INTRODUCTION
At present, radiation therapy is an essential part for the treatment of localised breast cancer. Breast conservation therapy (BCT), or also known as lumpectomy followed by radiotherapy, is widely accepted as the standard of treatment for patients with localised breast cancer and ductal carcinoma in situ (DCIS).Reference Veronesi, Cascinelli and Mariani 1 – Reference Clarke, Collins and Darby 4 Aside from that, patients tend to feel more confident about their body images and are more satisfied with BCT compared with mastectomy.Reference Curran, Van Dongen and Aaronson 5
Adjuvant radiotherapy in BCT has been proven to be effective in reducing local recurrence.Reference Veronesi, Cascinelli and Mariani 1 – Reference Clarke, Collins and Darby 4 Standard radiation treatment of the whole breast irradiation is three-dimensional conformal radiotherapy technique (3D-CRT) with images set from a computed tomography (CT) simulator to deliver 45–50 Gy in 25 fractions. However, there are still some acute and long-term toxicities, especially to the skinReference Fernando, Ford and Powles 6 – Reference Cox, Stetz and Pajak 10 and adjacent organs, such as the heart,Reference Gyenes, Rutqvist, Liedberg and Fornander 11 – Reference Giordano, Kuo and Freeman 15 lungReference Kahán, Csenki and Varga 16 – Reference Marks, Bentzen and Deasy 18 and contralateral breast.Reference Boice, Harvry, Blettner, Stovall and Flannery 19 Several studies showed that toxicities were associated with inhomogeneous dose at the target volume and unwanted dose to adjacent organs. For these reasons, several advanced whole breast irradiation techniques have been developed to increase dose homogeneity, improve target volume coverage and reduce dose to organs at risk (OAR).Reference Vicini, Sharpe and Kestin 7 , Reference Pignol, Olivotto and Rakovitch 20 – Reference Popescu, Olivotto and Beckham 24 However, there are few studies of these advanced techniques in Asians,Reference Rongsriyam, Rojpornpradit, Lertbutsayanukul, Sanghangthum and Oonsiri 25 , Reference Tsai, Lin and Lee 26 who have different size and shape of breasts compared with participants reported in previous studies. Moreover, there is no standardisation of the definition of the target volume. Therefore, this could result in unreliable outcomes.
The purpose of this study was to compare the dose distribution of the standard of treatment for whole breast irradiation, 3D-CRT, to the other three advanced techniques such as electronic tissue compensation (ECOMP), inverse intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT) that were available at the King Chulalongkorn Memorial Hospital (KCMH).
MATERIALS AND METHODS
Records of Thai women diagnosed with locally advanced breast cancer or DCIS who had already underwent breast-conserving surgery and whole breast irradiation treatment at the Division of Therapeutic Radiation and Oncology of KCMH from November 2013 to November 2014 were retrospectively reviewed. The authors excluded patients who previously underwent mastectomy or breast augmentation of the ipsilateral or contralateral breast. The number of patients in this study (sample size) was calculated based on a pilot study in order to achieve the adequate number for statistical analysis. We used the quota technique for the sampling method. The images from the GE Lightspeed RT CT (LightSpeed RT GE Medical system, Waukesha, WI, USA) simulation that had been used for whole breast irradiation of each patient were used for contouring target volumes, OAR and re-planning the whole breast irradiation by four techniques. The review of medical records in this study was approved by the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (approval no. 349/56).
Target volumes and OAR
Clinical target volume (CTV), planning target volume (PTV) and OAR, which were heart, ipsilateral lung, contralateral lung and contralateral breast, were contoured by the author from the CT simulation images. The definition of the CTV boundaries was based on the Radiation Therapy Oncology Group (RTOG) 27 (see Supplementary Table 1). For DCIS and invasive cases that had negative nodes, the author contoured the CTV for whole breast irradiation. For cases with positive nodes, the author contoured CTV for whole breast and chest wall irradiation. Regional nodes were not contoured in this study. PTV was defined according to the RTOG 1005 protocol 28 for whole breast irradiation, which was CTV +7 mm 3D expansion but excluded the part that extended posteriorly into the anterior surface of the ribs (bony thorax and lung), cross midline, extended anteriorly to the outside of the body and excluded 5 mm of tissue under the skin (Figures 1 and 2). For the whole breast and chest wall irradiation, the authors adapted the PTV from the RTOG 1005 protocol by excluding part of the PTV that extended posteriorly towards the heart but kept the border that extended into chest wall and lung. The other borders were the same as for the whole breast irradiation PTV (Figures 3 and 4).

Figure 1 Target volumes and organs at risk for whole left breast irradiation; planning target volume (red line), clinical target volume (brown line), contralateral breast (magenta line), left lung (yellow line), right lung (green line).

Figure 2 Target volumes and organs at risk for whole right breast irradiation; planning target volume (red line), clinical target volume (brown line), contralateral breast (orange line), left lung (yellow line), right lung (green line).
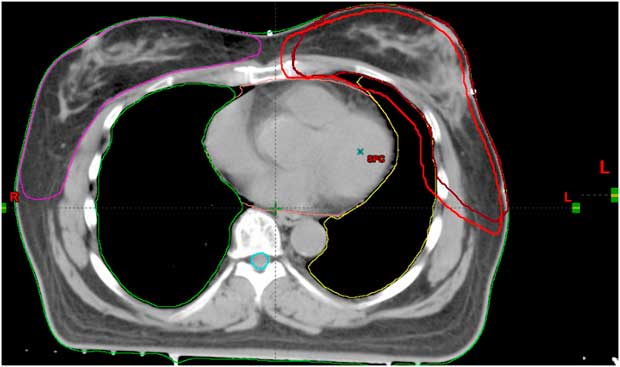
Figure 3 Target volumes and organs at risk for whole left breast and left chest wall irradiation; planning target volume (red line), clinical target volume (brown line), contralateral breast (magenta line), left lung (yellow line).
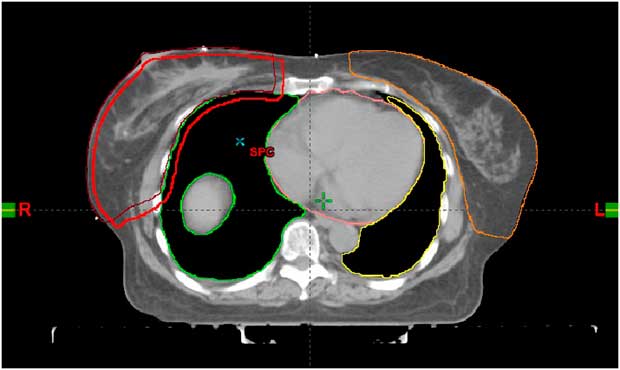
Figure 4 Target volumes and organs at risk for whole right breast and right chest wall irradiation; planning target volume (red line), clinical target volume (brown line), contralateral breast (orange line), left lung (yellow line).
Irradiation techniques, calculation and dose prescription
Each patient was re-planned by using all four techniques: standard 3D-CRT, ECOMP, inverse IMRT and VMAT. The total dose of radiation was 50 Gy in 25 fractions with 6 MV photon energy which was prescribed to PTV. The skin flash was used in ECOMP technique. All treatment plans were calculated with Eclipse treatment planning software (version 11.0.31; Varian Medical Systems, Palo Alto, CA, USA). The radiation fields for each technique are described as follows:
-
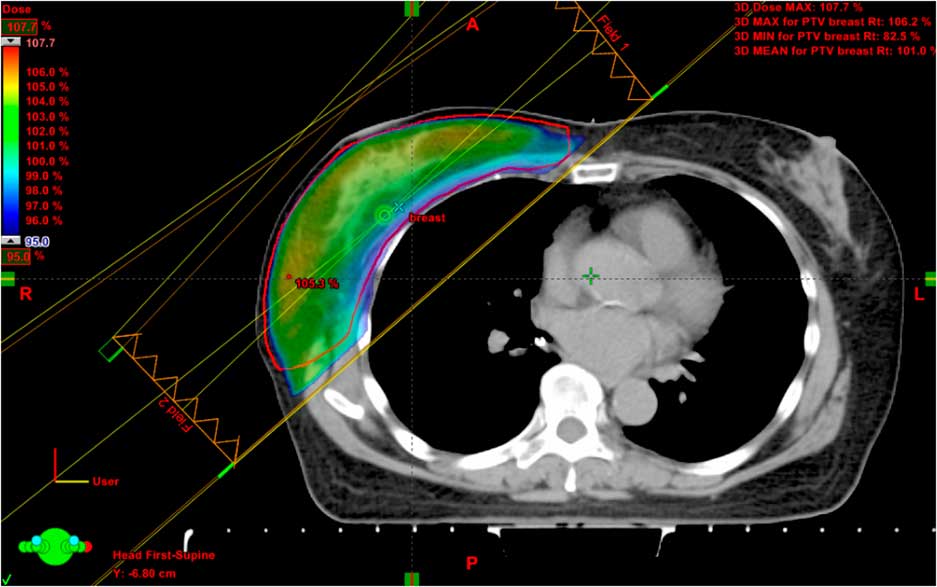
(1) Standard 3D-CRT was planned by the same author that contoured target volumes and OAR. The plans consisted of two tangential fields. The angles between these beams were chosen in such a way that the posterior border of the lateral and medial fields were non-divergent. The optimal wedge angles and multileaf collimators (MLC) were chosen based on the dose distribution and calculated with inhomogeneity correction according to the standard protocol (Figure 5).
-
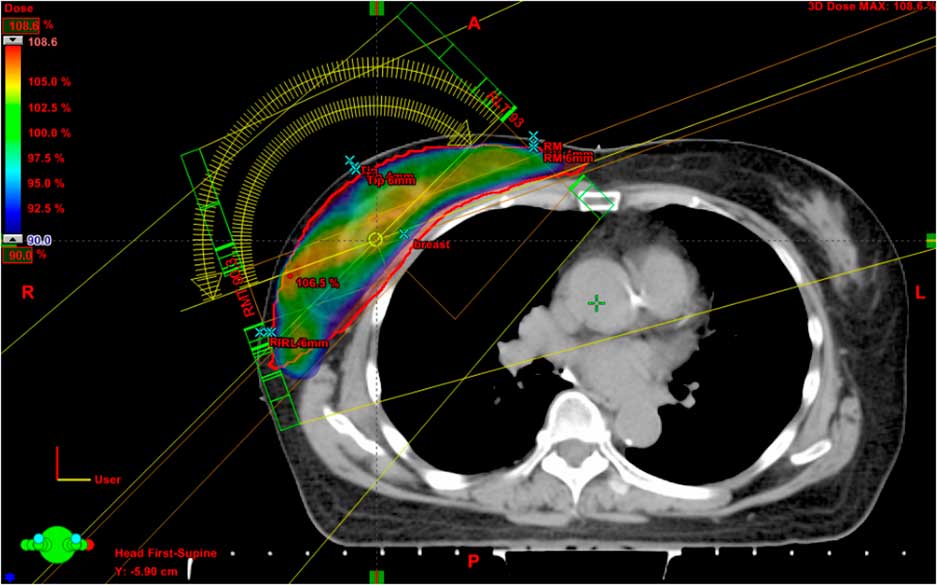
(2) ECOMP was planned by the same author as 3D-CRT technique. The plans consisted of two tangential fields. Tissue compensation was used to correct the dose inhomogeneity which could occur from an irregular surface of the patient’s breast. The fluent distribution was calculated by ray tracing and determining the amount of missing tissue along each ray line. The fluent maps were converted to leaf sequences for dynamic MLC (DMLC) delivery (Figure 6).
-
(3) Inverse IMRT was planned by a physicist. The plans composed of five co-planar fields. The first two out of five fields were tangent, but not opposing. Gantry angles were adjusted as appropriate to cover PTV and avoid unnecessary normal tissue. Dose–volume constraints were inputted according to RTOG 1005 protocol (Table 1). The plan was optimised by The Eclipse Planning System, using inverse planning with DMLC (Figure 7).
-
(4) VMAT was planned by the same physicist who planned IMRT technique. Two co-planar arcs were inserted and adjusted as they needed to cover the PTV and avoid dose to the normal tissues. The VMAT plans were generated with a gantry angle sampling frequency of 2°, maximum MLC leaf motion between gantry samples of 2·5 cm and the gantry speed of 4·8°/second. Dose–volume constraint was inputted according to the RTOG 1005 protocol (Table 1) and then optimised by The Eclipse Planning System (Figure 8).
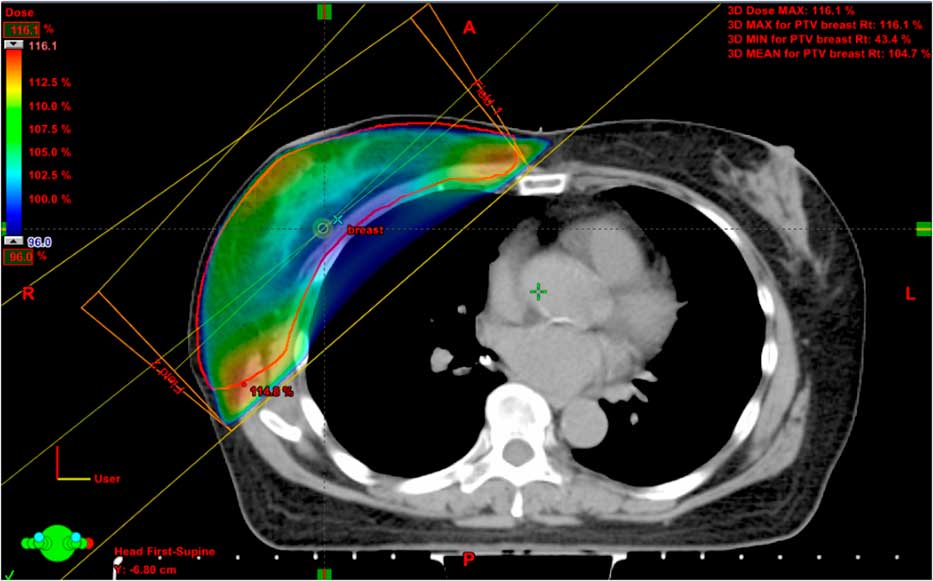
Figure 5 The dose colour wash representing 95% of the prescribed dose and beam alignment of three-dimensional conformal radiotherapy technique.
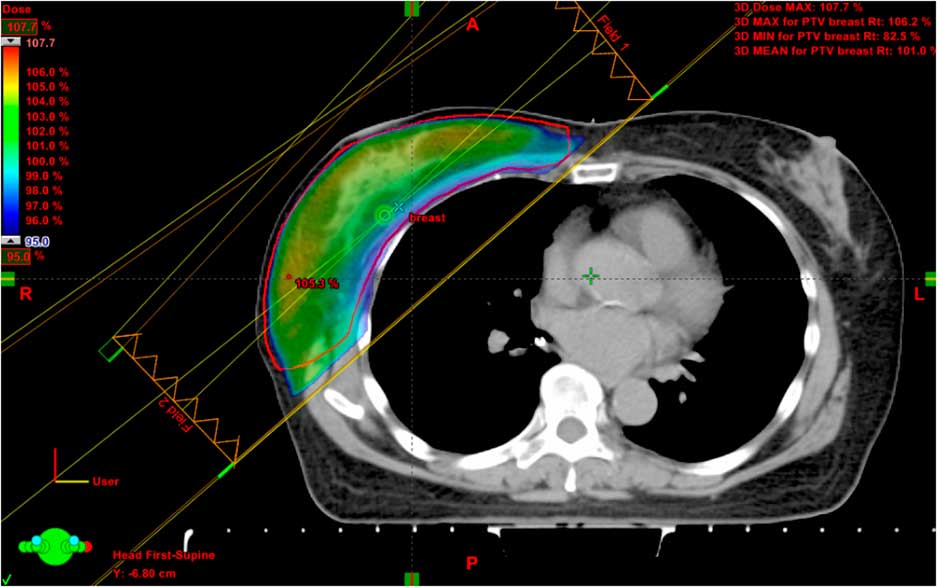
Figure 6 The dose colour wash representing 95% of the prescribed dose and beam alignment of electronic compensator (ECOMP) technique.
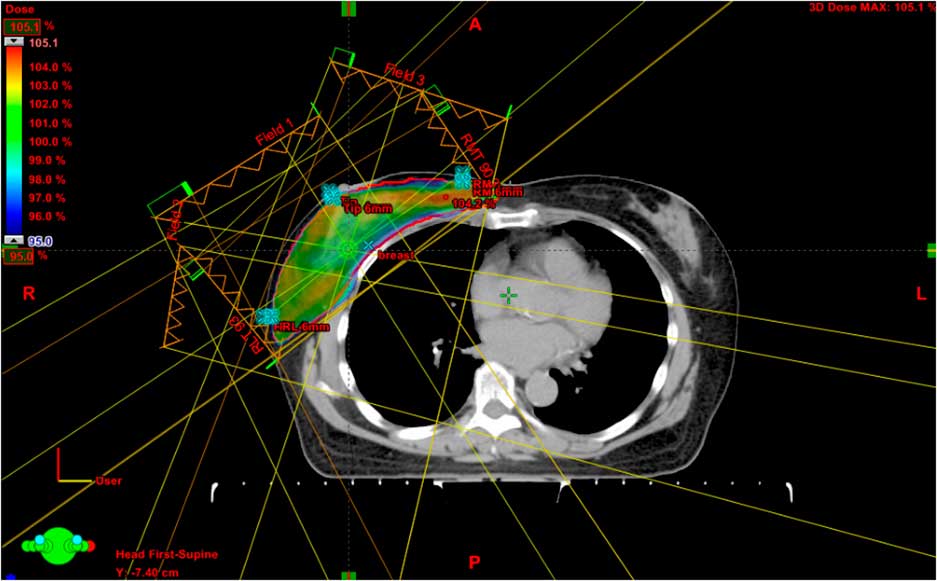
Figure 7 The dose colour wash representing 95% of the prescribed dose and beam alignment of intensity-modulated radiation therapy technique.

Figure 8 The dose colour wash representing 95% of the prescribed dose and beam alignment of volumetric-modulated arc therapy technique.
Table 1 Dose–volume histogram constraint for optimisation

Abbreviations: PTV, planning target volume; Dmax, maximum dose.
Data analysis
Dose–volume histograms (DVHs) were generated and recorded for PTV size, volume enclosed by the 95% isodose (V95%), PTV maximum dose (Dmax, PTV2%), PTV minimum dose (Dmin, PTV98%), irradiated breast size, mean heart dose (MHD), heart V30 (percentage of the volume receiving >30 Gy), heart V25, mean lung dose (MLD), lung V20, mean ipsilateral lung dose (MILD), mean contralateral lung dose (MCLD), mean contralateral breast dose (MCBD), body volume enclosed by 95% isodose and monitor units (MU).
The primary outcome of this study was the radical dose homogeneity index (HI), which was defined as the ratio of Dmin to Dmax of the PTV (HI=Dmin/Dmax). The secondary outcomes were conformity index (CI), MHD, heart V30, heart V25, MLD, lung V20, MILD, MCLD, MCBD and MU. The CI was defined as the fraction of the PTV that is enclosed by the reference dose (95%) multiplied by the fraction of the total body volume (from the CT simulation) which included the 95% isodose (CI=PTV95%/PTV×PTV95%/V95%).
All results were analysed by IBM SPSS statistics 20 program, using repeated-measures analysis of variance test with a significance level of 0·05.
RESULTS
There were 25 patients in this study. The age of the participants ranged from 40 to 74 years. Mean irradiation of the breast size was 804·57 cm3 and ranged from 423 to 1,744 cm3. Median breast size was 646 cm3. Number of patients were classified according to TNM (primary tumor, nodes, metastasis) stage and PTV as described in Tables 2 and 3, respectively. The primary and secondary outcomes are shown in Table 4.
Table 2 TNM stage of patients according to AJCC 7th edition

Abbreviation: TNM, primary tumor, nodes, metastasis stage; DCIS, ductal carcinoma in situ.
Table 3 The target volumes and sides of whole breast irradiation

Table 4 Homogeneity index (HI), conformity index (CI) and dose to organs at risk of three-dimensional conformal radiotherapy (3D-CRT), electronic compensator (ECOMP), inverse intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT) techniques

Abbreviations: MHD, mean heart dose; MLD, mean lung dose; MILD, mean ipsilateral lung dose; MCLD, mean contralateral lung dose; MCBD, mean contralateral breast dose; MU, monitor units.
HI and CI
The HI outcome for the ECOMP and IMRT techniques were significantly higher than the 3D-CRT technique (p<0·001 for both comparisons). The HI of VMAT and 3D-CRT were hardly different (p=0·807) and also observed this in comparing IMRT and ECOMP (p=0·858). However, the ECOMP and IMRT techniques had significantly higher HI when compared with the VMAT technique (p<0·001 and p=0·001, respectively).
For the CI outcome, the ECOMP, IMRT and VMAT techniques were significantly higher than the 3D-CRT technique (p<0·001 for all comparisons). IMRT and VMAT techniques had significantly higher CI compared with the ECOMP technique (p<0·001). When comparing between VMAT and IMRT, the CI was hardly different (p=0·89).
Heart dose
For the MHD, this was found to be significantly lower when the ECOMP technique was used compared with the 3D-CRT (p<0·001) and VMAT techniques (p=0·001). ECOMP also had lower MHD compared with IMRT but not statistically different (p=0·053). The 3D-CRT technique had non-significantly lower MHD compared with the VMAT technique (p=0·202). The MHD for the IMRT technique was significantly lower than the VMAT (p=0·001). But when the MHD for the IMRT was compared with the 3D-CRT, this was found to be comparable (p=0·715).
For the heart V25 outcome, this was found to be significantly lower when the ECOMP technique was used compared with the 3D-CRT (p=0·001). IMRT technique had statistically significant lower heart V25 compared with the 3D-CRT, ECOMP and VMAT techniques (p=0·001, 0·021 and 0·049, respectively). VMAT technique had statistically significant lower heart V25 compared with the 3D-CRT technique (p=0·014). The V25 of the VMAT was non-statistically lower than ECOMP (p=0·323).
The heart V30 was significantly lower when the ECOMP technique was used compared with the 3D-CRT technique (p=0·001). The IMRT technique had statistically significant lower heart V30 compared with the 3D-CRT and ECOMP techniques (p<0·001 and p=0·005, respectively). The heart V30 was non-statistically higher in VMAT compared with IMRT (p=0·181). The VMAT technique had statistically significant lower heart V30 compared with the 3D-CRT technique (p=0·002). When the VMAT was compared with the ECOMP, VMAT tended to have statistically lower V30 (p=0·051).
Lung dose
For MLD, this was found to be significantly lower when the ECOMP technique was used compared with the 3D-CRT, IMRT and VMAT techniques (p<0·001 for all comparisons). The MLD of 3D-CRT was comparable with IMRT (p=0·557) and non-statistically lower compared with VMAT (p=0·051). In addition, the MLD of IMRT was non-statistically lower than VMAT technique (p=0·058).
As for the lung V20 outcome, this was found to be significantly lower when the IMRT technique was used compared with the 3D-CRT (p=0·001), ECOMP (p=0·025) and VMAT (p=0·006). ECOMP technique had statistically significant lower lung V20 compared with the 3D-CRT (p=0·006). VMAT technique had comparable lung V20 when compared with the 3D-CRT technique (p=0·890).
MILD was significantly lower when the ECOMP technique was used compared with the 3D-CRT (p<0·001) and the VMAT (p=0·674). IMRT technique had statistically significant lower MILD compared with the 3D-CRT technique (p=0·001). The MILD was comparable between the IMRT and the ECOMP (p=0·587) and VMAT (p=0·209). The VMAT technique had statistically significant lower MILD compared with the 3D-CRT (p=0·012).
For MCLD, this was significantly lower when ECOMP technique was used compared with the 3D-CRT, IMRT and VMAT techniques (p<0·001 for all comparisons). 3D-CRT technique had statistically significant lower MCLD compared with the IMRT and VMAT techniques (p<0·001 for both comparisons). The IMRT technique had statistically significant MCLD compared with the VMAT technique (p=0·048).
Contralateral breast dose
As for the MCBD, it was significantly lower when the ECOMP technique was used compared with the 3D-CRT (p=0·001), IMRT (p<0·001) and VMAT (p<0·001) techniques. The 3D-CRT technique had statistically significant lower MCBD compared with the IMRT (p=0·003) and VMAT (p<0·001) techniques. IMRT technique had statistically significant lower MCBD compared with the VMAT technique (p<0·001).
MU
The MU of 3D-CRT were statistically lower than other three techniques (p<0·001 for all comparisons). The MU of ECOMP were also statistically lower than IMRT and VMAT techniques (p<0·001 for both comparisons), whereas the MU of IMRT were statistically higher than other techniques (p<0·001 for all comparisons).
DISCUSSION
As whole breast irradiation is the mainstay treatment for localised breast cancer and DCIS, several radiation techniques have been studied to reduce normal organ toxicity. Even though 3D treatment planning has been used widely, inhomogeneity of the target volume, inconformity and dose to adjacent organs are still problematic. As a result of this, many advanced techniques for whole breast irradiation have been developed. However, this study is the first to compare the standard treatment 3D-CRT with the three advanced techniques; ECOMP, IMRT and VMAT.
The results in this study also supported previous reports that IMRT was superior to the 3D-CRT. However, the HI in this study was lower than the results from Rongsriyam et al.Reference Rongsriyam, Rojpornpradit, Lertbutsayanukul, Sanghangthum and Oonsiri 25 and Popescu et al.Reference Popescu, Olivotto and Beckham 24 This discrepancy may be due to the different sizes of the CTV and PTV. The HI of previous studies and this study are shown in Table 5. In addition, only few studies have compared ECOMP or VMAT with the 3D-CRT. A whole breast irradiation study by Caudell et al.Reference Caudell, De Los Santos and Keene 21 compared ECOMP, tomotherapy (TOMO) and IMRT techniques. The results showed that ECOMP was superior in lowering dose to the lung, heart, contralateral breast compared with the IMRT and TOMO techniques which was consistent with the outcomes of comparing ECOMP with IMRT in our study.
Table 5 Homogeneity index (HI) of this study and previous studies

Abbreviations: 3D-CRT, three-dimensional conformal radiotherapy; ECOMP, electronic compensator; iMRT, inverse intensity modulated radiotherapy; VMAT, volumetric-modulated arc therapy; fIMRT, forward intensity modulated radiotherapy; CR, conventional radiation therapy.
When several techniques are compared with each other, interpretation of the data may be difficult because other considerations have to be taken into account. For example, most of the whole breast irradiation studies were conducted in the Western countries. Therefore, results from Caucasians may not be applicable to Asians who have different breast sizes and shapes. Like the study by Popescu et al.,Reference Popescu, Olivotto and Beckham 24 their mean PTV was larger than ours. For a study conducted in China by Zhang and Zheng,Reference Zhang and Zheng 30 the results showed that HI and CI of direct machine parameter optimisation (DMPO) IMRT was the highest compared with conventional radiation therapy and conformal radiation therapy (CRT), consistent with our study. The mean size of the target volumes from previous studies are shown in Table 6.
Table 6 Breast volume, clinical target volume (CTV), planning target volume (PTV) and target delineation of this study and previous studies
Abbreviations: RTOG, Radiation Therapy Oncology Group; CT, computed tomography.
Another factor that may affect the interpretation of the data is the CTV. The authors noticed that the definition of CTV was different between several whole breast irradiation studies (i.e., glandular breast plus margin, irradiated volume, breast parenchyma, etc.), which could result in high inter-observer variation (Table 6). As a result of this, the RTOG conducted an atlas for contouring breast, chest wall and regional nodes for breast cancer irradiation. 27 The authors decided to use RTOG contouring atlas to standardise the CTV contouring to lower the variabilities among the assessors. However, PTV was not defined in the RTOG atlas, thus the authors adapted the definition of it from the RTOG 1005 protocol. 28 Nevertheless, the target volumes in this study tend to be larger than clinical irradiated volumes from authors’ hospital which use 3D anatomical landmarks. Also, in 2013, the Danish Breast Cancer Cooperative GroupReference Nielsen, Berg and Pedersen 29 established a consensus for delineating target volume and OAR for breast cancer. There are some minor differences in cranial, ventral and lateral boundaries, compared with the RTOG atlas, whereas for the other boundaries the definitions used were similar (see Supplementary Table 2).
Aside from that, the most common adverse effect of the whole breast irradiation is skin toxicity. A randomised clinical trial by Pignol et al.Reference Pignol, Olivotto and Rakovitch 20 showed that IMRT could significantly improve the dose distribution, resulted in lowering the proportion of moist desquamation which was correlated with the pain score, global health status scale and breast status scale. Besides this, Zaghloul et al.Reference Zaghloul, Rashed, Shaukat, Rostom and Badawy 31 compared the conventional physical wedges or dynamic wedges technique with the multiple fields in field (MFIF) technique, in which the results concurred that MFIF technique had higher HI and also reduced skin toxicity. This correlation of HI and clinical outcome may be applicable to our study which means that IMRT and ECOMP may cause less skin toxicity compared with 3D-CRT.
Likewise, cardiotoxicity is another serious adverse effect of breast irradiation, especially for the left-sided breast cancer. A large population-based case–control study by Darby et al.,Reference Darby, Ewertz and McGale 14 showed an increase of 7·4% in rates of major coronary events when the MHD is increased by 1 Gy of the MHD. This can be rectified by using advanced techniques which could maintain low dose to OAR. A study by Tsai et al.Reference Tsai, Lin and Lee 26 showed that VMAT technique could maintain low dose to OAR, including MHD, heart V5, V10, V15 and V30. Our study showed consistent results. The heart V30 was lower in advanced techniques. However, only the ECOMP technique had statistically significant lower MHD than the 3D-CRT. These discrepancies may be due to the different PTV size which mean PTV from Tsai et al. and our study were 562·1 and 870 cm3, respectively. As both studies used the RTOG atlas for contouring, the difference in PTV size could have resulted from including the chest wall in our study for patients with positive nodes. These outcomes can be extrapolated to indicate that the IMRT and VMAT could reduce high dose to the heart, regardless of the PTV size, but unable to lower the low dose for the large PTV. On the other hand, ECOMP could reduce both low and high doses in any PTV size.
To avoid cardiotoxicity, several techniques have been proposed. A study conducted by Swanson et al.Reference Swanson, Grills, Ye, Entwistle, Teahan and Letts 32 showed that moderate deep inspiration breath hold (DIBH) could significantly decreased 40% of the cardiac mean dose compared with the free breathing (FB) technique. In this study, only sets of free-breathing CT simulation images were collected. Therefore, we could not evaluate the dosimetry of whole breast irradiation of breath hold technique. However, this technique has been implemented in the authors’ hospital for left-sided breast cancer cases with image guide radiation therapy to match the skin surface on the treatment days and skin surface from the CT simulation. As patients who were able to use this technique had to hold deep inspiration for a period, they had to have good performance status and required short treatment time.
Besides the heart injuries, other side effects can include the lung sequelae after breast irradiation. A study by Kahán et al.Reference Kahán, Csenki and Varga 16 showed that the radiation dose was positively correlated with the risks of developing pneumonitis or fibrosis. Our study showed that the ECOMP had the lowest MLD compared with other techniques. However, for MILD, IMRT and VMAT had lower dose compared with ECOMP. In addition, the lung V20 was lower when the ECOMP and IMRT techniques were used compared with the 3D-CRT. But for the MCLD, the IMRT and VMAT techniques had higher dose compared with the 3D-CRT. These results corroborates the data reported by Popescu et al.Reference Popescu, Olivotto and Beckham 24 that IMRT and VMAT techniques were able to decrease the lung V20 when compared with the 3D-CRT. Along the similar lines, Rongsriyam et al.Reference Rongsriyam, Rojpornpradit, Lertbutsayanukul, Sanghangthum and Oonsiri 25 reported that the MILD was lower when the IMRT technique was used compared with the 3D-CRT but at the same time it also increased the MCLD.
Moreover, other factors such as the MU are equally important. In clinical practice, the MU are correlated with the treatment time. In this study, ECOMP and IMRT had statistically significant higher primary outcome for HI when compared with the other techniques. However, the mean MU of ECOMP was much less than IMRT. This may imply that the treatment time for ECOMP could be reduced to half of that used in the IMRT technique which was consistent with the findings from our clinical practice. Not only shorter treatment time, but ECOMP also took shorter time for treatment planning comparing with IMRT and VMAT. Therefore, ECOMP may be an optimal option for advanced technique in whole breast irradiation.
The other factor that needs to be considered is the dose intensity. So far, all of the advanced techniques in this study used DMLC to adjust for the dose intensity in a specific area of PTV. As the breast continuously moves, directly related to the respiratory cycle, an accurate dose to the breast tissue is of concern that it may not be the same as the isodose level in the treatment planning. One centimetre-skin flash tool was used for this treatment planning to cover the anterior part beyond the PTV for the inspiration cycle during ECOMP. The opened fields of MLC were significantly larger in ECOMP technique compared with the IMRT and VMAT. Thus, ECOMP may be less affected by the free breathing compared with the IMRT and VMAT. The ideal method to solve this problem is probably DIBH. However, for advanced techniques such as IMRT and VMAT, the patients are required to hold their breaths for a long period which may not be practical and achievable.
In conclusion, ECOMP, IMRT and VMAT were superior to the 3D-CRT. The advanced techniques show promising use and maybe preferred over the standard of treatment. However, this research is a dosimetric study, hence the data from the DVH may be different from the clinical situation. Therefore, additional study is warranted to compare between these four techniques in real patients.
Acknowledgements
The authors are thankful to Associate Professor Sivalee Suriyapee and Ms Swe Swe Lin, radiation physicists, who gave advices about optimising IMRT and VMAT plans, Ms Buntipa Netsawang, who gave advice about statistical analysis, and radiation oncology team of KCMH who kindly supported us in this research study.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1460396917000243