Introduction
Laryngeal cancers and, to a lesser extent, hypopharyngeal cancers are common among head and neck cancers in the UK. There are over 1700 new cases each year with an increased incidence in males, where they occur around five times more frequently.1 Incidence has remained stable for the past decade in both Scotland and the UK as a whole despite falling tobacco use, but notwithstanding this, a projected decrease of around 17 per cent in its incidence has been predicted over the next 20 years.1,2 Mortality rates have fallen by 10 per cent over the past decade and are projected to continue falling as diagnostic and management strategies improve.3 Overall, 19–59 per cent of patients diagnosed with head and neck cancer in the UK will survive beyond 5 years, depending on the stage.2,3
Total laryngectomy, with or without pharyngectomy, is indicated as a treatment option in either the primary treatment (primary total laryngectomy) of advanced laryngeal or hypopharyngeal cancers or as a salvage procedure (salvage total laryngectomy) following recurrence after laser surgery, radiation or chemoradiation. Total laryngectomy can also be utilised in a variety.
Although recent trends show a move towards organ-sparing treatments,Reference Sayles and Grant4,Reference Stankovic, Milisavljevic, Zivic, Stojanov and Stankovic5 total laryngectomy has long been established as one of the cornerstones in the treatment of advanced laryngeal cancers, offering potentially superior survival rates for those with advanced local disease.Reference Dyckhoff, Plinkert and Ramroth6–Reference Busoni, Deganello and Gallo8
Total laryngectomy can result in major changes to a patient's breathing and swallowing, resulting in significant functional and psychological morbidity. This may be compounded by complications, such as wound or chest infection, neopharyngeal stenosis, and pharyngocutaneous fistulae. Pharyngocutaneous fistulae and neopharyngeal stenosis can have a large impact on duration of hospital admission and long-term functional outcomes in particular.Reference Sayles and Grant4 Identifying predisposing factors for these complications may allow optimisation of peri-surgical care and improve post-operative outcomes.
In this study, we report the surgical complications of total laryngectomy performed in NHS Lothian for squamous cell carcinoma (SCC) of the larynx and hypopharynx over a 10-year period, with a focus on predisposing factors for complications, neopharyngeal stenosis and pharyngocutaneous fistulae rates.
Materials and methods
Patients and ethical considerations
The project was registered with the trust's Caldicott Guardian and all data were anonymised and stored in concordance with data protection laws.
All patients undergoing total laryngectomy in NHS Lothian for SCC of the larynx or hypopharynx between 2007 and 2016 were included. Patients with other tumour types or indications were excluded.
Data collection
A retrospective review of electronic clinical records and speech and language therapy records between 2007–2016 was performed. Data collected included: demographic information (age, gender, and tumour site and subsite), pathological details (using guidelines from the 7th edition of Tumour–Node–Metastasis Staging), modality of treatment (surgery with or without chemotherapy or radiotherapy), pre-operative haemoglobin level, primary tracheoesophageal puncture, and complication rates of pharyngocutaneous fistulae and neopharyngeal stenosis.
Reconstruction management
Our institutional approach to reconstruction after total laryngectomy is based on an individualised, patient-centred decision depending on the extent of surgery, tissue condition and patient co-morbidities. Pedicled or free flap reconstruction is routinely used in the salvage setting after chemoradiation and selectively used in patients who received either radiotherapy alone or had a pharyngeal resection that could not be closed primarily.
Definitions
The definition of neopharyngeal stenosis varies in the literature, with either direct visualisation, radiological or functional definitions being offered.Reference Walton, Vellucci, Patel, Jennings, McCammon and Underbrink9,Reference Sweeny, Golden, White, Magnuson, Carroll and Rosenthal10 Due to this, we report two different rates: the first required at least one neopharyngeal dilatation and/or a long-term feeding tube to maintain nutrition, and the second rate required more than one neopharyngeal dilatation and/or a long-term feeding tube. The more conservative diagnosis of requiring at least one dilatation was used for further analysis in this study, to ensure stenosis rates were not under-reported.
The relationship between predisposing factors and pharyngocutaneous fistulae development was also analysed. The impact of a low pre-operative haemoglobin level on pharyngocutaneous fistulae was investigated, using a haemoglobin level of less than 125 g/l, based on previous literature.Reference Paydarfar and Birkmeyer11 Additionally, the use of pre-operative therapy (chemoradiotherapy or radiotherapy alone) on pharyngocutaneous fistula development in the salvage total laryngectomy cohort was also analysed.
Statistical methods
The outcomes of both primary total laryngectomy and salvage total laryngectomy were analysed in separate subgroups, using SPSS® statistical software.
To detect differences in complication rates between primary total laryngectomy and salvage total laryngectomy groups, the chi-square test for categorical data was used. Logistic regression was used to analyse predisposing factors for complications.
Results
Demographic data
In total, 173 patients underwent total laryngectomy for SCC of the larynx or hypopharynx in NHS Lothian between 2007 and 2016. Further demographic data, including gender, age and follow up is shown in Table 1.
Table 1. Demographic data

*Total n = 173; †total n = 114; ‡total n = 59; **statistically significant result. Pts = patients; PTL = primary total laryngectomy; STL = salvage total laryngectomy; PCF = pharyngocutaneous fistula; NPS = neopharyngeal stenosis
The annual trend over the 10-year period shows a gradual reduction in primary total laryngectomy procedures performed (Figure 1). It can also be seen that primary total laryngectomy was performed in the management of more advanced cancers (pathological tumour stage at diagnosis).

Fig. 1. Number of primary total laryngectomy operations performed by pathological tumour stage during the study period.
Conversely, the number of salvage total laryngectomy procedures performed across the study period remained relatively constant and it was shown to be favoured in the management of less advanced cancers, with an earlier pathological tumour stage at recurrence (Figure 2).
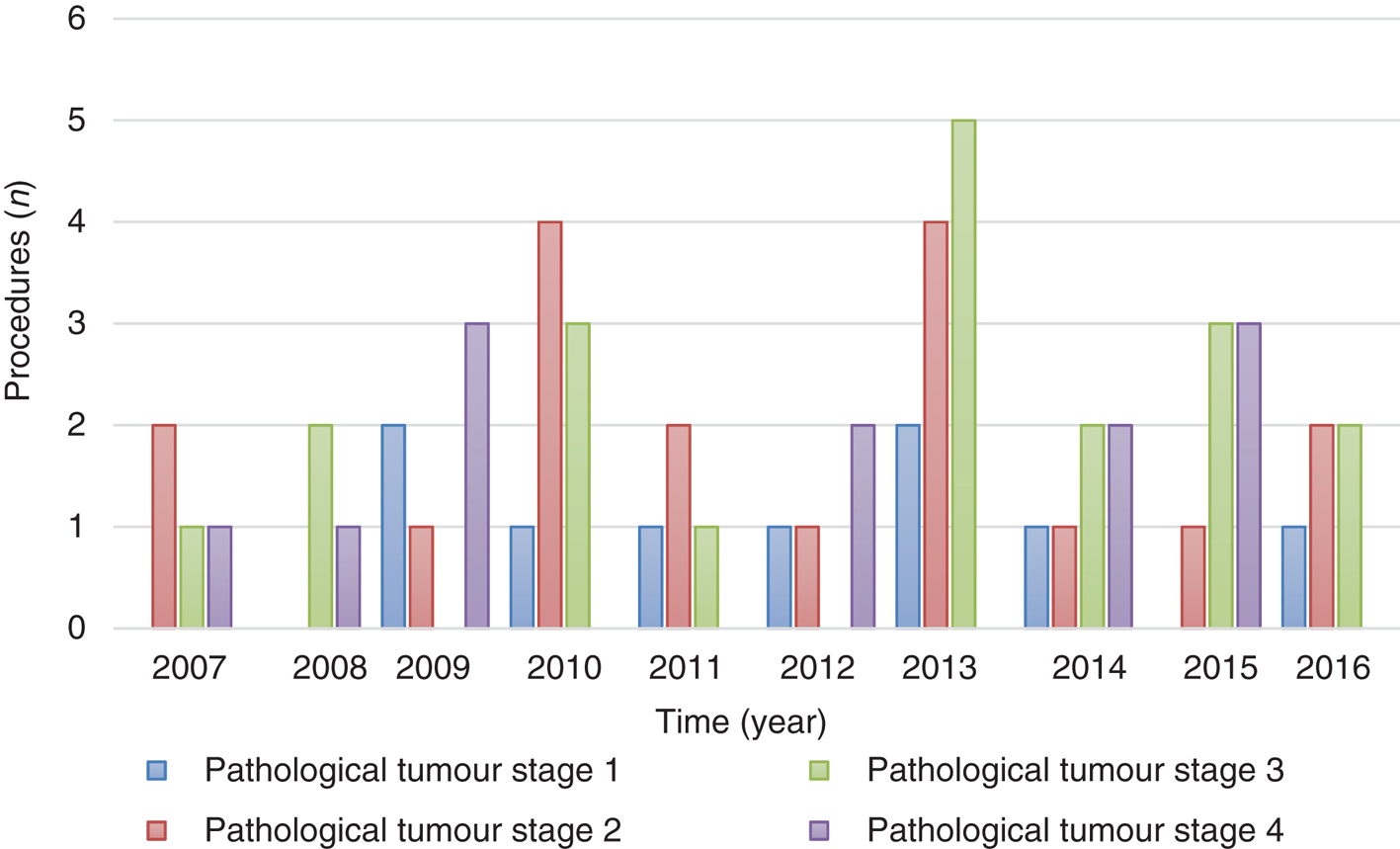
Fig. 2. Number of salvage total laryngectomy operations performed by pathological tumour stage over the study period.
Overall, 81 per cent (140 of 173) of tumours arose from the larynx, and the remaining 19 per cent arose from the hypopharynx. Further details of the demographic data, distribution of pathological tumour staging and nodal staging (stage at recurrence in the salvage total laryngectomy cohort), and treatment modalities are shown in Table 1.
A comparison of cohorts demonstrated a statistically significant difference between the pathological tumour staging and pathological nodal staging, reconstruction rates and pharyngocutaneous fistulae rates. Primary total laryngectomy was more commonly performed for locoregionally advanced disease and reconstruction was utilised less often than in salvage total laryngectomy. Details of treatment modality in each cohort can be seen in Table 1. Of note, only one patient in the salvage total laryngectomy cohort had previously undergone laser resection of an early laryngeal cancer that went on to recur.
Reconstruction
The overall reconstruction rate was 33 per cent and was higher in the salvage total laryngectomy cohort. The distribution of reconstruction by type for each cohort can be seen in Table 2.
Table 2. The type of reconstruction used for each cohort

PTL = primary total laryngectomy; STL = salvage total laryngectomy
Pharyngocutaneous fistulae development
Overall, 11 per cent (19 of 173) of patients developed pharyngocutaneous fistulae, with 6 per cent (7 of 114) affected in the primary total laryngectomy cohort and 20 per cent (12 of 59) in the salvage total laryngectomy cohort (p = 0.005).
As seen in Table 3, there was a statistically significant association between the development of pharyngocutaneous fistulae following reconstruction in the primary total laryngectomy cohort only (p = 0.02).
Table 3. Additional associated factors for patients who developed pharyngocutaneous fistulae

*Statistically significant result. PTL = primary total laryngectomy; STL = salvage total laryngectomy; PCF = pharyngocutaneous fistula
There was an even distribution of patients across the other associated factors, except for gender, which showed a possible male predominance. However, this failed to reach statistical significance.
In both cohorts, pharyngocutaneous fistulae development occurred most frequently within the first month post-operatively.
Predisposing factors for pharyngocutaneous fistulae
The relationship between predisposing factors and the development of pharyngocutaneous fistulae was calculated using logistic regression analysis and failed to reach statistical significance for pre-operative haemoglobin levels with primary chemoradiotherapy or radiotherapy alone in the salvage total laryngectomy cohort. The results can be seen in Table 3.
Neopharyngeal stenosis rates
Neopharyngeal stenosis rates differed depending on the definition adopted. Overall, 11 per cent (19 of 173) of patients required at least 1 neopharyngeal dilatation and/or had feeding tube dependence to maintain nutrition, and 6 per cent (10 of 173) of patients required more than 1 neopharyngeal dilatation and/or had feeding tube dependence. Two patients (one in each cohort) required permanent feeding tube placement.
Further cohort analysis showed higher rates of neopharyngeal stenosis in the salvage total laryngectomy cohort, regardless of the definition used but dropped again when the definition of more than 1 dilatation and/or feeding tube dependence was adopted. As aforementioned, the more conservative definition is further reported below in Table 4.
Table 4. Associated factors for patients that developed neopharyngeal stenosis
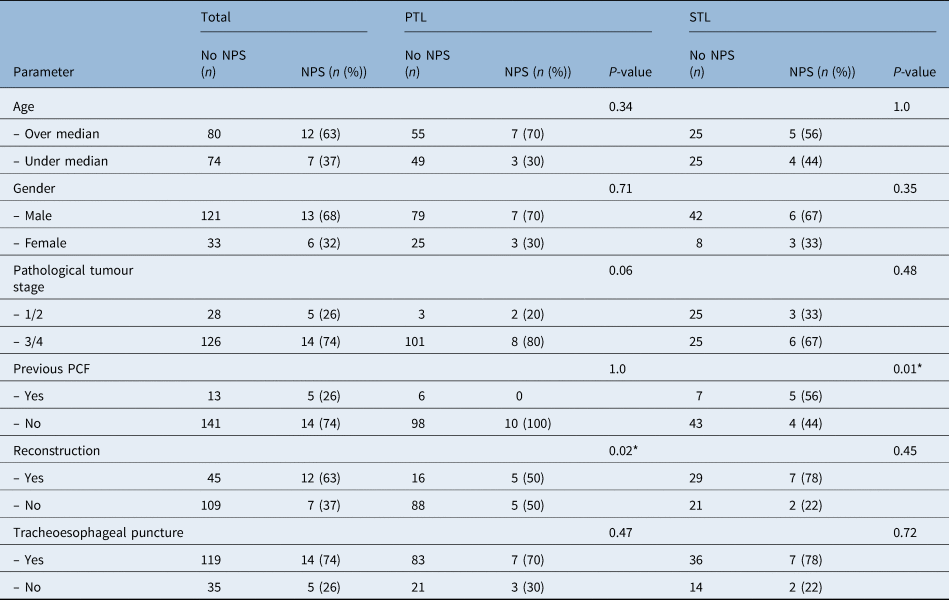
*Statistically significant result. PTL = primary total laryngectomy; STL = salvage total laryngectomy; NPS = neopharyngeal stenosis; PCF = pharyngocutaneous fistula
In the primary total laryngectomy cohort, the time to neopharyngeal stenosis development varied from 3–28 months post-operatively, with a median of 7 months. In the salvage total laryngectomy cohort, this varied from 1–14 months, with a median of 5 months.
As can be seen in Table 4, it was found that patients were significantly more likely to develop neopharyngeal stenosis following a pharyngocutaneous fistula in the salvage total laryngectomy cohort (p = 0.01). Additionally, patients were significantly more likely to develop neopharyngeal stenosis following reconstruction in the primary total laryngectomy cohort (p = 0.02).
A clinical association between neopharyngeal stenosis development and salvage total laryngectomy, when compared with primary total laryngectomy, failed to reach statistical significance (p = 0.21).
Discussion
Total laryngectomy is regarded as a cornerstone in the management of advanced laryngeal cancers that can result in significant physical and psychological morbidity. Complications such as pharyngocutaneous fistulae and neopharyngeal stenosis are well documented and often substantially influence both in-patient admission times and enteral functional outcomes. Therefore, this study aimed to report patient demographics and the rates of pharyngocutaneous fistulae and neopharyngeal stenosis in our centre, along with predisposing factors to their development.
Demographic data
Both primary total laryngectomy and salvage total laryngectomy were performed in a predominantly male population of increased age with the majority of cancers (81 per cent, n = 140) having a laryngeal subsite, and the remaining 19 per cent (n = 33) originating in the hypopharynx.
Primary total laryngectomy was most commonly utilised in the management of advanced laryngeal cancers, with 96 per cent of patients confirmed as having pathological tumour stage 3 (n = 49) or 4 (n = 60) disease. It was also performed in a very limited number of patients with a pathological tumour stage 1 (n = 3) or 2 (n = 2) tumour. Upon further investigation, these patients had either hypopharyngeal tumours with extensive nodal neck disease or had been downgraded from tumour grade 3 to 2 on pathological staging.
Salvage total laryngectomy was performed in the management of recurrent disease, with patients having an earlier primary tumour stage (at recurrence) when compared with primary total laryngectomy. In this cohort, 15 per cent (n = 9) of tumours were stage 1, 32 per cent (n = 19) were stage 2, 34 per cent (n = 20) were stage 3 and 19 per cent (n = 11) were stage 4.
Reconstruction was performed in 33 per cent of cases overall. However, this differed significantly across cohorts, with rates of 18 per cent and 61 per cent for primary total laryngectomy and salvage total laryngectomy, respectively. The favoured type of reconstruction was an anterolateral thigh free flap in the primary total laryngectomy cohort and pectoralis major flap in the salvage total laryngectomy cohort. This is due to anterolateral thigh flaps being used to reconstruct large or total pharyngeal defects in both primary total laryngectomy and salvage total laryngectomy and pectoralis major flaps to provide additional support to pharyngeal closure, more so in salvage total laryngectomy.
Pharyngocutaneous fistulae development
A pharyngocutaneous fistulae is the development of an epithelialised communication between the neopharynx and cervical skin through which saliva and pharyngeal contents can leak. Incidence is variable, with rates from 14.3–29.2 per cent3,Reference Richard, Sancho-Garnier, Pessey, Luboinski, Lefebvre and Dehesdin7,Reference Busoni, Deganello and Gallo8,Reference Paydarfar and Birkmeyer11 reported in the literature. It is the most common major complication following total laryngectomyReference Cavalot, Gervasio, Nazionale, Albera, Bussi and Staffieri12 and has been previously associated with concurrent chemotherapy or radiotherapy, re-operation and, subsequently, increased morbidity.Reference Makitie, Niemensivu, Hero, Keski-Säntti, Bäck and Kajanti13
Our results showed pharyngocutaneous fistulae rates of 6 per cent (n = 7) and 20 per cent (n = 12) in the primary total laryngectomy and salvage total laryngectomy cohorts, respectively (p = 0.005), confirming that this complication is more commonly associated with salvage surgery, chemoradiotherapy and radiotherapy alone.
As expected, it was observed across both cohorts that pharyngocutaneous fistula development occurred most commonly within the first month post-operatively, or more specifically during the immediate post-operative period. This is in agreement with the literature that suggests complications of this nature tend to occur more commonly in the first 12 months following surgery.Reference Sayles and Grant4
Both low pre-operative haemoglobin level and chemotherapy or radiotherapy alone, in addition to poor post-operative nutrition have been previously identified as possible predictors of poor wound healing and pharyngocutaneous fistulae.Reference Paydarfar and Birkmeyer11–Reference Makitie, Niemensivu, Hero, Keski-Säntti, Bäck and Kajanti13
Patients were more likely to develop pharyngocutaneous fistulae following reconstruction in the primary total laryngectomy cohort, and this is likely because of larger and more complex pharyngeal defects. Age, gender, tumour stage and tracheoesophageal puncture were not seen to influence the development of pharyngocutaneous fistulae in either cohort. Additionally, in contrast to the literature, no associations were found between the predisposing factors analysed and the development of pharyngocutaneous fistulae.
Neopharyngeal stenosis and dilatation
Although dysphagia post-laryngectomy can occur because of altered swallowing dynamics or dysmotility of a new free flap graft, neopharyngeal stenosis is a common occurrence and often results in dysphagia and nutritional compromise.Reference Francis, Weymuller, Parvathaneni, Merati and Yueh14 It occurs in 7–19 per centReference Walton, Vellucci, Patel, Jennings, McCammon and Underbrink9,Reference Sweeny, Golden, White, Magnuson, Carroll and Rosenthal10,Reference Francis, Weymuller, Parvathaneni, Merati and Yueh14 of laryngectomy cases, with around 80 per cent occurring in the first year post-operatively.Reference Sweeny, Golden, White, Magnuson, Carroll and Rosenthal10 It is most commonly managed with neopharyngeal dilatations. However, in severe cases, feeding tube insertion may be required and complete stenosis may require resection with reconstruction.
The definition of neopharyngeal stenosis is still the subject of debate. Using the definition of neopharyngeal stenosis as the requirement for at least 1 dilatation and/or feeding tube dependence to avoid under-reporting, the overall rate in the study was 11 per cent, or 19 of 173 patients. Of these, 10 patients required multiple dilatations to maintain their nutritional intake.
Again, in line with the literature, it was seen that the majority of neopharyngeal stenosis development across both cohorts occurred within the first 12 months following surgery.Reference Sayles and Grant4
Although neopharyngeal stenosis rates were higher in the salvage total laryngectomy cohort and a clinical association was thought to exist, this result failed to reach statistical significance (p = 0.21).
No associations between complications were found in the primary total laryngectomy cohort as no patients with previous pharyngocutaneous fistulae developed neopharyngeal stenosis, but an association between previous pharyngocutaneous fistulae and the development of neopharyngeal stenosis was seen in the salvage total laryngectomy cohort (p = 0.01).
• An overall shift towards organ-sparing management was seen in this study, supporting recent trends in the literature
• Primary total laryngectomy continues to be used in the management of locoregionally advanced disease, with salvage total laryngectomy used in the management of recurrent disease
• Although complication rates in this cohort are favourable when compared to the literature, they remain hard to predict
• Pre-operative haemoglobin levels and adjuvant treatments failed to predict pharyngocutaneous fistulae formation, contrasting to the findings of previous studies
• Reconstruction in the primary total laryngectomy cohort was the only factor seen to predispose patients to both pharyngocutaneous fistulae and neopharyngeal stenosis development
• Previous pharyngocutaneous fistulae in the salvage total laryngectomy cohort was seen to predict neopharyngeal stenosis development
Despite the higher rates of reconstruction in the salvage total laryngectomy cohort, an association between reconstruction and the development of neopharyngeal stenosis was observed only in the primary total laryngectomy cohort (p = 0.02). All primary total laryngectomy patients who developed neopharyngeal stenosis had stage 4 hypopharyngeal tumours, and it is thought that the site of disease influenced this outcome because of a more complex resection. No significant associations between other demographics and neopharyngeal stenosis development were seen in either cohort.
Limitations and future study
This study was not without limitations. For example, the inherent difficulties of retrospective data collection and selection bias in treatment choices must be considered.
Other difficulties include the debate over an accurate definition of neopharyngeal stenosis and the comparison to other studies. This highlights a potential area of improvement for future research.
The possibility of ‘sub-clinical’ neopharyngeal stenosis that was not reported or the potential of subjects to die before developing complications could have affected the outcomes. However, previous studies have suggested that up to 80 per cent of strictures occurred in the first year post-operatively,Reference Sweeny, Golden, White, Magnuson, Carroll and Rosenthal10 re-enforcing these results.
There were clinical trends seen towards more advanced primary tumour stages, additional post-operative therapies and the male sex having a higher risk of complications, but none of these reached statistical significance, likely because of the small number of complications observed.
It is apparent that further research into the predictors of pharyngocutaneous fistulae and neopharyngeal stenosis is required to help identify and minimise risk factors. In addition to alcohol abuse, increasing age, male sex, smoking, tobacco and human papilloma virus infection have also been identified as possible risk factors.Reference Torrente, Rodrigo, Haigentz, Dikkers, Rinaldo and Takes15 Additionally, analysis of other parameters such as pre-operative serum albumin levels and nutritional status, post-operative thyroid function, and reflux disease could provide further valuable information.
Conclusion
With these limitations in mind, this study demonstrates a clear trend towards organ-sparing management and a corresponding shift towards salvage total laryngectomy in our region over the past decade. Additionally, outcomes shown here in the form of pharyngocutaneous fistula and neopharyngeal stenosis rates are favourable, even when a more conservative definition of neopharyngeal stenosis is adopted.
Our results show higher complication rates in the salvage total laryngectomy setting. This may have been because of poor tissue quality or a lower physiological reserve of patients following adjuvant therapy. Extrapolating from this and with the shift towards organ-sparing management, a higher incidence of complications and the increased resources to manage these may represent a potential problem in the future.
Additionally, we have shown that complications of total laryngectomy are hard to predict. None of the relationships between complications and predisposing factors were statistically significant.
Despite the shift towards the organ-sparing management of laryngeal cancer, total laryngectomy remains a cornerstone in the management of more advanced cases. Furthermore, it is important that patients are managed by a head and neck multi-disciplinary team and adequately counselled in the pre- and post-operative period about the possible complications associated with total laryngectomy.
Competing interests
None declared








