Introduction
Diabetes mellitus is reaching epidemic proportions in the United States and other industrialized nations.Reference Narayan, Boyle, Thompson, Sorensen and Williamson 1 Although a chronic disease, diabetes, and its medical treatment, also can cause acute, sudden symptoms that require emergency care. In these cases, emergency medical dispatchers (EMDs) must identify accurately diabetic-triggered events in order to ensure that patients receive the proper care and that Emergency Medical Services (EMS) system resources are allocated appropriately.
The Medical Priority Dispatch System (MPDS) is a protocol system employed in 42 countries by more than 53,000 certified members. Among 911 centers utilizing the MPDS, those using the MPDS software ProQA consistently report that 2%-3% of their total cases are assigned to the Diabetic Problems Chief Complaint.Reference Clawson, Dernocoeur and Rose 2 Most of the Chief Complaint protocols in the system are designed to handle specific signs and symptoms (eg, Breathing Problems or Chest Pain). The origin of the Diabetic Problems protocol represents a very different structural philosophy.Reference Clawson 3 Rather than addressing a specific symptom or incident type, the Diabetic Problems protocol is one of the few that is diagnosis-based. Callers usually are aware that a patient has a diabetic history and recognize the associated symptoms.Reference Clawson, Dernocoeur and Rose 4 As a result, many provide that information to the EMD as part of their description of the patient's signs and symptoms. Thus, it has been considered sound to assume that EMDs can rely on the caller's report of diabetic history or diabetic problems as a basis for selecting Diabetic Problems as the Chief Complaint.
However, despite the growing prevalence 5 and cost of diabetes, no published research exists on the soundness of this assumption. The ability of EMDs to initially identify other Chief Complaint conditions such as strokeReference Buck, Starkman and Eckstein 6 has been quantified and also linked to specific initial trigger words and clinical clues provided by the caller. Accurate identification of diabetic-triggered problems, versus those mimicking these problems, is similarly important since accurate EMD identification leads to appropriate EMS response and patient care.
The primary objective of this study is to determine the percentage of EMD-identified Diabetic Problems cases (using the MPDS Case Entry process) confirmed by EMS and/or hospital records as true diabetic-triggered events. The secondary objective is to establish whether 911 patients identified by EMDs as having diabetic problems actually have other medical conditions that may obscure the Chief Complaint selection process and be the actual primary cause of the emergency call.
Methods
Setting
This retrospective study was conducted in Salt Lake City, Utah USA and involved six hospitals. Salt Lake City had an urban/suburban resident population of 171,000 at the time of this study. The city utilizes a multi-tiered, combination EMS response system with seven paramedic engines and six emergency medical technician (EMT) engines, statically maintained. Salt Lake City also has private EMT ambulances positioned by computer-aided, dispatch-controlled system status management processes and peak-load staffing programs. All 911 calls are handled by certified Advanced EMDs at the Fire Department Emergency Communication Center.
This center has been an International Academies of Emergency Dispatch (IAED)-Accredited Center of Excellence since 1998—a best-practices designation that requires a minimum of either 90% or 95% compliance to various processes used within the MPDS protocols. The actual compliance rates during the study period were: 95.9% overall score, 97.9% for the Diabetic Problems protocol use, 100% for initially selecting the Diabetic Problems as the correct Chief Complaint, and 98.3% for the selection of all Chief Complaints. The data were collected using the MPDS version 11.0 (1999 release). The study was approved by the Institutional Review Boards of the six participating hospitals and by the Salt Lake City EMS/Inter-Hospital Council.
Outcome Measures
The primary endpoints or outcome measures in this study were: the percentage of cases that had a history of diabetes, percentage of EMD-identified Diabetic Problems cases that were confirmed by EMS and/or hospital records as true diabetic-triggered events, and the percentage of EMD-identified diabetic patients who also had other medical conditions.
EMD Diabetic Problems Identification
Emergency Medical Dispatchers assign cases to the Diabetic Problems protocol based on the primary assessment question, “What's the problem, tell me exactly what happened.” The most obvious way EMDs select the Diabetic Problems Chief Complaint protocol is for the caller to volunteer that the patient is known to be diabetic. However, callers may or may not provide specific diabetic history information. Instead, some callers may suggest a diabetic history without specifically stating that the patient is diabetic; for example, a caller rather than stating, “My dad's a diabetic,” may simply say that the patient's “blood sugar is low,” that the patient “has the sugar,” or that the patient “uses insulin.” Callers also may use more general terms, including references to fainting, dizziness, or weakness, which may obviously be more likely to complicate protocol selection. Further details on various dispatch case classifications are presented in Table 1.
Table 1 Definitions of Diabetes Severity Matrix

Diabetic-Triggered Events
The primary measure of a true diabetic-triggered event was the hospital (discharge/admit) diagnosis, whenever this was available. In some instances, the hospital diagnosis was not available—for example, when paramedics treated and resolved a hypoglycemic condition at the scene and the patient refused to go to the emergency department. In these cases, paramedic-run report information, particularly the paramedic-reported Chief Complaint and working diagnosis, were used to identify diabetic-triggered vs. non-diabetic-triggered events.
Paramedic-reported first and second blood glucose assessment measures also contributed to identification, along with paramedic-reported patient history and medications. However, blood glucose often changes rapidly during the course of an emergency diabetic event. Hence, the authors did not feel that blood glucose level alone was a sufficient and entirely reliable measure to define a true diabetic-triggered event. In addition, blood glucose is not known at the moment the caller reports the problem via 911, unless the caller volunteers that information (which appears to be very rare in the authors’ experience.) For these reasons, the more complete analysis of the total hospital and paramedic information was used to make this determination.
Case Reviews: Data Collection and Processing
The data were collected over a one-year period (2001), and the study sample included all calls assigned to the Diabetic Problems Chief Complaint protocol, irrespective of gender, age, etc. (Figure 1). Paramedic scene and hospital outcome data for these patients were also obtained. Using EMS patient care reports, emergency department care and admission records, and hospital charting and discharge records, each patient's record was examined to determine diabetic history, type of diabetes, and other medical conditions primarily involved (if applicable). Each case was then identified as either a diabetic-triggered event or a non-diabetic-triggered event. Using these data, each case was evaluated to determine whether the EMD's identification of the case as a diabetic problem was accurate. Two reviewers (a paramedic and a fourth-year medical student) performed the initial reviews independently. Where there was discordance, a third reviewer (ie, a senior EMS medical doctor) resolved the issue(s).
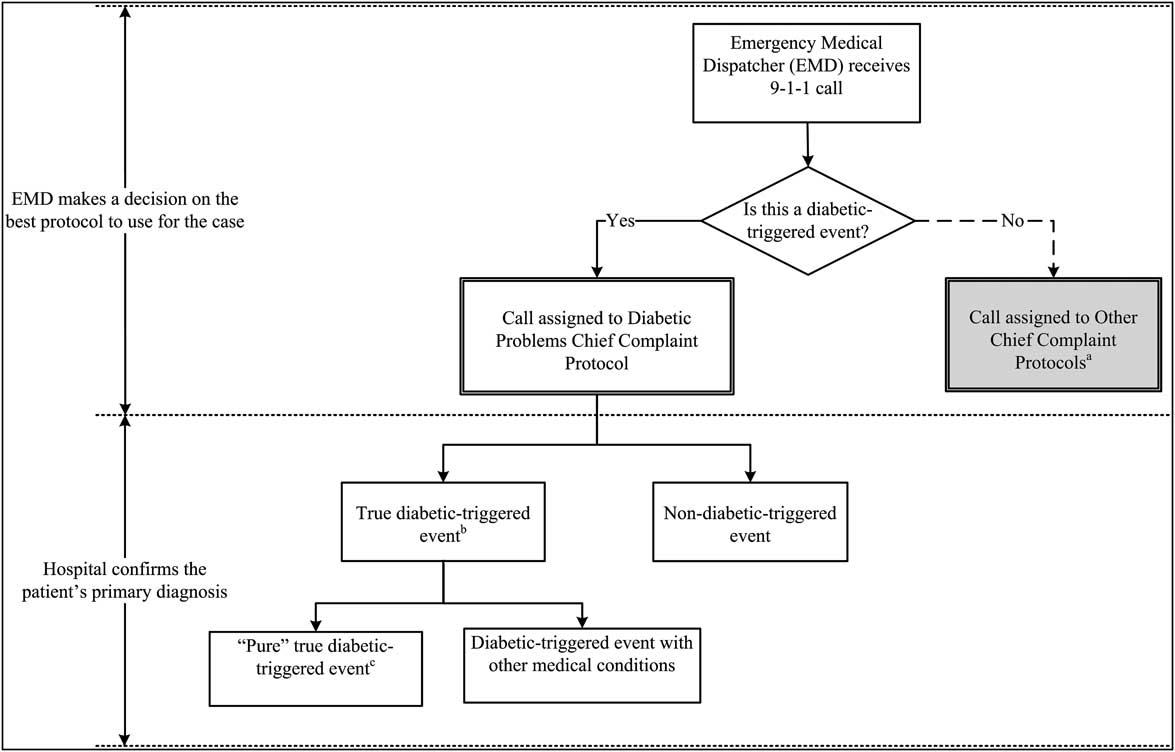
Figure 1 Study Sampling Process
aThese calls were excluded from the study sample.
bAn event in which the patient's emergency was directly caused by diabetes or its medical management.
cA true diabetic-triggered event in which the patient's emergency did not include/involve any other medical condition.
Paramedic scene and hospital outcome data were analyzed retrospectively to determine the true immediate cause of the emergency call. Patients were identified as having a diabetic-triggered event if the data confirmed that the EMD's assessment of the immediate reason for calling 911 was directly triggered by diabetes and its direct medical management (or lack thereof). The remaining patients were those whose immediate concern or symptom was determined not to have directly resulted from diabetes. These patients were identified as having a non-diabetic-triggered event. In other words, these patients’ emergent problems were determined to have been caused by medical problems other than diabetes, even if they had a documented diabetic history.
Data Analysis
STATA for Windows software (STATA Statistical Software: Release 11.2, StataCorp, College Station, Texas USA) was used for data analysis. Significance of the differences between study groups was assessed at a .05 significance level. Two-sided Fisher's Exact Test was used to assess the differences between various outcome measures in the categorical data. The cases were also profiled by patient age and MPDS determinant codes. Finally, the presence of, and differences between, diabetic history, diabetic-triggered events, and non-diabetic-triggered events were evaluated.
Results
A total of 393 patient cases were assigned to the Diabetic Problems Chief Complaint protocol. Of these, 14 cases (3.6%) had no information later recorded by responders, emergency room, or hospital personnel. Thus, the total number of cases studied was 379. Of these 379, 279 (73.6%) were identified as having a diabetic-triggered event.
Overall, 96.8% (367/379) of all the patients had a medical record that documented history of diabetes (Table 2). Every patient who had a diabetic-triggered event had a documented history of diabetes. Of the patients who had a diabetic history (n = 367), 76% (n = 279) had a diabetic-triggered event. The percentage of patients who had a diabetic-triggered event was slightly higher for those who had Type 1 diabetes than for those who had Type 2 diabetes (74.2% [46/62] and 57.7% [30/52], respectively). Although the difference was not statistically significant (two-sided Fisher's Exact, P = .063), this could be attributed to the small sample size.
Table 2 Comparison of Diabetic History and Diabetic-Triggered Events Outcome Measures

aTwo-sided Fishers Exact Test P value assessing significance of association between diabetic history and diabetic-triggered event measures.
bRow percentages.
cColumn percentages.
Per patient medical records, only four cases had non-diabetic proven hypoglycemia, which included an insulinoma. These patients were classified with those having no diabetic history and a non-diabetic triggered event. They were the only patients whose emergencies were related to blood sugar issues, but who were not experiencing a diabetic-triggered emergency.
Discussion
This study demonstrated that when EMDs classified cases as diabetic-triggered events by selecting the Diabetic Problems Chief Complaint protocol, they were correct the majority (73.6%) of the time. In those cases in which the EMD initially selected the Diabetic Problems Chief Complaint protocol but no diabetic-triggered event was found, other medical conditions were found to exist, such as stroke, respiratory problems, pneumonia, and renal failure. Future studies should identify whether the approximately one-quarter of cases assigned to the Diabetic Problems Chief Complaint, in the absence of a diabetic-triggered event, were nonetheless handled at an acuity level appropriate to the seriousness of the problem. This would provide a test of the “safety net” features of the Diabetic Problems Chief Complaint protocol designed to identify and correctly triage priority symptoms, even if the most appropriate Chief Complaint protocol was not initially selected.
The Diabetic Problems Chief Complaint protocol also was demonstrated to be a clinically accurate selection for a large majority of the patients with a diabetic history; 76% of these patients were in fact suffering from a diabetic-triggered event. Only 12 (3.6%) patients were never confirmed to have a history of diabetes, and none of these were suffering from a diabetic-triggered event. Although the sample size in this group was very small, this finding suggests that EMDs should exercise caution in using the Diabetic Problems Chief Complaint for patients with no mentioned history of diabetes. This finding also indicates the potential value of changes to the Diabetic Problems protocol to prompt EMDs to move to a different Chief Complaint for patients with no diabetic history.
Although the sample of patients with no later documented diabetic history was small (12 patients), paramedic on-scene reports indicate that many of the patients without diabetic history were reported by third- and fourth-party callers. By definition, these callers have less knowledge of the patients’ histories. They may provide inaccurate information or simply guess that a patient behaving in a certain way is diabetic. Also, in a few cases, these patients had contact with the police first, generally because they were acting strangely in public, fainting, vomiting, or, in one case, “staggering down the sidewalk.” At least one was recorded as having consumed a significant amount of alcohol, and another was described in the paramedic's report as “possible ETOH [alcohol] abuse.” Occasionally such patients may represent alcoholism to police or others as diabetes to avoid charges of public drunkenness. In other words, callers’ lack of direct information about the patient and, less often, patient claims about being diabetic can explain at least some of the relatively small number of non-diabetic-triggered events handled on this Chief Complaint protocol.
In determining why some patients without diabetic history or diabetic-triggered events were handled on this protocol, it is also important to remember that the EMD can only know what he or she is told. MPDS-certified EMDs are specifically trained to take all callers’ statements at face value to avoid missing potentially serious medical problems due to the error of “judging the caller.”Reference Clawson, Dernocoeur and Rose 7 Without the audio recordings of these calls, it is not possible to know exactly what callers said to EMDs. However, the paramedic reports do suggest that the placements of the 12 non-diabetics into the Diabetic Problems protocol were not necessarily mistakes on the EMD's part or problems with the Chief Complaint selection methodology.
EMDs were trained to use the answer to the primary assessment question, “What's the problem, tell me exactly what happened,” to select a Chief Complaint protocol based on the caller's statements about the patient's signs and symptoms. This Chief Complaint-focused training includes understanding of the Rules, Axioms, and Definitions used in the Additional Information section of each Chief Complaint protocol, which identify common symptoms, conditions, and concerns related to that complaint. The proper use of this specific information is particularly important in handling diabetic problem calls since diabetic problems can mimic, or be mimicked by, other medical conditions.
In addition, EMDs are trained to recognize common terms and phrases used by callers to suggest a diabetic history. Some such terms and phrases (unpublished survey data n = 174) are: low blood sugar (86.8%), diabetic coma (48.9%), hypoglycemia (44.8%), insulin shock (41.4%), insulin use (37.9%), oral diabetic medicine (16.1%), diabetic ketoacidosis (15.5%), or tumor that secretes insulin—an insulinoma (1.1%). Others may include diabetic emergency, sugar diabetes, sugar shock, high blood sugar, references to the patient having just eaten food or candy containing sugar, or references to sugar problems, sugar attacks, and high or low sugar. Callers often also report that the patient is confused or not acting right, along with references to a history of diabetes. If the caller is first party (the patient), he may report his own diabetic history, and the same is true of second-party callers who know the patient; third-party callers may report that they “think” they patient is diabetic based on their own experiences with the disease, or they may rely on information from someone else.
Correctly selecting the Diabetic Problems Chief Complaint protocol is therefore a process that relies collectively on the patient's level of communicative ability, the caller's knowledge or impression, the EMD's specific training and access to additional Chief Complaint-specific information, and the EMD's evaluative judgment of the case specifics. As a result of this complexity, the ability of EMDs to accurately identify true diabetic-triggered events and to handle them correctly on the Diabetic Problems protocol is a significant concern.
This study was intended to test the assumption that caller statements about diabetes can be relied on in selecting the Diabetic Problems Chief Complaint protocol. Many callers will state information about the patient's diabetic history to the EMD (or use commonly-understood terms, such as “got the sugar” or “sugar attack”), so it is intuitively sound to assume that properly-trained EMDs can use caller reports as a reliable method for selecting the Diabetic Problems Chief Complaint. This assumption has been found to be generally sound, since 97% (367/379) of patients initially assigned to this protocol had a confirmed history of diabetes, and of those with a later confirmed diabetic history, 76% (279/367) had a diabetic-triggered event.
The potential problem with the diabetes assumption is that statements about diabetic history could overshadow other, more serious complaints. This problem has been demonstrated to be largely nonexistent, as 76% of those with documented history of diabetes were confirmed to be experiencing diabetic-triggered events as the immediate reason for their emergency call.
Additionally, chronic medical problems that can be caused by diabetes 8 were found to be the true reason for the emergency call in many of the other 24% of cases. This indicates that many of these non-diabetic-triggered events may in fact have been diabetic related, even if not diabetic triggered. Even in these cases, then, the selection of the Diabetic Problems protocol was not so much incorrect as potentially non-optimal.
Limitations
Although the investigators were able to follow up the MPDS's Diabetic Problems Chief Complaint cases, (n = 393) and obtain their hospital outcome data (forward approach), the backward approach (ie, to obtain all hospital records that had diabetes as a final diagnosis or a listed condition and then match them with their respective MPDS codes to find out which chief complaints they were initially assigned to) was not performed. The backward approach would be important to identify which other MPDS protocol(s) may also have been used to evaluate and prioritize diabetic-triggered events. While the authors would have preferred to determine whether, at the Chief Complaint selection point, other 911 patients classified into other Chief Complaints had diabetic-triggered problems, this would require studying hospital record outcomes for all 911 patients for the entire study period; this is currently beyond most systems’ capabilities.
Access to the actual audio records of the EMD interrogations in order to provide an actual compliance score for the individual cases in this study was not performed. However, as reported in the methods above, the 911 center has been IAED-accredited from 1997 until present, and had a very high recorded compliance rate during the study period. This study's data also did not include the caller party type (ie, first-party caller: the patient; second-party caller: a caller with direct access to the patient; third-party caller: a caller not with the patient; fourth-party caller: a remote referral from another agency, such as a security firm or airport control center). Because first- and second-party callers generally provide more accurate information, comparison with third- and fourth-party callers may provide more specific results.
Certain priority symptoms, by MPDS rules, contraindicate the selection of the Diabetic Problems Chief Complaint protocol, regardless of a patient's diabetic history or the caller's impression of the problem. For example, if a reported diabetic patient is not conscious and not breathing, or if the complaint includes chest pain, the Cardiac or Respiratory Arrest/Death protocol or the Chest Pain protocol, respectively, would be selected. This limitation would need to be considered when studying hospital outcomes being traced back to their initial MPDS Chief Complaint codes.
Finally, the number of discordant reviews (between the two reviewers), who performed the initial case reviews, was very small (fewer than five cases). Therefore, it was not useful to perform inter-rater reliability with the small sample size.
Conclusions
This study demonstrated that when certified EMDs initially selected the Diabetic Problems Chief Complaint, they correctly identified a diabetic-triggered event the majority of the time. Future studies should examine the associations between the EMD-assigned MPDS determinant codes and scene-determined severity measures such as blood sugar level and Glasgow Coma Score. Further research should also examine the impact of caller party type on the EMD's ability in selecting the Diabetic Problems Chief Complaint, as well as the usefulness of the caller's degree of familiarity with, or proximity to, the patient.
Acknowledgments
The authors would like to thank the following agencies and hospitals who helped with the data collection and initials processing: Salt Lake City Fire Department, Gold Cross Ambulance Services, LDS Hospital, Primary Children Medical Center, Salt Lake Regional Medical Center, St. Mark's Hospital, University of Utah Medical Center, and Veteran Affairs Medical Center. The authors also thank Pamela Stewart, Chair of the Board of Certification, IAED, for managing the various Institutional Review Board maintenance and renewal processes.





