INTRODUCTION
A cancer diagnosis and the subsequent complex treatments are often associated with fear and psychosocial distress (Mishel, Reference Mishel1984; Sherman et al., Reference Sherman, Simonton and Latif2009). Psychosocial care for patients with cancer has been an important component of healthcare in oncology for more than 25 years. In 1997, the National Comprehensive Cancer Network (NCCN) established a panel that included oncologists, nurses, social workers, psychiatrists, psychologists, and a member of the clergy who developed specific guidelines related to distress screening and access to appropriate psychosocial care (National Comprehensive Cancer Network, 2010). These guidelines were based on a body of psychosocial literature that dates back to 1980. More recently, the Institute of Medicine (IOM) published a report in 2007, “Cancer Care for the Whole Patient,” which elaborated upon the NCCN guidelines by recommending a model of care that included distress screening, psychosocial needs, treatment plans, referral to appropriate resources, and evaluation of this entire process for effectiveness (Institute of Medicine, 2008). Clinicians often expect all patients to respond with the same amount and type of distress to a diagnosis of multiple myeloma. However, the variation in levels of and sources of distress is significant, and patients who cannot adapt to their clinical circumstances present with myriad psychological and social problems, increasing the burden on healthcare teams in these settings.
For nearly a third of newly diagnosed cancer patients, the vulnerability associated with these problems (including emotional and mental health problems, developmental problems, financial stress, lack of or inadequate health insurance, and reduced employment and income) generates significant psychological distress that may not manifest itself to the healthcare team until the patient reaches an observable crisis event (Weisman, Reference Weisman1976; Institute of Medicine, 2008). To prevent crisis events and proactively identify patients with psychological distress, the Commission on Cancer (CoC) of the American College of Surgeons (ACoS) in 2012 established new standards of care that require distress screening (Standard 3.2) and survivorship care plans (Standard 3.3) to create a “patient-centered focus” (American College of Surgeons, 2012). Cancer centers and programs are now planning to meet these standards by 2015. Guidance for institutions to achieve multidisciplinary collaboration among healthcare team members will be needed to facilitate achieving these goals in timely fashion.
In the case of patients with multiple myeloma, the complex treatment pathway and long duration of this chronic yet life-threatening disease with repeated relapses are two factors that can lead to psychosocial distress for patients. Many newly diagnosed multiple myeloma patients experience high levels of fatigue and pain, resulting in low levels of physical well-being, and these symptoms can be further exacerbated by treatment, osteolytic lesions, and recurrent infections (Sherman et al., Reference Sherman, Simonton and Latif2004). Bone pain and fractures are not uncommon. Given that a significant number of multiple myeloma patients are older at the time of diagnosis, the severity of these symptoms can be quite debilitating. For these older patients, intensive treatments such as stem cell transplantation (SCT) may appear overwhelming or unrealistic. If treatment progresses to SCT, patients with multiple myeloma often identify a family caregiver who can provide a high level of onsite care during treatment and recovery. An SCT and the level of care required can dramatically impact the employment status of both the patient and the family caregiver. As a result, the economic stability of these families can be severely compromised (Talley et al., Reference Talley, McCorkle, Baile and McCorkle2012). Thus, fatigue, pain, long recovery, and potential economic hardship are potential concerns for patients with multiple myeloma and their caregivers.
As a result, MM patients are confronted by an array of significant concerns related to bone health, health maintenance, mobility and safety, sexual dysfunction, and renal health (Bilotti et al., Reference Bilotti, Faiman and Richards2011). Virtually all MM patients develop osteolytic bone lesions that can produce poor circulation, blood clots, muscle wasting, and decreased performance status. Monitoring of bone complications is essential, and promotion of exercise, adequate nutrition, vitamin and mineral supplements, and planned radiographic examinations can prove to be valuable (Miceli et al., Reference Miceli, Colson and Faiman2011). In turn, these interventions can enable the patient to maintain mobility, reduce risk of falling, and to maintain daily activities (Rome et al., Reference Rome, Jenkins and Lillibey2011).
Even as early as the initial diagnosis, MM patients can present with complaints of fatigue, pain, insomnia, and decreased performance status that can result in a depressed mood (Coleman et al., Reference Coleman, Goodwin and Coon2011). Further, this symptom burden can also include peripheral neuropathy, a frequent side effect associated with bortezomib (Broyl et al., Reference Broyl, Jongen and Sonneveld2012).
For patients who progress to autologous transplantation, higher levels of depression can be observed post-transplant, but reductions in pain and increased social functioning are also possible (Sherman et al., Reference Sherman, Simonton and Latif2009). In general, the cumulative effect of high-dose chemotherapy followed by autologous transplant produces lower levels of quality of life, and this is particularly true among older patients (Slovacek et al., Reference Slovacek, Slovackova and Pavlik2008). Furthermore, cognitive abilities—including learning, memory, executive function, and motor function—can also be adversely affected. Nearly 50% of these patients experience one or more cognitive deficits (Jones et al., Reference Jones, Vichaya and Wang2013). Throughout all of these complex treatments and related side effects and symptoms, family caregivers simultaneously experience their own levels of distress and their reactions to each new symptom. A reliable caregiver is a prerequisite for eligibility for transplantation, but caregivers face many of the same challenges as MM patients do. Caregivers must understand complex treatment information, perform technical care such as catheters or injection, and assist the patient in the multiple activities of daily living (Kurtin et al., Reference Kurtin, Lilleby and Spong2013).
While there exists a clear need for targeted psychosocial care for the multiple myeloma patient and their caregivers, there is relatively little or no literature around this topic. In the present paper, we describe some of the unique challenges that a diagnosis of multiple myeloma affords, provide a roadmap for psychosocial care for these patients, and, finally, propose a novel model of care that promotes active engagement of both the patient and their family caregivers across the continuum of the disease.
Unique Combination of Psychosocial Needs for Patients With MM and Their Caregivers
One of the unique features of multiple myeloma is that it is commonly preceded by a diagnosis of monoclonal gammopathy of undetermined significance (MGUS), which is typically asymptomatic. Indeed, just a small percentage (1% per year) of these patients have a chance of progression to full-blown symptomatic multiple myeloma (Merlini & Palladini, Reference Merlini and Palladini2012). Not surprisingly, the stress of being diagnosed with a precursor disease that can potentially progress to a fatal disease may lead to significant stress in many patients and their families. Most of these patients call this period “watch and worry,” instead of using the term “watch and wait,” which physicians employ to describe the lack of treatment and follow-up in these patients. In some patients with smoldering myeloma, the risk of progression is much higher, and the rate of progression can rise to 50% within 2 years. Many of these patients start to worry about the impending diagnosis of a terminal illness like multiple myeloma and the side effects related to therapeutic interventions. These patients feel that the “other shoe will drop” every time they see their oncologists. In addition, patients may have the label of cancer written in their medical records, which can have consequences for their life and health insurance, and at work. Therefore, though these patients seem healthy and are told to live their lives without the consequences of therapy or the symptoms related to the disease itself, patients with multiple myeloma suffer significant psychosocial stresses that have to be identified early and recognized by a medical professional.
Like with other cancers, multiple myeloma affects all members of a family when a member has been diagnosed. Over the past decade, family caregivers have assumed a higher level of support and responsibility in the daily care of patients with cancer. While many caregivers may adapt to this critical role, others may struggle to meet the demands of maintaining stability within the family and simultaneously providing the necessary level of care. What makes multiple myeloma somewhat unique to other cancer diagnoses is that family caregivers may be subject to “psychosocial fatigue,” where the culmination of stressors from years of medical caregiving results in significant strain with psychological and social consequences. It can be particularly challenging given that the disease typically afflicts the elderly, for whom younger family members may live far away and have caregiving responsibilities to their own family. Family caregivers benefit from ongoing monitoring and support, so that their critical contribution to the overall wellness of the patient can be sustained. However, the healthcare team should be aware of significant variations that exist in family functioning (Olsen et al., Reference Olsen, McCubbin and Barnes1983). Not all families have the same ability to provide the type of care that is required. Families should be assessed for their level of functioning so that the healthcare team can set appropriate expectations of patient care for each individual family (Fobair & Zabora, Reference Fobair and Zabora1995). Another important area of assessment is the family's developmental stage; this may influence the ability and availability of caregivers (Given et al, Reference Given, Given, Kozachik and Given2003).
Another unique feature of multiple myeloma is that, while it is relatively rare, incidence rates among African Americans are about twice those among whites in the United States (Siegel et al, Reference Siegel, Naishadham and Jemal2013). Rates among Hispanics are similar to those among whites, whereas rates among Asian/Pacific Islanders are substantially lower. The reasons for the excess of disease among African Americans or the variations among diverse populations are not known. African Americans and other minorities are typically underrepresented in clinical research (Redwood & Gill, Reference Redwood and Gill2013). Attention is required to understand the needs of culturally diverse communities in efforts to ensure that all patients have access to the highest quality of care and social and emotional support.
Identifying Resources to Reduce Distress
Multiple myeloma generates challenges and complex problems for every patient and their family. Healthcare professionals should apply a theoretical model to guide the assessment of these problems. Stress model theory (SMT) suggests that an individual must experience a series of cognitive appraisals (primary and secondary appraisals) related to a crisis event, such as a cancer diagnosis, as well as the level of distress associated with the diagnosis (Lazarus & Folkman, Reference Lazarus and Folkman1984). Before the patient and family can reduce the distress associated with a cancer diagnosis, the patient and each family member must develop a personal meaning with respect to the diagnosis. Primary appraisal helps the patient or family member define what the crisis event means at this point in his/her life. Resources are critical for the individual to define a crisis event. Since many studies have demonstrated the relationships between distress and resources, distress is an appropriate marker for identification of patients at high risk for having limited resources.
Stress model theory postulates that each patient possesses a number of internal and external resources. Examples of internal resources include personality, level of optimism, ability to solve problems, and spirituality. External resources are often social supports, like the family. If social supports are adequate and available, the individual possesses a greater likelihood of defining this event in a more positive manner. These internal and external resources not only facilitate definition of the crisis, but also promote the development of a secondary appraisal, leading to effective strategies for responding to the specific crisis event (Lazarus, Reference Lazarus1991). Failure to respond to the demands of a crisis event and to solve the related complex problems may result in significant levels of emotional distress, which will cause disruptions in daily functioning. However, most patients or caregivers will attempt to conceal their distress from their families and those around them. This model recommends improving the problem-solving resource by the creation of an effective “problem-solving team” through integration of the family into this intervention. The biopsychosocial model could also be considered, which stipulates that psychological status and intervention can impact immune function and health outcomes as well as quality-of-life outcomes (Suls & Rothman, Reference Suls and Rothman2004).
There is a high level of probability that newly diagnosed multiple myeloma patients with limited resources will experience significant distress at the time of diagnosis. If this distress can be detected much earlier along on the patient's journey, targeted psychosocial interventions could be offered at a more appropriate time in the course of care, such as at the time of diagnosis. If emotional distress is undetected and untreated, unhealthy behaviors can occur, satisfaction with life decreases, and inappropriate use of healthcare resources may be the result (Institute of Medicine, 2008; Carlson et al., Reference Carlson, Angen and Cullum2004; DiMatteo, Reference DiMatteo2004). Patients and families over time can become overwhelmed, impacting decision making and problem solving, and the overall response to the demands of the illness can be compromised. As a result, patients and families can be at risk for increased distress and diminished quality of life. Therefore, evidence-based interventions are essential in order to allow multiple myeloma patients and their families to manage this disease across the disease continuum (Toseland et al., Reference Toseland, Blanchard and McCallion1995a ).
Roadmap for Psychosocial Care in Multiple Myeloma
We propose here the critical points of screening for distress and opportunities for personalized psychosocial care (see Figure 1). Active engagement of the patient and family in the treatment plan is critical to optimal treatment outcomes. Patients and families can be engaged through active communication with the healthcare team, education about the disease and its treatment, screening for psychosocial distress, referral to appropriate psychosocial resources, and follow-up to ensure that patient needs and concerns have been adequately addressed. Screening, referral, and follow-up for distress should occur throughout the disease continuum, but at the very least we believe it is critical to screen for distress at the following pivotal transition points using a validated, consistent approach.
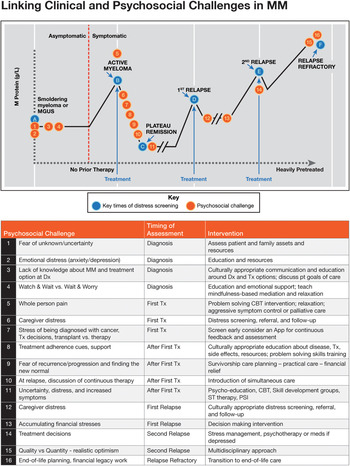
Fig. 1. (Color online) Linking clinical and psychosocial challenges in multiple myeloma.
Diagnosis
The point of diagnosis or shortly thereafter is an important time for assessing the psychosocial support needs of patients and linking them to appropriate resources. This is the period during which patients are at highest risk for suicide, and this period of time can be quite long in multiple myeloma (Lamers et al., Reference Lamers, Hartmann and Goldschmidt2013). In a recent study, approximately half of multiple myeloma patients surveyed using a checklist of psychosocial treatment options at this time desired some type of psychosocial support (Lamers et al., Reference Lamers, Hartmann and Goldschmidt2013). The investigators suggested that psychosocial support should be offered to patients at earlier points along the disease continuum, as another study suggested a lower need for psychosocial support at later stages of disease, although the studies were conducted differently (Molassiotis et al., Reference Molassiotis, Wilson and Blair2011a ). Furthermore, patients may independently seek information that can cause psychosocial distress (Potrata et al., Reference Potrata, Cavet and Blair2011).
At First Treatment
Treatment initiation brings with it a new set of potential psychosocial concerns. The onset of treatment is often correlated with a progression of disease, which can be associated with increased anxiety. As patients begin treatment, they must determine how to fit it into their daily lives (Molassiotis et al., Reference Molassiotis, Wilson and Blair2011b ). The cost of treatment can lead to financial difficulties, problems in terms of compliance with the therapy, or even decisions on whether to pursue treatments at all based on financial considerations (Zafar & Abernethy, Reference Zafar and Abernethy2013). Adverse events associated with treatments can dramatically impact patients' daily lives and relationships, from sexual dysfunction to debilitating fatigue (Molassiotis et al., Reference Molassiotis, Wilson and Blair2011b ; Bilotti et al., Reference Bilotti, Faiman and Richards2011).
After First Treatment
When patients first respond to treatment, they will face a new set of challenges. Participation in therapy is important to avoid disease progression but can be significantly impacted by emotional distresses, including depression (Lamers et al., Reference Lamers, Hartmann and Goldschmidt2013). Concluding a treatment can begin a long period of continuous worry that their disease will recur at any moment. Patients will need to identify this new “normal” (Molassiotis et al., Reference Molassiotis, Wilson and Blair2011b ).
First Relapse
At first relapse, patients will likely begin considering continuous therapy. Financial stresses accumulate from additional treatment or disease-associated costs (Zafar & Abernethy, Reference Zafar and Abernethy2013), resulting in negative impacts on both the patients' emotional well-being and their relationships (Lamers et al., Reference Lamers, Hartmann and Goldschmidt2013). Patients live with an uncertainty about disease progression and can begin to experience increased symptoms of disease such as pain. Physical symptoms or deterioration and increased dependency can lead to decreased quality of life (Maher & de Vries, Reference Maher and de Vries2011).
Second Relapse
At this stage, patients face more limited treatment decisions. Patients at this stage are highly experienced and have likely dealt with significant adverse events over a long period of time and may begin to experience treatment fatigue. They may begin to question the quality versus quantity of life they have left. Patients also face continuously mounting medical costs, which can impact decisions to seek additional treatment (Zafar & Abernethy, Reference Zafar and Abernethy2013).
Relapse Refractory
After aggressive life-prolonging treatment options are exhausted, patients and families will need to be supported during the transition to aggressive symptom control, palliative care, and end-of-life care. Providers must engage patients in end-of-life planning. Patients are often referred to palliative care late as opposed to early, and need to begin to put their affairs in order (Irwin et al., Reference Irwin, Greer and Khatib2012). Patients and their caregivers at this stage will likely begin to plan their financial legacy and begin preparing for the final stages of the disease. Patients and caregivers may be under significant distress at this point, as they prepare for the patient's death and transition to a new care team (if palliative care was not introduced early after diagnosis).
Global Interventions Versus Event-Specific Interventions
Although specific points and psychosocial concerns are outlined in the above sections, many interventions can be applied globally or across the disease continuum at each point of potential psychosocial concern. Education is critical at each transition point to alleviate fear of the unknown and help patients and their caregivers to better understand expectations for the future (Molassiotis et al., Reference Molassiotis, Wilson and Blair2011b ). Additional global broadly applicable interventions include cognitive-behavioral interventions, disease-management groups, problem solving, and short-term psychotherapy. Patients should be given opportunities to have many goals-of-care discussions, and early palliative care referrals for aggressive symptom control can be very helpful in reducing depression symptoms, improving quality of life, and increasing length of survival (Temel et al., Reference Temel, Greer and Muzikansky2010).
Across the transition points outlined in Figure 1, caregivers should be screened for distress, as this can negatively impact the patient if not addressed and treated. Oncology social workers or other specifically trained mental health professionals can provide vital services throughout the course of the disease. In addition, mobilization of local, regional, and national community supportive resources can also be beneficial to the patient and family experience, especially in oncology practices and cancer centers with limited psychosocial personnel and programming.
Interventions to address specific events should be considered for patients with psychosocial distress at certain transition points. For example, finances can be a concern if a patient is identified as the breadwinner for a family and needs to undergo allogeneic stem cell transplantation. Training on discussing time off with their employer and financial planning can help to alleviate some of that distress (Zafar & Abernethy, Reference Zafar and Abernethy2013). In another example, patients may continue pursuing treatment even when their quality of life begins deteriorating. If the conversation about quality versus quantity of life remaining has not been engaged in earlier, it will be important to address this topic at this stage. Skilled psychosocial professionals, such as oncology social workers, are critical to provision of the supports outlined above.
Evaluating the Impact of Interventions
Of critical importance to incorporation of psychosocial care into standard practice is assessment of interventions on the clinical progression of a patient's disease. The impact of psychosocial interventions has been well documented in the literature (Meyer & Mark, Reference Meyer and Mark1995; Cwikel et al., Reference Cwikel, Behar and Rabson-Hare2000; Graves, Reference Graves2003; Gottlieb & Wachala, Reference Gottlieb and Wachala2007; Jacobsen, Reference Jacobsen2008; Faller et al., Reference Faller, Schuler and Richard2013). Whether assessing survival or quality-of-life measures, a better understanding of the impact of psychosocial interventions will provide further support in generating a standard survivorship care plan that best addresses patient needs along the disease continuum of multiple myeloma. Barbara Anderson and her colleagues have suggested that psychosocial intervention can benefit overall survival in patients with breast cancer (Anderson et al., Reference Anderson, Yang and Farrar2008; Reference Anderson, Thornton and Shapiro2010). This finding provided the first indication that psychosocial care can impact survival, and should be used as a model to further examine the clinical impact of psychosocial care. In fact, reports have suggested that psychosocial QoL at baseline can predict overall survival in multiple myeloma as well (Strasser-Weippl & Ludwig, Reference Strasser-Weippl and Ludwig2008). By garnering more data on clinical impact, stakeholders involved in incorporating psychosocial care into the standard of care will be more able to assess the value that it provides.
Opportunities to Screen Caregivers/Family for Distress
Throughout the course of this paper, reference has been made to the critical role that family caregivers provide during various phases of treatment for multiple myeloma. Often, healthcare professionals consider families as though each were identical to the next. Family seems to be a universal concept; however, the variation in day-to-day family functioning is significant. Family researchers have investigated this variation, and numerous models have been developed to explain significant differences in family functioning. Olsen and colleagues (Zabora et al., Reference Zabora, Smith and Baker1992) described the circumplex model of family functioning, which is based on three critical components: roles and responsibilities, family cohesion, and family lifecycle. These components are based on a significant review of the family literature. About 15 to 20% of all families are more extreme in their level of cohesion; most often, these families are considered either “enmeshed” or “disengaged,” and each type can present major challenges to the healthcare team (Zabora & Smith, Reference Zabora and Smith1991). When the issue of the patient's distress was discussed earlier, the concept of distress screening was explored as a mechanism to identify those patients who are undergoing the greatest psychological distress as treatment commences. Difficulties that are experienced by patients or families are often not exhibited or identified until a later point in time. The first step in screening caregivers may be as simple as assessing family functioning and understanding the potential psychosocial challenges that may impact caregivers or patients based on the family dynamic. Along the patient's journey, as they experience additional transition points in care, caregivers and family may be screened for potential impact on levels of distress as well. “Screening” of families could occur employing Olsen's Family Adaptability Cohesion Evaluation Scale–III, which would inform the healthcare team as to the type of family they have engaged. This knowledge could benefit the patient by guiding early interventions with potentially difficult families.
Addressing Current Challenges to Linking Psychosocial Care and Clinical Disease
Based on the above outlined challenges of a diagnosis of multiple myeloma, we propose that the following principles (outlined in Table 1) be followed:
-
A. All multiple myeloma patients should be screened for distress at the time of the initial diagnosis using a consistent, highly reliable, validated tool such as the Brief Symptom Inventory-18 (BSI-18) or the Patient Health Questionnaire (PHQ-9).
-
B. Screening for distress should be repeated at critical transition points that include completion of initial outpatient treatment, completion of inpatient treatment such as stem cell transplantation, and transition to home following treatment at a tertiary care facility or at the six-month mark following initial diagnosis.
-
C. Following a screen for high distress, a comprehensive psychosocial needs assessment should be conducted by a psychosocial oncology professional such as an oncology social worker, and, at a minimum, include the following key areas (National Cancer Institute, 2013) supported by the psychosocial literature:
-
■ Physiological
-
■ Demographics of patient and caregivers
-
■ Psychological
-
■ Spiritual
-
■ Social
-
■ Legal and advance directives
-
-
D. Psychosocial interventions to meet elevated levels of distress within the individual patient or family are not limitless. Four major interventions have been identified that can benefit patients and families experiencing distress; these include psycho-education, cognitive-behavioral therapy, disease-management groups, and short-term psychotherapy (Fawzy et al., Reference Fawzy, Fawzy and Arndt1995). Problem-solving education is a combination of psycho-education and cognitive-behavioral techniques (Houts et al., Reference Houts, Nezu and Nezu1996; Toseland et al., Reference Toseland, Smith, McCallion and Smith1995b ).
-
E. Pertinent outcomes for multiple myeloma patients and their families following assessment/intervention would include whether there has been a reduction in distress, a decrease in the severity of physical symptoms, or an increase in quality of life. In addition, given the recent work of Anderson et al. (Reference Anderson, Thornton and Shapiro2010), salivary cortisol levels and other stress-related biomarkers could also be measured to determine if a significant physical risk has also been diminished. Further research is needed to examine the impact on clinical disease, but standardization of outcome measures should be strongly considered to improve our understanding of the clinical impact of psychosocial interventions.
Table 1. Principles of psychosocial care for patients with multiple myeloma

FUTURE DIRECTIONS AND CONCLUSION
Significant progress has been made in treatment of multiple myeloma, extending survival for patients. It is clear that the diagnosis and relatively long-term trajectory of multiple myeloma can have a dramatic effect on patients and their family members. It is the opinion of our group that patients cannot simply manage this illness and the associated distress without the benefit and support of family members. Each influences the other. Survivorship, or the ability to productively live well despite this diagnosis, requires that all of the elements in the previous section are defined and operationalized. Perhaps survivorship care plans can contribute to operationalizing these needs. Community resources can play a valuable role in helping patients and families address areas of distress and connect with others facing a similar journey. Many patients do not access community-based psychosocial resources because they did not know about them (“no one told me”) (Forsyth et al., Reference Forsyth, Kent and Weaver2013). Survivorship care plans, developed at the time of diagnosis and including the items discussed in the current paper, can become evolving documents that guide a patient and family through treatment, recovery, and then to living as a cancer survivor through disease progression and end of life, and can lead to identifying and addressing distress earlier on in the patient or caregiver journey.
Multiple myeloma and its treatment are associated with a unique set of challenges, as these patients tend to be older at the time of diagnosis and can experience significant levels of fatigue and pain. Treatment transitions can be rapid as the healthcare team attempts to identify the best course of treatment. Stem cell transplantation and associated recovery certainly generates significant challenges for older patients and their family caregivers. Future research should focus on the interplay between patient and family caregivers in order to identify optimal interventions for both multiple myeloma patients as well as their family caregivers. It has been hypothesized that distress screening and early interventions that reduce a patient's level of distress could reduce cortisol levels and might promote longer survival (Mundy-Bosse et al., Reference Mundy-Bosse, Thornton and Yang2011). Further efforts should be made to correlate reduction of distress with such clinical parameters as cortisol levels, time to progression, response to treatment, minimal residual disease status, cytogenetic status, M protein levels, and survival. We know that caregiver distress can affect patients, but the impact of caregiver interventions on patient disease outcomes should also be assessed in future research.
Finally, after a review of the literature, we propose a model of care that promotes active engagement in therapies for the treatment of multiple myeloma while engaging the individual patient and their family caregivers. This treatment approach must be evidence based in terms of distress screening tools, comprehensive psychosocial assessments, and, most importantly, the interventions and measurements of response that clinicians apply to this population. Furthermore, simultaneous care provided to alleviate symptoms and side effects might be incorporated earlier on in the disease continuum than palliative care is currently introduced. This may help in screening patients for distress and alleviate associated distress at future stages when additional care teams are introduced. As previously stated, multiple myeloma presents numerous complex problems for patients and their family caregivers, and the focus should be on ensuring that these patients possess the most effective resources with which to manage this difficult disease.
ACKNOWLEDGMENTS
The authors would like to gratefully acknowledge Elizabeth Bilotti for her contributions to the concepts outlined herein. Editorial assistance was provided by Mark Ellis, Ph.D. (E-Squared Communications) and funded by Onyx Pharmaceuticals.




