontal sinus via the instrument port, using forceps. When the cartilage graft was too large to be introduced through the sinusotomy opening, it was introduced intranasally into the sinus through the Draf type I, II or III sinusotomy. The cartilage was then tucked into the extradural pocket, using probes. This step was possible because of the flexibility of the cartilage. In large defects, multiple pieces of cartilage were used.
The temporalis fascia was then used as an onlay graft over the denuded area surrounding the defect. A layer of Surgicel® (Surgicel by Ethicon.inc, USA) was placed over the fascia graft. Two number eight catheters were fed through the instrument port into the frontal sinus, then into the nasal cavity through the intranasal sinusotomy, and brought out. An appropriately sized plastic sheet, cut away from the Merocel packing, was tied to one end of a 3-0 silk suture, and the other end of the suture was tied to one of the catheters. An appropriate piece of Merocel was cut, and another 3-0 silk suture was tied to one end, while the other end was tied to the second catheter. By pulling the catheters, the silk sutures were railroaded into the nasal cavity. First, the catheter to which the plastic sheet was tied was pulled until the sheet was inserted into the frontal sinus and placed over the Surgicel layer. Next, the Merocel was inserted into the frontal sinus by pulling the second catheter. Normal saline was instilled to expand the Merocel, and its position was adjusted.
The eyebrow wound was closed in layers. Skin closure was performed with 6-0 Ethilon sutures (Ethicon, Somerville, New Jersey, USA), for better cosmetic results. The two silk sutures were brought out of the nasal cavity and fixed over the ala with Micropore tape (Micropore tape by 3M, St. Paul, USA). The ethmoid cavity was packed with Merocel.
Intravenous broad-spectrum antibiotics were commenced pre-operatively and continued for at least three days after surgery. Patients were made ambulant on the first post-operative day. They were warned and reassured about the possibility of CSF leakage for a few days post-operatively, before adherence of the grafts to the graft bed. We did not use intrathecal fluorescein, tissue glue or a lumbar drain in any of our cases. Patients were discharged after 72 hours.
Patients were seen in the out-patient department on the seventh post-operative day, and all packs were removed under local anaesthesia. Under endoscopic vision, the silk sutures were pulled, one by one, in a downward direction, and the Merocel and plastic sheet were delivered through the endonasal frontal sinusotomy. Intranasal pack removal was successful and without incident in all cases.
Results
A total of nine patients underwent endoscopic frontal sinusotomy and endoscopic repair of a CSF fistula in the posterior wall of the frontal sinus. Five patients were female and four male. Patients' ages ranged from 21 to 55 years.
The aetiology of these patients' CSF leaks is shown in Table I. Although our patients' CSF leaks were of mixed aetiology, five were post-traumatic and four were spontaneous.
Table I Patient data
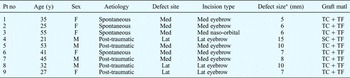
*Largest diameter. Pt no = patient number; y = years; matl = material; F = female; M = male; med = medial; lat = lateral; TC = tragal cartilage; TF = temporalis fascia; SC = septal cartilage
We encountered six medial defects and three lateral defects, which required six medial and three lateral external frontal sinusotomies. The largest frontal sinus posterior wall defect encountered measured approximately 1.5 × 1 cm (and greater than 1.5 cms along its greatest diameter).
Cerebrospinal fistula repair was successful in all patients, with no reported recurrences or complications at the time of writing. The duration of follow up ranged from three months to three years.
Discussion
Cerebrospinal fluid rhinorrhoea is caused by an abnormal communication between the subarachnoid space and the nasal cavity. Such fistulae can present at different sites in the nasal cavity, including the cribriform plate, lateral lamella, sphenoid sinus and frontal sinus.
In the frontal sinus, these defects are sometimes seen in the posterior wall, placed either medially, high up above the frontal floor, or in the lateral recess of the sinus.
These defects are not accessible via an endonasal endoscopic approach, mainly because angled telescopes are necessary for visualisation and longer curved instruments are required to reach the defect. Even then, an ‘end-on’ view of the defect is not possible. Despite the vast range of modern technology and instrumentation now available, these defects elude meaningful repair endonasally.
Traditional approaches to the frontal sinuses consist of osteoplastic flap and neurosurgical procedures. A coronal or brow incision and an osteoplastic flap technique with obliteration of the sinus are used.Reference Marshall, Jones, Gleeson, Jones, Burton, Clarke, Browning, Luxon, Lund, Hibbert and Watkinson1 This gives adequate exposure to the frontal sinus to enable repair of defects in the posterior wall, and even those placed laterally.Reference Marshall, Jones, Gleeson, Jones, Burton, Clarke, Browning, Luxon, Lund, Hibbert and Watkinson1 However, this procedure is associated with high rates of morbidity and recurrence, and sometimes causes alteration of the frontal contour, resulting in poor cosmesis.Reference Marshall, Jones, Gleeson, Jones, Burton, Clarke, Browning, Luxon, Lund, Hibbert and Watkinson1 In addition, it is a radical operation which obliterates sinus function. Needless to say, neurosurgical procedures are also associated with higher morbidity rates and occasional deformity.
Anterior frontal sinusotomy is synonymous with trephination.Reference Muntarbhorn, Thanaviratananich, Stamm and Draf2 Frontal trephination involves the use of a trephine to make a small hole in the anterior table of the frontal bone. Trephination can also be performed with a needle, trocar, chisel, gouge or drill. Drilling is the safest and most elegant way of producing a hole in the anterior wall of the frontal sinus. Although acute frontal sinusitis is the common indication for frontal trephination, it has also been employed in cases of chronic frontal sinusitis to widen the frontal outflow tract.Reference Muntarbhorn, Thanaviratananich, Stamm and Draf2
Our technique utilises two holes in the anterior wall of the frontal sinus, a few millimetres apart, to repair posterior table defects. No other reported technique has used such an arrangement, to our knowledge. A third hole may also be drilled, if a third hand is required in difficult situations.
The earliest report of frontal sinusotomy was by Ogston, who in 1884 described the ‘median anterior trephination of the frontal sinus through a median vertical incision’.Reference Ogston3 Schimidt (before 1895) and Silcock (in 1897)Reference Silcock4 reported using the eyebrow incision to perform trephination, in order to drain pus from the frontal sinus. Lothrop (1899)Reference Lothrop5 used an incision near the fronto-nasal suture and Kisch (1928) used a naso-orbital incision for frontal sinus trephination. Recent contributions to anterior frontal sinusotomy have come from Draf,Reference Draf and Draf6 Fry et al.,Reference Fry, Biggers and Fischer7 Wigand,Reference Wigand and Wigand8 Hoffmann and May,Reference Hoffman and May9 Gerber et al.,Reference Gerber, Myer and Prenger10 Muntarbhorn,Reference Muntarbhorn11 and Thawley and Deddens.Reference Thawley and Deddens12 All took advantage of the eyebrow as an incision site. The indication for surgery was mainly chronic sinusitis with obstruction of the frontal outflow tract. All these recent authors used one hole, varying in shape, to remove obstruction in the region of the frontal ostium. Drilling of the frontal beak has also been described via a frontal sinusotomy.Reference Muntarbhorn, Thanaviratananich, Stamm and Draf2
In contrast, our technique employs two holes in the anterior wall of the ipsilateral frontal sinus, created using eyebrow incisions, to repair posterior wall defects: one port for the endoscope and the other for instruments. We used a naso-orbital incision in one case, medial eyebrow incisions in five patients and lateral eyebrow incisions in three patients. An extradural cartilage inlay and temporalis fascia onlay technique was used in all cases. Tragal cartilage was used in eight cases and septal cartilage in one. Tragal cartilage proved to be a reliable graft material in our hands.
• The value of endoscopic endonasal repair of cerebrospinal fluid fistulae is well established
• Superiorly and laterally placed defects in the frontal sinus posterior wall are difficult to repair via an endonasal endoscopic approach
• A novel technique of endoscopic repair of such defects is described, involving access holes drilled into the anterior wall of the frontal sinus
• The defect is visualised directly with endoscopes through one port, and the repair conducted by passing instruments through the other port
• This technique of external frontal sinusotomy and endoscopic repair enables easy visualisation and precise repair, while preserving the normal sinus anatomy and function
There are several advantages of using this new technique for the management of frontal CSF fistulae. There is excellent visualisation of the defect, even when it is laterally placed. Depending on the position of the defect, the ports can be placed so as to enable an end-on approach to the defect (via either medial or lateral sinusotomy). The margins of the defect can be delineated precisely, and the extradural pocket is created by direct endoscopic vision. We believe that complete separation of the cranial soft tissues from the soft tissues of the frontal sinus, with placement of a cartilage graft between the two, is the key to successful repair. The cartilage is placed in an underlay fashion in the extradural pocket. The flexibility of the cartilage is utilised to manoeuvre it into place. Perhaps the most important advantages of our technique are preservation of normal sinus function and a reduced incidence of cosmetic deformities, post-operatively. In our experience, eyebrow incisions produce acceptable cosmetic results.
Draf I or III intranasal drainage is mandatory in all cases, since the graft support is removed through intranasal sinusotomy after seven days. Removal of graft support was achieved without incident in all our cases. We have been using a plastic sheet between the fascia graft and the Merocel for many years. This prevents the Merocel from adhering to the fascia, and is removed after seven days.
To the best of our knowledge, such an approach to the repair of CSF leakage from the frontal sinus posterior wall has not previously been reported.
Conclusion
The management of frontal sinus CSF fistulae presents a unique challenge. Traditional external approaches have now given way to endoscopic techniques. Laterally placed frontal sinus leaks are sometimes difficult to approach endoscopically, and may necessitate an external osteoplastic approach or neurosurgical procedure.
We believe that our new technique of external frontal sinusotomy plus endoscopic repair of the frontal sinus posterior wall defect offers distinct advantages, in that the normal anatomy and function of the sinus are preserved. The technique enables an end-on view of the defect, making the procedure precise and simple.
The obvious disadvantage of our technique is the facial scar, but this is well concealed if placed close to the eyebrow. This minor cosmetic disadvantage should not deter the surgeon from creating a solid, reliable repair of a potentially dangerous condition.
Our initial experience of using external frontal sinusotomy for the repair of frontal sinus posterior wall defects has been encouraging, and the technique has the potential to be extended to the other lesions of the frontal sinus.
This simple technique enables repair of frontal sinus posterior wall defects to fall within the purview of otolaryngologists.
To the best of our knowledge, this report represents the first description of this procedure.





