Introduction
Acute mastoiditis is the most common severe complication of acute otitis media in children, with an incidence ranging from 1.2 to 6.1 per 100 000 children.Reference Groth, Enoksson, Hultcrantz, Stalfors, Stenfeldt and Hermansson1 Although there has been a significant reduction in the incidence of acute mastoiditis since the introduction of antibiotics, its frequency has remained stable over the last decades.Reference House2–Reference Bahadori, Schwartz and Ziai4 Moreover, this stability persists despite the introduction of pneumococcal immunisation in the standard care of children in several countries.Reference Tawfik, Ishman, Tabangin, Altaye, Meinzen-Derr and Choo5
A blockage of the aditus ad antrum is the first step in the pathogenesis of acute mastoiditis, which is common for all ages. This blockage results in the trapping of serous exudate in the mastoid air cells and, in turn, pus formation, which can spread to the periosteum, causing periostitis. Contrary to older children and adults, the antrum in neonates and young infants is the only existent air cell, given that the mastoid cell system has not yet developed.Reference Niv, Nash, Slovik, Fliss, Kaplan and Leibovitz6 Should the infection progress, it can lead to cortical bone erosion and subperiosteal abscess formation (Figure 1).Reference Fliss, Leiberman and Dagan7 Untreated acute mastoiditis, with or without a subperiosteal abscess, can cause serious, life-threatening complications, such as meningitis, epidural or intracranial abscesses, and sigmoid sinus thrombosis.

Fig. 1. Axial (a) and coronal (b) contrast-enhanced computed tomography scans of a four-month old infant, which demonstrate a well-formed post-auricular abscess (white arrows). The infection has spread through a breakdown of the lateral mastoid cortex (outlined arrows). Note the complete lack of pneumatisation of the mastoid cell system at this age, bilaterally (arrowheads).
Our standard approach with older children suffering from acute mastoiditis includes parenteral antibiotics and myringotomy in all cases. The initial surgical approach also involves drainage or simple mastoidectomy when a subperiosteal abscess is present, while simple mastoidectomy is mandatory when intracranial complications are suspected.Reference Psarommatis, Voudouris, Douros, Giannakopoulos, Bairamis and Carabinos8
Acute mastoiditis is very rare in neonates and young infants, and few studies concerning this age group have been published.Reference Niv, Nash, Slovik, Fliss, Kaplan and Leibovitz6 This study aimed to investigate the epidemiological and clinical features of acute mastoiditis in neonates and infants aged six months or less. Our approach to diagnosis, imaging and treatment of this particular group is described and compared with corresponding data from older children.
Materials and methods
A retrospective review was performed of the medical records for all infants aged six months or less who were admitted to our department with the diagnosis of acute mastoiditis from January 2007 to December 2017.
The patients’ medical charts were reviewed, and data concerning the children's age, gender, history of middle-ear infections and antibiotic taking, clinical presentation, laboratory and imaging findings, medical and surgical treatment, microbiology, and final outcomes were manually collected and analysed.
The diagnosis of acute mastoiditis was based on clinical manifestations, including patients’ recent history of symptoms or signs of acute otitis media, accompanied by retroauricular inflammatory signs such as erythema, swelling, pain and/or antero-inferior protrusion of the auricle. Measurements of white blood cell count and differential, C-reactive protein, and erythrocyte sedimentation rate (ESR) were obtained upon patients’ admission. Imaging studies were not routinely performed. Contrast-enhanced computed tomography (CT), with or without brain magnetic resonance imaging (MRI), was conducted only in cases where an intracranial complication was suspected.
All children were treated with intravenous (IV) antibiotics in association with a wide myringotomy. Pus samples of the middle-ear effusion were obtained, and sent for culture and antimicrobial susceptibility testing. Myringotomy was performed, even in children presenting with purulent discharge on admission. Needle aspiration of the post-auricular area was also performed in all cases. Management of subperiosteal abscess included either drainage or antrotomy; the decision was made by the attending physician. In cases where an intracranial complication was suspected (i.e. focal neurological signs or symptoms, cranial nerve involvement, persistent high spiking fever), imaging studies were conducted as soon as possible. Depending on the findings, mastoidectomy was performed when necessary. All children were closely monitored on a daily basis.
Initial treatment was considered successful if, within 2–3 days, the following were observed: progressive restoration of the post-auricular inflammatory signs and auricular protrusion; partial or full restoration of the laboratory inflammatory markers; and the absence of fever. Improvements in all three parameters are essential to deem the treatment successful. In cases of no improvement in clinical or laboratory findings, further surgical treatment, such as antrotomy, was performed.
The R open-source software was used for statistical analysis of quantitative and qualitative variables.
Results
Epidemiology
During a 10-year period, 11 young infants aged 6 months or less, suffering from acute mastoiditis, were identified and included in our study. The group comprised six males and five females. The youngest was 2 months old, while the mean age of the group was 4.7 months.
History
No predisposing factors or conditions were identified. None of the infants were premature or suffered from any disease or syndrome. One of the infants had previously been admitted to the neonate intensive care unit because of jaundice. None of the patients had a previous history of middle-ear infections or had been subjected to any prior ear surgery. Five children (45.5 per cent) did not have any symptoms prior to the episode of acute mastoiditis, while four were suffering from bronchiolitis (36.3 per cent), one from an upper respiratory tract infection for three weeks and one from gastroenteritis.
Presentation
On admission, all 11 children had had obvious signs and symptoms of acute mastoiditis for 12–48 hours (mean = 37.1 hours, interquartile range = 24 hours). All of them had a protruding ear associated with erythema, tenderness and swelling of the mastoid area. In eight children (72.7 per cent), a subperiosteal abscess had already formed on admission. The right mastoid was affected in seven patients (63.6 per cent), and the left mastoid was affected in four patients (36.3 per cent). Seven children had ipsilateral otoscopic signs of acute otitis media and four were suffering from bilateral acute otitis media.
Post-auricular symptomatology was, in most cases, associated with fever (n = 7, 63.6 per cent). Irritability was present in five patients (45.5 per cent), and one patient had shown decreased food intake; two patients had no symptoms other than the clinical signs of retroauricular inflammation. In addition to the post-auricular findings, the presence of persistent high spiking fever in two cases and the toxic appearance in one case raised the suspicion of an intracranial complication.
Laboratory findings
The complete blood count revealed a significant increase in the white blood cell count in all cases (mean = 20.782 cells/μl, interquartile range = 7300 cells/μl). The C-reactive protein levels showed a bigger range, varying between 6 mg/l and 261 mg/l (mean = 79.2 mg/l, interquartile range = 93.7 mg/l). The ESR was measured in eight children, and the average value was 77.7 mm in the 1st hour (interquartile range = 70 mm/hour).
A temporal bone CT scan was performed in three patients, as an intracranial complication was suspected. One of the patients also underwent magnetic resonance venography, because sigmoid sinus thrombosis was suspected based on the CT scan. Another child was subjected to MRI, 6 days after surgery, because of an episode of temporary loss of consciousness. Intracranial complications were not diagnosed in any of the aforementioned cases.
Treatment
All patients were initially treated with empirical IV antibiotics. They all received a combination of cefotaxime and clindamycin. Antipyretics and analgesics were administered according to the individualised needs of each case.
The surgical treatment included myringotomy (seven ipsilateral, four bilateral) and ipsilateral needle aspiration of the post-auricular area, performed under general anaesthesia, in all children within the first hours after admission. Moreover, of the children with a subperiosteal abscess, four (36.4 per cent) were treated with incisional drainage of the abscess and four (36.4 per cent) underwent antrotomy. The average time that elapsed from diagnosis to surgery was 11.6 hours. An infant who was initially treated with IV antibiotics and bilateral myringotomy eventually underwent antrotomy, 3 days later, because no clinical improvement was observed (Figure 2).
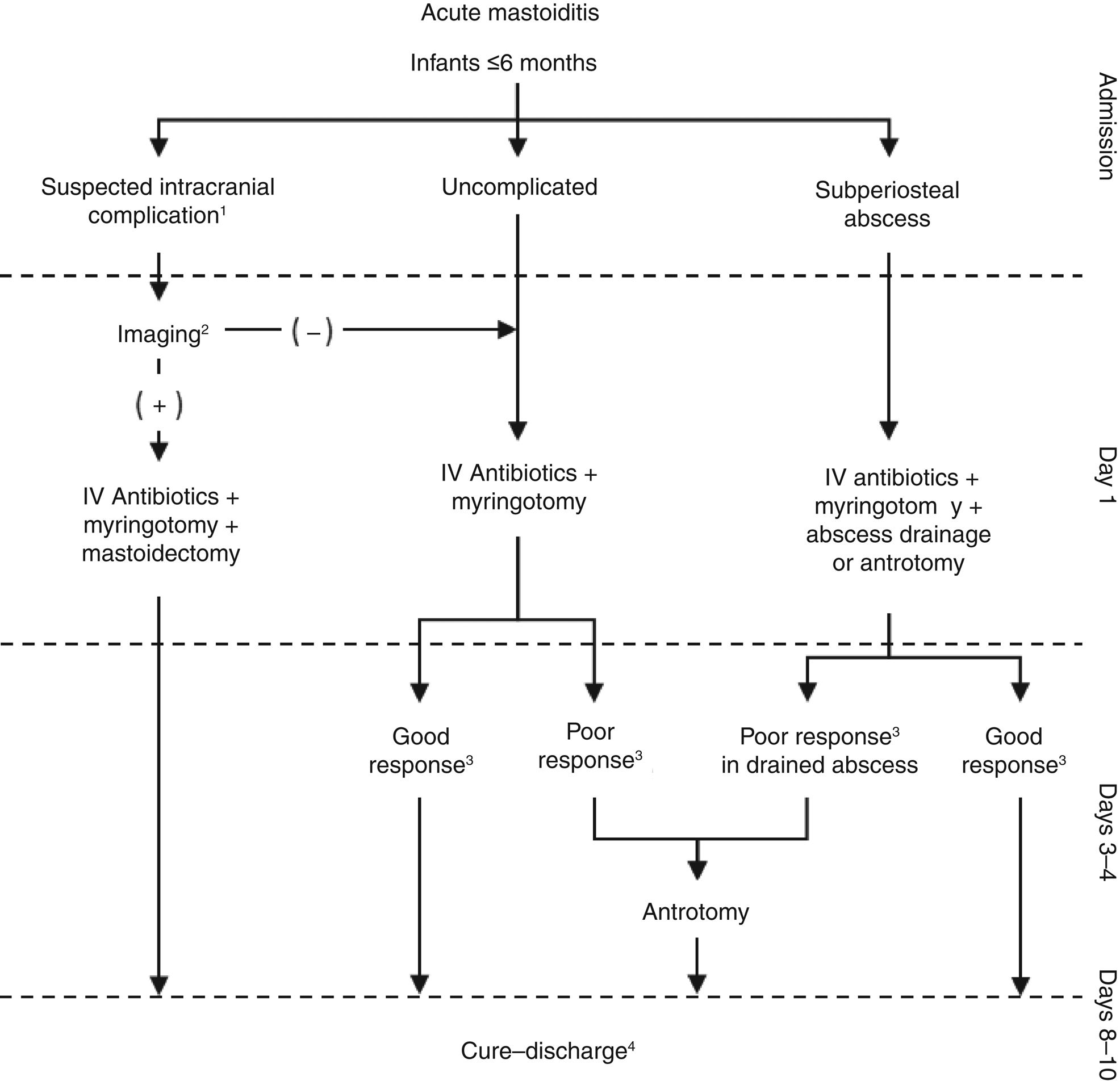
Fig. 2. Suggested algorithmic management pathway for acute mastoiditis for infants aged six months or less. Notes: 1. Focal neurological signs or symptoms, cranial nerve involvement, high spiking fever, vomiting, papilloedema, altered mental state, toxic appearance. 2. Contrast-enhanced computed tomography; magnetic resonance imaging and magnetic resonance venography may be needed. 3. Using clinical and laboratory criteria. 4. For infants with intracranial complications, longer in-hospital treatment is required.
Microbiology
Culture results were positive in 10 out of 11 specimens (90.9 per cent). The two most commonly found bacteria were Streptococcus pneumoniae (5 infants; 45.5 per cent) and penicillin-sensitive Streptococcus pyogenes (4 infants; 36.3 per cent). All S pneumoniae strains isolated were susceptible to penicillin, except in one case, wherein the S pneumoniae strain isolated proved to be resistant to penicillin but susceptible to cefotaxime. In two cases, more than one pathogen was detected; in the first case, penicillin-sensitive Haemophilus influenzae and S pneumoniae were identified, while in the second, penicillin-sensitive H influenzae and coagulase-negative staphylococcus were detected.
Final outcome
All patients were fully cured and discharged after an average hospitalisation of 9.3 days. All children took oral antibiotics for one more week after discharge (amoxicillin/clavulanate in 10 cases, and clarithromycin in 1 case).
The mortality rate in the study population was null. None of the infants developed any additional in-hospital acquired complications while under treatment, due to either the disease itself or the surgery. Repetition of either myringotomy or mastoidectomy was not deemed necessary in any of the cases. No recurrences shortly after discharge, requiring re-admission, were recorded either. After an average follow up of 18 months, no short-term or long-term complications or sequelae were observed.
Eight of the children did not develop further middle-ear infections within the follow-up period. One patient suffered from an episode of acute otitis media in the contralateral ear, while one presented with acute otitis media in the previously affected ear. Lastly, one infant suffered a recurrent acute mastoiditis ipsilaterally, four months later, which was apparently unrelated to the first episode.
Discussion
Acute mastoiditis still remains a relatively frequent disease among the paediatric population, which, if untreated or mishandled, can lead to severe and life-threatening complications. Numerous studies on paediatric acute mastoiditis can be found in literature, while currently there is no consensus regarding the proper management options or treatment protocols.Reference Anne, Schwartz, Ishman, Cohen and Hopkins9,Reference Loh, Phua and Shaw10
To the best of our knowledge, there is only one study concerning acute mastoiditis exclusively in infants aged under six months, to which our results can be compared.Reference Stenfeldt, Enoksson, Stalfors, Hultcrantz, Hermansson and Groth11 The very young age of the patients, the variability in their general health status, the total lack of patient co-operation, the potential absence of specific symptomatology and the possible dominance of systemic symptoms, render the management of acute mastoiditis in this age group challenging. Even experienced otolaryngologists may feel uncomfortable when dealing with this pathology in neonates and infants aged six months or less.
Regarding the manifestation of the infection, all patients exhibited the typical signs and symptoms of acute mastoiditis. All the infants had post-auricular swelling, erythema and tenderness, as well as auricular protrusion, on admission, with no exceptions. Most of the patients had a fever, ranging from 37.8°C to 39.5°C (64 per cent), while some showed low food intake and irritability. Irritability is a common but non-specific symptom in this age group. Other symptoms and/or signs (i.e. lethargy, vomiting, bulging fontanelle and cranial nerve involvement) should be additionally exhibited before intracranial complications are considered.
The time needed for acute mastoiditis to develop, following acute otitis media, may be much shorter in young infants than in older children and adults, which is of clinical significance. This was observed not only in our series but in other studies as well.Reference Stenfeldt, Enoksson, Stalfors, Hultcrantz, Hermansson and Groth11–Reference Taylor and Berkowitz14 Additionally, the absence of previous middle-ear infection implies that the first episode of acute otitis media in the patients’ life led to acute mastoiditis.Reference Stenfeldt, Enoksson, Stalfors, Hultcrantz, Hermansson and Groth11,Reference Groth, Enoksson, Hermansson, Hultcrantz, Stalfors and Stenfeldt15 In contrast to older children, the absence of a positive otological history in young infants and neonates is the norm. Therefore, paediatricians and otolaryngologists should treat every single episode of middle-ear infection, even the first one, cautiously in this particular age group.
Regarding imaging, only 3 of the 11 children in this study underwent imaging investigations because of suspected intracranial complications.Reference Bales, Sobol, Wetmore and Elden16 In contrast to other studies, the need for antrotomy was not used as a criterion for performing CT or MRI.Reference Stenfeldt, Enoksson, Stalfors, Hultcrantz, Hermansson and Groth11,Reference Marom, Roth, Boaz, Shushan, Oron and Goldfarb17,Reference Chesney, Black and Choo18 The authors’ opinion is that in typical cases of acute mastoiditis in neonates and young infants, attending surgeons may refrain from any imaging study. However, they should adopt a low threshold in deciding to request a contrast-enhanced CT scan and/or MRI in cases of a suspected intracranial complication or a doubtful diagnosis.
A remarkable difference of acute mastoiditis in young infants, in comparison with older children, is illustrated by the significantly higher percentage of subperiosteal abscess formation on admission of the former. In a mixed paediatric population suffering from acute mastoiditis, Luntz et al.Reference Luntz, Brodsky, Nusem, Kronenberg, Keren and Migirov12 reported a 17 per cent rate of subperiosteal abscess present on admission, while Psarommatis et al.Reference Psarommatis, Voudouris, Douros, Giannakopoulos, Bairamis and Carabinos8 reported a 22 per cent rate. In the series under investigation, 73 per cent of the infants aged six months or less had a formed subperiosteal abscess on admission. A higher rate of subperiosteal abscess formation in infants aged six months or less with acute mastoiditis was found by Stenfeldt et al.Reference Stenfeldt, Enoksson, Stalfors, Hultcrantz, Hermansson and Groth11 as well.
The clinical examination establishes the diagnosis of subperiosteal abscess. The clinical criteria are those of acute mastoiditis (recent history of acute otitis media; retroauricular redness, swelling and pain; and antero-inferior displacement of the auricle), combined with retroauricular fluctuation and/or bulging of the posterosuperior wall of the external auditory canal.Reference Niv, Nash, Slovik, Fliss, Kaplan and Leibovitz6,Reference Psarommatis, Voudouris, Douros, Giannakopoulos, Bairamis and Carabinos8,Reference Stenfeldt, Enoksson, Stalfors, Hultcrantz, Hermansson and Groth11 The diagnosis of subperiosteal abscess can be enhanced by imaging findings. However, according to our approach, performing a temporal bone CT scan only for the purpose of establishing the diagnosis of subperiosteal abscess is not recommended. A diagnosis of subperiosteal abscess is definitively confirmed or rejected during surgery.
In recent years, we have adopted the approach of needle aspiration of the post-auricular area in all children with acute mastoiditis, either younger or older than six months.Reference Psarommatis, Voudouris, Douros, Giannakopoulos, Bairamis and Carabinos8,Reference Psarommatis, Giannakopoulos, Theodorou, Voudouris, Carabinos and Tsakanikos19 This approach has helped us diagnose subperiosteal abscess in cases of acute mastoiditis without palpable post-auricular fluctuation or posterior canal wall bulging, which otherwise would have remained undiagnosed. Regardless of the quantity, pus aspiration from the post-auricular area is a non-failing finding for subperiosteal abscess formation. In one case in this series, just 0.5 ml of clear pus was aspirated by the young infant, and it was cured without further surgery. We believe that carefully performed post-auricular aspiration in children suffering from acute mastoiditis is a very sensitive, simple, low-cost procedure for diagnosing subperiosteal abscess, with no complications or adverse effects. It can be safely added to the standard of care for all children suffering from acute mastoiditis, and can be performed in the same operating session as myringotomy.
All infants with acute mastoiditis in our series were given empirical IV antibiotics immediately upon admission. The combination of cefotaxime and clindamycin was used for all patients. This scheme theoretically covers almost the whole spectrum of micro-organisms known to be involved in acute mastoiditis. Furthermore, in our experience, it works very effectively in all paediatric ages. Regarding the microbiology of acute mastoiditis in infants aged six months or less, it appears to be quite similar to that of older children.Reference Groth, Enoksson, Hultcrantz, Stalfors, Stenfeldt and Hermansson1,Reference Psarommatis, Voudouris, Douros, Giannakopoulos, Bairamis and Carabinos8,Reference Psarommatis, Giannakopoulos, Theodorou, Voudouris, Carabinos and Tsakanikos19–Reference Benito and Gorricho21 S pneumoniae and S pyogenes were the most common pathogens in this series. Bacterial resistance was not a matter of concern in our population, given that four out of five S pneumoniae cases and all S pyogenes cases were found to be susceptible to penicillin.
Apart from the prompt antibiotic treatment, all young infants were subjected to a surgical intervention for pus pressure release within the first 12 hours of admission. Our decision-making regarding the treatment of acute mastoiditis took into consideration both the potential long-term risks of general anaesthesia as well as the potentially insufficient treatment of acute mastoiditis. In a large, multi-centre study of acute mastoiditis in paediatric patients where myringotomy was not systematically performed, an alarming rate of intracranial and intratemporal complications developed in-hospital (8.5 per cent of cases) has been reported.Reference Luntz, Brodsky, Nusem, Kronenberg, Keren and Migirov12 Regardless, the probability of developing such serious complications should be minimised.
Irrespective of the type of surgical procedure adopted, it is the authors’ opinion that early surgical intervention constitutes a key action in achieving satisfactory outcomes. Every infant in this study was subjected to an operation that assisted in the drainage of the pus from the middle-ear cleft, and in the obtainment of pus specimens for culture and susceptibility testing. Myringotomy alone was sufficient for two out of three young infants with uncomplicated acute mastoiditis. In one case, antrotomy was needed, and performed on the 3rd in-hospital day, because of a poor clinical response to treatment after 48 hours. Infants suffering from acute mastoiditis and subperiosteal abscess (n = 8) were subjected to myringotomy as well as an additional procedure to drain the abscess within the first 12 hours of admission. Four out of eight patients underwent antrotomy; the remaining four patients were drained either by needle aspiration or by post-auricular incision. Both subgroups had an uneventful post-operative period and a similar final outcome.
Concerning the terminology, we prefer the term ‘antrotomy’ instead of ‘simple mastoidectomy’, because the mastoid air cells have not been developed and essentially only the cavity of the antrum exists at this age (Figure 1). Basically, this is the main cavity which should be accessed; in most cases, no further intervention is required. Therefore, the term ‘antrotomy’ describes the surgical operation for acute mastoiditis in infants aged six months or less more precisely.
• Literature on the management of acute mastoiditis in infants aged six months or less is limited
• This age group shows the same presenting symptomatology as older children, but subperiosteal abscess formation rate is higher
• Imaging studies can be avoided in typical acute mastoiditis cases with or without subperiosteal abscess
• Contrast-enhanced computed tomography and/or magnetic resonance imaging can be reserved for suspected intracranial complications or when diagnosis is doubtful
• Initial surgical approaches should include parenteral antibiotics and wide myringotomy; antrotomy can be reserved for unresponsive cases after 3–4 days
• Abscess drainage or antrotomy should be included in the initial approach for those infants with subperiosteal abscess
A significant shortcoming of the present study is the limited population size. Investigation of a much larger number of neonates and infants suffering from acute mastoiditis is necessary to draw safer conclusions. However, based on the experience gained up to this point, the algorithm shown in Figure 2 seems to be both effective and safe. It is strongly suggested that this algorithm be used for all cases of acute mastoiditis in infants aged six months or less.
Conclusion
Throughout the study period, no mortality, in-hospital, short- or long-term complications or sequelae, revision myringotomies or mastoidectomies, or re-admissions were observed. Given the positive final outcomes of all patients, their management is deemed highly safe. Therefore, some practical conclusions regarding the management of acute mastoiditis in infants aged six months or less can be reached. First, infants aged six months or less share the same presenting symptomatology compared to older children. Second, a much higher rate of subperiosteal abscess formation is expected in young infants suffering from acute mastoiditis. Third, imaging studies can be avoided in typical cases of acute mastoiditis with or without subperiosteal abscess. Contrast-enhanced CT and/or MRI can be reserved for: those cases of suspected intracranial complications, recurring acute mastoiditis cases and patients with a non-typical manifestation when diagnosis is doubtful. Fourth, the management methods used for older children can be safely applied to neonates and infants aged six months or less. Medical and surgical measures should be promptly applied. These include: parenteral antibiotics and wide myringotomy in all cases, and additional abscess drainage or antrotomy for those infants with a subperiosteal abscess. Fifth, in uncomplicated acute mastoiditis patients, antrotomy can be reserved for non-responsive cases after 3–4 days.
Competing interests
None declared




