CASE PRESENTATION
A 42-year-old African man presented to the Hospital of the University of Pennsylvania Emergency Department (ED) in 2019 with altered mental status, vomiting, and diarrhea of unclear duration. Limited history initially available included that he worked as an Ebola virus disease (EVD) researcher and had arrived in Philadelphia 1 day prior from the Democratic Republic of Congo (DRC), where he was working in unknown proximity to an ongoing EVD epidemic.1 His family could not reach him after he arrived in Philadelphia, which resulted in the dispatch of local emergency medical services. Upon arrival to his hotel room, paramedics found the patient sitting in a chair, confused, incontinent of brown stool, and surrounded by emesis. While driving enroute to our ED, the ambulance transmitted his history and his vital signs, which were notable for a fever.
Based on his travel and exposure history, fever, and gastrointestinal symptoms, he met criteria to be classified as a “wet,” or potentially highly infectious, person under investigation (PUI) for EVD,Reference Wadman, Schwedhelm and Watson2,Reference Malvy, McElroy and de Clerck3 and, per protocol, the ED called our bioresponse hotline. This activated our hospital emergency management command center and bioresponse teams, and alerted the Philadelphia Department of Public Health, the Pennsylvania Department of Health, and the Centers for Disease Control and Prevention (CDC).
Because of the close proximity of the patient’s hotel, the predesignated “wet” patient treatment area in the ED could not be cleared of the critically ill patients occupying those spaces prior to the ambulance’s arrival. The patient was therefore brought immediately from the ambulance to an unoccupied negative pressure room in the ED. The ambulance was locked and taken out of service. The paramedics, who had not worn any non-routine personal protective equipment (PPE), were quarantined in a separate nearby ED room and attended to by their organization’s safety officer. Nearby patients were moved elsewhere for their safety and to allow for the creation of an ad hoc “warm zone” decontamination space spanning adjacent treatment rooms and the ED hallway. Three specially trained clinicians – an emergency medicine attending physician, an ED nurse, and a medical critical care attending – donned “wet” PPE, including full-body coverall, powered air purifying respirator (PAPR), face shield, hood, shoe covers, and double gloves,Reference Suen, Guo and Tong4 and entered the patient’s room to begin evaluation and treatment.
Vital signs on arrival included a temporal temperature of 104.0°F; blood pressure of 94/53 mm Hg; respiratory rate of 32 breaths per minute; heart rate of 115 beats per minute; and oxygen saturation of 100% on 100% non-rebreather mask, which was quickly weaned to room air. His initial physical exam was notable for a well-nourished man without signs of chronic illness but acutely ill appearing. He was somnolent, only briefly arousable to painful stimuli, and unable to consistently answer questions or follow commands. Cranial nerves were intact, and there were no signs of meningismus. He had dry mucous membranes and no scleral icterus. He was tachypneic but without the use of accessory muscles and was protecting his airway. He had a tachycardia that was regular; the point of maximal impulse was not displaced, and there was no right ventricular heave. His abdomen was soft, non-tender, non-distended, and there were no masses or palpable organomegaly. He had no rashes, petechiae, or skin breakdown. His lower extremities were warm with no edema. His stool was brown, liquid, and negative for occult blood. Traditional stethoscopes could not be used through PPE. His clothing was examined and was notable for non-bloody stool.
Point-of-care ultrasound was performed, as it was the only immediately available diagnostic imaging modality in the setting of high-risk pathogen isolation precautions. Ultrasound findings were notable for no lung consolidation, pleural effusions, or B-lines and normal pleural sliding throughout the lungs; grossly normal left ventricular ejection fraction, grossly normal right ventricular function, and no pericardial effusion; no liver abscesses, gallbladder inflammation, or free fluid in the abdomen; and an underfilled, collapsing inferior vena cava. Laboratory studies were drawn but processing was delayed while limited point-of-care testing was set up and the high-risk pathogen specimen laboratory protocol was activated.
DIFFERENTIAL DIAGNOSIS, MANAGEMENT, AND CLINICAL COURSE
Our initial differential diagnosis was centered upon malaria, EVD, and bacterial sepsis. Initial management included placement of 3 large bore peripheral intravenous lines and a temperature-sensing urinary catheter, initiation of aggressive crystalloid volume resuscitation with Ringer’s lactate solution, rectal acetaminophen, and empiric antimicrobial therapy with intravenous vancomycin, cefepime, amikacin, and metronidazole. His hypotension progressed, necessitating initiation of low-dose peripherally administered norepinephrine. His high fever persisted, and ice packs were placed in his axillae and groin.
Limited laboratory results were first available 4 hours after presentation (Table 1) and were notable for markedly elevated lactate, leukocytosis, thrombocytopenia, elevated creatinine, and elevated total bilirubin. Thin and thick blood smears revealed Plasmodium falciparum and concern for low-level co-infection with Plasmodium malariae, based on the presence of later stage parasites, including rare schizonts, with initial total parasitemia of 2.9%. Malaria immunochromatographic antigen testing (BinaxNOW Malaria, Abbott Laboratories) was positive for the histidine-rich protein II (HRPII) antigen specific to P. falciparum and for a nonspecific pan-Plasmodium aldolase antigen. In the presence of confirmed P. falciparum infection by a positive HRPII antigen, the positive aldose antigen does not further distinguish between P. falciparum mono-infection and the possibility of co-infection with an additional non–P. falciparum strain.Reference Ota-Sullivan and Blecker-Shelly5
TABLE 1 Laboratory Studies

Notes: ALT = alanine aminotransferase; AST = aspartate aminotransferase; INR = international normalized ratio; LDH = lactate dehydrogenase; PT = prothrombin time; PTT = partial thromboplastin time; RBC = red blood cell.
At this time, the patient was given a diagnosis of cerebral malaria and septic shock with multisystem organ dysfunction, including circulatory dysfunction, encephalopathy, metabolic lactic acidosis, acute kidney injury, acute liver injury, and diffuse intravascular coagulation with thrombocytopenia. He was started on intravenous quinidine gluconate and adjunctive intravenous doxycycline for malaria, and he was continued on broad-spectrum antibiotics. (Intravenous artesunate is not approved by the U.S. Food and Drug Administration and not commercially available in the United States, and can only be obtained under emergency circumstances from the CDC in Atlanta, GA.)Reference Twomey, Smith and McDermott6
Repeat laboratory studies (see Table 1) showed worsening of his metabolic lactic acidosis, despite a 5-liter crystalloid fluid resuscitation, and his exam was notable for worsening mental status and tachypnea. He underwent rapid sequence endotracheal intubation using etomidate and succinylcholine with a primary indication of refractory metabolic acidemia and a secondary indication of airway protection. Intubation via direct laryngoscopy was technically challenging in the setting of PPE and the patient’s friable oral mucosa and thrombocytopenia, but was successful and confirmed by end-tidal CO2. A chest X-ray was facilitated without breaching isolation precautions, using a previously developed protocol, and showed clear lung fields and an endotracheal tube requiring minor repositioning.
After intubation, the patient developed progressive shock requiring further volume resuscitation, up-titration of norepinephrine, addition of vasopressin and epinephrine, and placement of an internal jugular central venous catheter. His ventilator was titrated to a high minute ventilation (up to VE 21 L/min) and high flow rate to compensate for his severe metabolic acidemia. He was pharmacologically paralyzed to allow synchrony with this ventilatory strategy and to avoid hemodynamically significant ventilator dyssynchrony.
Samples from his initial phlebotomy were sent by official courier to the Pennsylvania Department of Health for EVD real-time reverse transcriptase polymerase chain reaction (rRT-PCR) testing,Reference Broadhurst, Brooks and Pollock7 which returned negative 10 hours after initial presentation. Because EVD testing can return a false negative in the first 72 hours after symptom onset and the patient could not provide a history,Reference Broadhurst, Brooks and Pollock7 he was maintained in isolation precautions. Using a negative pressure transport tent (IsoPod Isolation Stretcher, Airboss of America Corp.), he was then transferred from the ED to our Special Treatment Unit for continued management by the medical critical care bioresponse team.
Collateral history was later available from the patient’s family, who dated his symptom onset, including fever, at 10 days prior to presentation, with a lull and then recrudescence 3–4 days prior to presentation and prior to his travel from the DRC to Philadelphia. Of note, the initial symptom onset was approximately 24 hours after the patient received the V920 Ebola Zaire Vaccine (rVSVΔG-ZEBOV-GP, Merck & Co., Inc., Kenilworth, NJ, USA),Reference Regules, Beigel and Paolino8 an attenuated, replication-competent, recombinant vesicular stomatitis virus–based vaccine being distributed to persons living or working in high-risk areas of the DRC. The family also noted that he did not routinely take malaria prophylaxis when in endemic areas and had not been taking prophylaxis at the time that he initially became ill. A notable past medical history included prior malaria infections without sequelae and well-controlled type 2 diabetes mellitus.
At this time, a multidisciplinary discussion between our institution and city, state, and federal public health officials came to the consensus that the patient had greater than 72 hours of symptoms prior to his EVD test, making it a definitive negative test and allowing for the removal of isolation precautions. The clinical team, in particular, was in favor of the discontinuation of EVD precautions as his shock and multisystem organ failure continued to worsen, and renal replacement therapy was imminent. The patient was subsequently transferred from the Special Treatment Unit to the regular medical intensive care unit (ICU) on Hospital Day 2 for continued management. Parallel EVD testing at CDC laboratories on a sample forwarded from the Pennsylvania Department of Health was also subsequently negative, though this result returned approximately 16 hours after results from the state laboratory.
Removal of isolation precautions allowed for access to expanded routine laboratory and imaging diagnostics with pertinent findings, including computed tomography of the head without cerebral edema, hemorrhage, or infarction; computed tomography of the chest, abdomen, and pelvis without foci of infection, splenomegaly, or other major abnormalities; electroencephalogram without seizures; and transthoracic echocardiogram with low normal left ventricular ejection fraction. It also allowed for a rapid return to normal operations for the rest of the hospital, including cleaning and bringing back into service the involved ED rooms, ambulance, and Special Treatment Unit, which functions as a normal care space for 6 inpatients under routine circumstances. The quarantined paramedics, who had undergone decontamination of their persons and personal effects under the supervision of the bioresponse team and their organization’s safety officer and had been released under Philadelphia Department of Public Health surveillance, were released from further monitoring.
The patient’s ICU and remaining hospital course was notable for initiation of temporary continuous renal replacement therapy for metabolic acidemia and acute kidney injury with eventual slow renal recovery; resolution of shock and liberation from vasopressors but complicated by peripheral digital ischemia; a secondary bacterial aspiration pneumonia requiring re-intubation but ultimate liberation from the mechanical ventilator without tracheostomy; slowly improving mental status; and significant but slowly improving neuromuscular weakness requiring a moderate 2-person assist to ambulate at the time of hospital discharge.
The patient’s malaria parasitemia peaked at 7.0% on Hospital Day 2 and cleared by Hospital Day 4. He completed 3 days of intravenous quinidine and 5 days of intravenous doxycycline (continued in lieu of artesunate due to clinical improvement). Final molecular diagnostics performed by the CDC, including rRT-PCR and nested PCR assays, confirmed the presence of P. falciparum mono-infection without evidence of P. malariae co-infection. Schizonts on initial microscopy that were suspicious for P. malariae likely instead represented developing or immature P. falciparum schizonts. Blood cultures showed no bacterial growth throughout his hospitalization.
The patient was transferred out of the ICU on Hospital Day 12 and was discharged on Hospital Day 21 to begin rehabilitation. His complete disease course is illustrated in Figure 1.
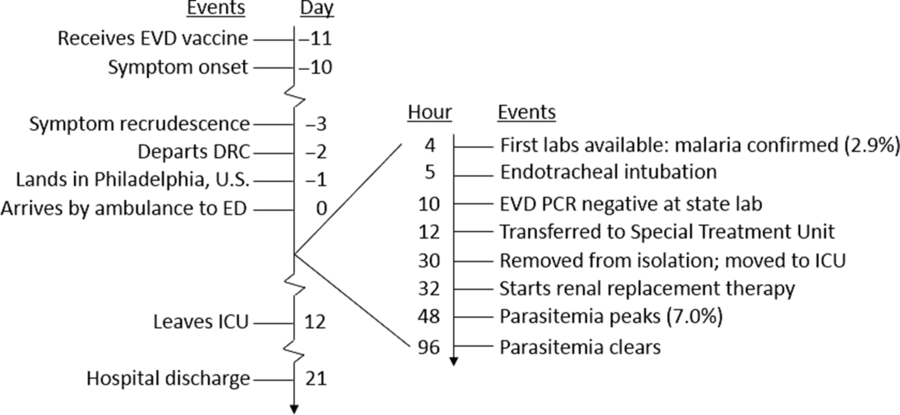
FIGURE 1 Patient timeline
DISCUSSION
Ebola treatment units throughout West and Central Africa are well versed in the care of patients with confirmed or suspected EVD, and continue to actively combat an ongoing EVD epidemic in the DRC, which has claimed over 2100 lives, the second worst on record behind the 2013–2016 West African epidemic.1 For hospitals like ours, physically remote from any active epidemic but serving a high-volume international air travel port-of-entry, the approach to risk assessment and preparedness is far different. Preparing for rare, resource-intensive events (such as caring for patients with possible EVD and other high-risk and emerging pathogens) is challenging. Clinical and operational skills can easily wane. Longitudinal funding and physical resource allocation, including supplies and treatment space, can be difficult to justify; however, the low-frequency, high-impact threat remains.
After the 2013–2016 EVD epidemic, which motivated massive acute global preparedness efforts that, in the United States, were largely unused by critically ill patients, our institution transitioned to a more longitudinal preparedness strategy involving a core group of clinical, operations, and administrative personnel with scheduled training and simulation. This case was our most significant test of that strategy and motivated a thorough evaluation of our capabilities and continued challenges. There are numerous clinical and operations issues worthy of reflection and discussion, and our institution undertook a comprehensive self-evaluation. However, this brief report highlights 3 themes heavily impactful on successful preparedness in hospitals like ours.
Malaria as a Primary Differential Diagnosis
Based on incidence, common zones of disease activity, and overlapping clinical syndromes, malaria and bacterial sepsis remain the primary differential diagnoses for a PUI for EVD.Reference Malvy, McElroy and de Clerck3 Hospitals outside of malaria-endemic areas, such as in the United States, may see only rare cases in returning and arriving travelers and may lack optimal clinical familiarity with diagnosis and management, as well as access to first-line parenteral artemisinins (ie, artesunateReference Twomey, Smith and McDermott6) or cinchona alkaloids (ie, quinidine). Our team discussed at length the implications on treatment and isolation decisions of an early diagnosis of malaria but with seemingly low parasitemia (2.9%) relative to the severity of multisystem organ dysfunction with profoundly elevated serum lactate (up to 13.9 mmol/L). In hindsight, this discordance likely represented under-measured parasitemia due to sequestration of P. falciparum–infected red blood cells in splenic and cerebral vascular beds,Reference Idro, Jenkins and Newton9 contributing to significant clinical debate in real time. We also considered the risk of malaria-EVD co-infection, which was documented in up to 21% of EVD-positive patients during the 2013–2016 epidemic.Reference Waxman, Aluisio, Rege and Levine10
Finally, we considered whether the patient’s receipt of the rVSVΔG-ZEBOV-GP vaccine 24 hours prior to symptom onset was related to his malaria diagnosis or severity. Safety reporting from the Sierra Leone Trial to Introduce a Vaccine Against Ebola (STRIVE), a randomized controlled trial of the rVSVΔG-ZEBOV-GP vaccine reported that vaccinated participants compared to unvaccinated participants had higher rates of post-vaccination malaria (incidence per 100 person-years [95% CI]: 0.59 [0.31-1.04] vs 0.12 [0.01-0.42]).Reference Jarrett, Seward and Fombah11 It is not clear what causal mechanism might explain this, and data on malaria severity were not reported. Our patient’s case was reported to the vaccine manufacturer.
While the establishment of a malaria diagnosis is ultimately essential, we posit it is not as emergently time-sensitive as initially perceived. Empiric antimalarial therapy can be initiated before a diagnosis is confirmed (this has been integrated into our EVD algorithm for future cases), isolation decisions will wait for definitive EVD testing regardless, and routine laboratory studies – blood gas analysis, lactate, complete blood count, and a metabolic panel – are likely to provide more helpful information to guide early clinical management. This hierarchy can guide a core group of laboratory scientists and technicians with special pathogen training who have limited bandwidth and equipment during management of an active case.
In-Room Bedside Management
A hallmark of high-risk pathogen care, except perhaps in the most resourced, specialized, and longitudinally dedicated treatment units, is limited personnel and limited or restricted diagnostics available at the bedside. The cost of reducing the number of bedside clinicians put at risk of a potential accidental exposure – typically to a rotating bedside nurse and primary-team-attending physician – is the unavailability of other specialized skillsets at the bedside. The 2 most noticeable and impactful personnel bedside absences, in our experience, were respiratory therapists and specialist consultants. For example, medical intensivists who are used to ordering mechanical ventilator settings in a well-resourced setting under normal operational circumstances must be prepared for comprehensive management of a mechanical ventilator, including setup, powering on, settings input, and responding to alarms.
While cross-sectional imaging, including computed tomography scanning, is generally not available, point-of-care ultrasound is the most accessible and useful imaging modality in the isolation setting (and often indicated under routine non-isolation circumstances). Given the variability in point-of-care ultrasound proficiency,Reference Stowell, Kessler and Lewiss12 it should be a point of attention in any high-risk pathogen preparedness training plan. Chest radiographs, with planned choreography, can be done safely and effectively through isolation, but we note that increasingly sophisticated point-of-care ultrasound maneuvers, such as thoracic ultrasoundReference Shrestha, Weeratunga and Baker13 and the use of agitated saline for central venous catheter position placement,Reference Bou Chebl, Kiblawi and El Khuri14 may continue to reduce the need.
Ethical Challenges of Care Delivery in Prolonged Isolation
Care delivery in isolation is unambiguously appropriate in the setting of a patient potentially infected with a high-risk pathogen, such as the Ebola virus, that poses great risk to bedside clinicians, other patients, and bystanders. It is also true that critical care provided in the setting of high-risk pathogen isolation is unambiguously inferior to the standard of care provided outside of such isolation and especially so in well-resourced settings. This makes pivotal the decision of when to discontinue isolation. Factors that dictate that decision include (1) knowledge of the disease-specific period from symptom onset during which diagnostic testing may return a false negative and is therefore not definitive (72 hours for EVD)Reference Broadhurst, Brooks and Pollock7; (2) a timely and accurate history of present illness to establish a time of symptom onset; (3) prompt and safe sample collection, transport, and testing to establish a definitive diagnosis; and (4) identification of which lab or labs can provide definitive results on which a decision to discontinue isolation can be based. Any time spent in isolation when it could have been discontinued is a disservice to the patient and sequestered family members.
SUCCESSES AND SHORTCOMINGS
We relied heavily on detailed clinical operations protocols first written at our institution during the 2013–2016 EVD epidemic and revisited through periodic tabletop and live-action simulations by a core dedicated workforce in the interim years. Tasks that are straightforward under normal operational circumstances – performing a portable chest X-ray, setting up a mechanical ventilator, obtaining and analyzing routine laboratory studies, and transporting a patient from 1 area of the hospital to another – were successful yet complex in the setting of isolation, and would have been impossible without this preparation.
We continue to struggle with the correct approach to the staffing of trained clinicians. In order to maintain longitudinal proficiency in this complex skillset for a rare event, we have operated with a small, core group. While proud of the quality of our clinical and operational performance during this event, we note in our post hoc analyses that our clinical personnel resources (specially trained bedside physicians and nurses) would have been exhausted had isolation been required for a prolonged period or for more than 1 patient simultaneously. We have since expanded our core critical care team and added a second layer of clinicians eligible for just-in-time training in the event that we might need to rapidly expand our capabilities.
Individual hospitals and health systems have to make individualized decisions about preparedness planning based on their own risk assessments, regional threats, organizational characteristics, and resources. We continually learn from training resources from established leading governmental (eg, Federal Emergency Management Agency’s Center for Domestic Preparedness, US Department of Health and Human Services Office of the Assistant Secretary for Preparedness and Response, CDC, Pennsylvania Department of Health), non-governmental (eg, National Ebola Training and Education Center), and academic (eg, the University of Nebraska Medical Center, Emory University School of Medicine) preparedness programs, and provide open access to our own preparedness program to inquiring hospitals. Most helpful for our institution has been a core longitudinal leadership group, written protocols that can be adapted to fit the unique challenges of new emerging threats, and simulation of the most high-yield, risk-reducing response activities (eg, PPE donning and doffing, patient transport).
CONCLUSION
Hospitals remote to high-risk pathogen outbreaks and ongoing epidemics are still at risk for rare but potentially high-impact events. Among numerous factors, successful preparedness strategies should optimize clinical management in high-risk pathogen isolation using pre-planned and simulated protocols while simultaneously minimizing isolation duration to the shortest necessary for public safety.
Statement of Informed Consent
The patient described provided informed consent for the publication of this report.
Elements of this case were initially presented at the Drinker Critical Care Society meeting (April 2019, Philadelphia, PA). This case has not been published nor is under review for publication elsewhere.
Acknowledgments
The authors wish to acknowledge and thank the numerous individuals across Penn Medicine and at the collaborating public health agencies for their dedication to our patient’s care and to the safety of our other patients, staff, and community during this process. In particular, the authors acknowledge Teresa Murphy (RN) and Heather Trout (RN) (leadership of the Special Treatment Unit and bioresponse nurses); Irving Nachamkin (DrPH, MPH) and Deborah Mincarelli (Pathology and Laboratory Medicine); and Kevin Heym, John Wierzbowski (MSc, MPH, CHEP), Nick Pinizzotto, and Jeffrey Henne (Safety & Emergency Management). Finally, the authors offer profound thanks to the patient, who gave his permission to publish this report and has dedicated his professional life to combating Ebola virus disease.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.




