Introduction
Different terms have been utilised to describe the spread of infection from the external ear to soft tissue and bony structures of skull base. Terms such as necrotising otitis externa were thought to accurately describe the pathological process.Reference Nadol1 If the inflammatory process in necrotising otitis externa extends to the central skull base, formed by temporal, sphenoid and occipital bones, the condition becomes a type of central skull base osteomyelitis. The other two types include central skull base osteomyelitis taking place after resolution of necrotising otitis externa and central skull base osteomyelitis as a primary condition.Reference Lesser, Derbyshire and Lewis-Jones2 Necrotising otitis externa occurs mainly in elderly, immunocompromised and diabetic patients.Reference Carfrae and Kesser3
The main symptom of necrotising otitis externa is severe deep pain which is worse at night. The main sign is granulation tissue in the ear canal and the main causative bacteria is Pseudomonas aeruginosa.Reference Carfrae and Kesser3 Diagnosis is controversial, with a recent literature review highlighting variability in diagnostic criteria between studies.Reference Mahdyoun, Pulcini, Gahide, Raffaelli, Savoldelli and Castillo4 However, most studies appear to agree on two main findings to establish diagnosis: otitis externa that is not responding to topical treatment and P aeruginosa as the causative agent. Otalgia and computed tomography (CT) scan findings appear to be less agreed upon.Reference Mahdyoun, Pulcini, Gahide, Raffaelli, Savoldelli and Castillo4 Management is mostly medical with dual antibiotic therapy recommended;Reference Carlton, Perez and Smouha5 most authors recommend treatment for six weeks.Reference Mahdyoun, Pulcini, Gahide, Raffaelli, Savoldelli and Castillo4
Unlike many other otological conditions, most patients with necrotising otitis externa are admitted to hospital in order to establish diagnosis and start treatment. Patients are then discharged back to the community, if capacity allows, to finish their treatments. Treatment in community requires that patients are fitted with a peripherally inserted venous catheter such as a long line or midline catheter.
Length of stay in hospital may be affected by local healthcare factors such as inter-disciplinary co-operation and primary and secondary care co-ordination. For example, unavailability of primary care provision of intravenous antibiotics may lead to prolonged admission. Increased length of stay has been shown to correlate with a higher rate of complications.Reference Schimmel6 It also has financial consequences with an average cost for patients aged 65 years and over estimated at £303 for each additional day in hospital.Reference Amyas7
In this study, we aimed to report the outcomes of a closed cycle audit of length of stay of patients with necrotising otitis externa compared with the national average and to present a new necrotising otitis externa management protocol.
Materials and methods
Ethical considerations
This project was registered as an audit and a quality improvement project with the hospital audit office.
Methods
Hospital Episode Statistics data,8 published by NHS England, were reviewed to extract national figures regarding length of stay in hospital for patients admitted with necrotising otitis externa.
Electronic medical records of patients admitted with necrotising otitis externa to the Freeman hospital (a tertiary referral centre) between 1 January 2015 and 31 August 2018 were reviewed and analysed for patient age, sex, length of admission and time taken for key management steps. Following the first cycle of the audit, a new protocol was devised and implemented.
The second cycle audit was performed six months later, and the same data items were collected. Following the second cycle, the protocol was revised. The main outcome measure was length of in-patient stay.
Statistical analysis was performed using Prism 8® statistical software.
Results
Hospital Episode Statistics data
The number of patients admitted to hospital in England with necrotising otitis externa increased from 107 in 2002–2003 to 1126 in 2017–2018, with a total of 12 303 hospital bed days (mean of 10.9 days per patient) compared with 1130 bed days in 2002–3 (mean of 10.6 days per patient).8
First cycle audit
A total of 66 hospital admissions occurred over the study period in our trust for 48 patients in total with a mean length of stay of 12.4 days. Twelve patients (25 per cent) had more than one admission (Figure 1). Fourteen of the 18 re-admissions were for peripherally inserted venous catheter-related problems. The remaining four re-admissions (in three patients) were for persistence of symptoms. Age ranged from 45 to 95 years old with a mean age of 76 years. Data regarding gender, side of necrotising otitis externa and presence of diabetes are summarised in Table 1. Necrotising otitis externa was bilateral in one patient, spreading from the left ear to the right side via the skull base. Source of admission is highlighted in Figure 2 with the majority of admissions taking place from routine consultant clinic.

Fig. 1. Details of patients who had more than one admission.

Fig. 2. Source of admission in first cycle cohort. CAS = casualty clinic; GP = general practitioner; A&E = accident and emergency; Cons: consultant; EUA = examination under anaesthesia
Table 1. Demographic data of first cycle cohort

NOE = necrotising otitis externa
Sixteen patients had cranial nerve palsies. Of these, 14 patients had isolated facial nerve palsy, one patient suffered both hypoglossal and vagal nerve palsies, and one patient had isolated vagal nerve palsy and died of aspiration pneumonia as a result. Three more patients died in close proximity to their diagnosis of necrotising otitis externa with no identifiable cause.
Following the first cycle, discussions with all teams involved in caring for necrotising otitis externa patients, including radiology, microbiology, interventional radiology, out-patient parenteral antimicrobial therapy teams and district nurses led to development of a new protocol (Figure 3).
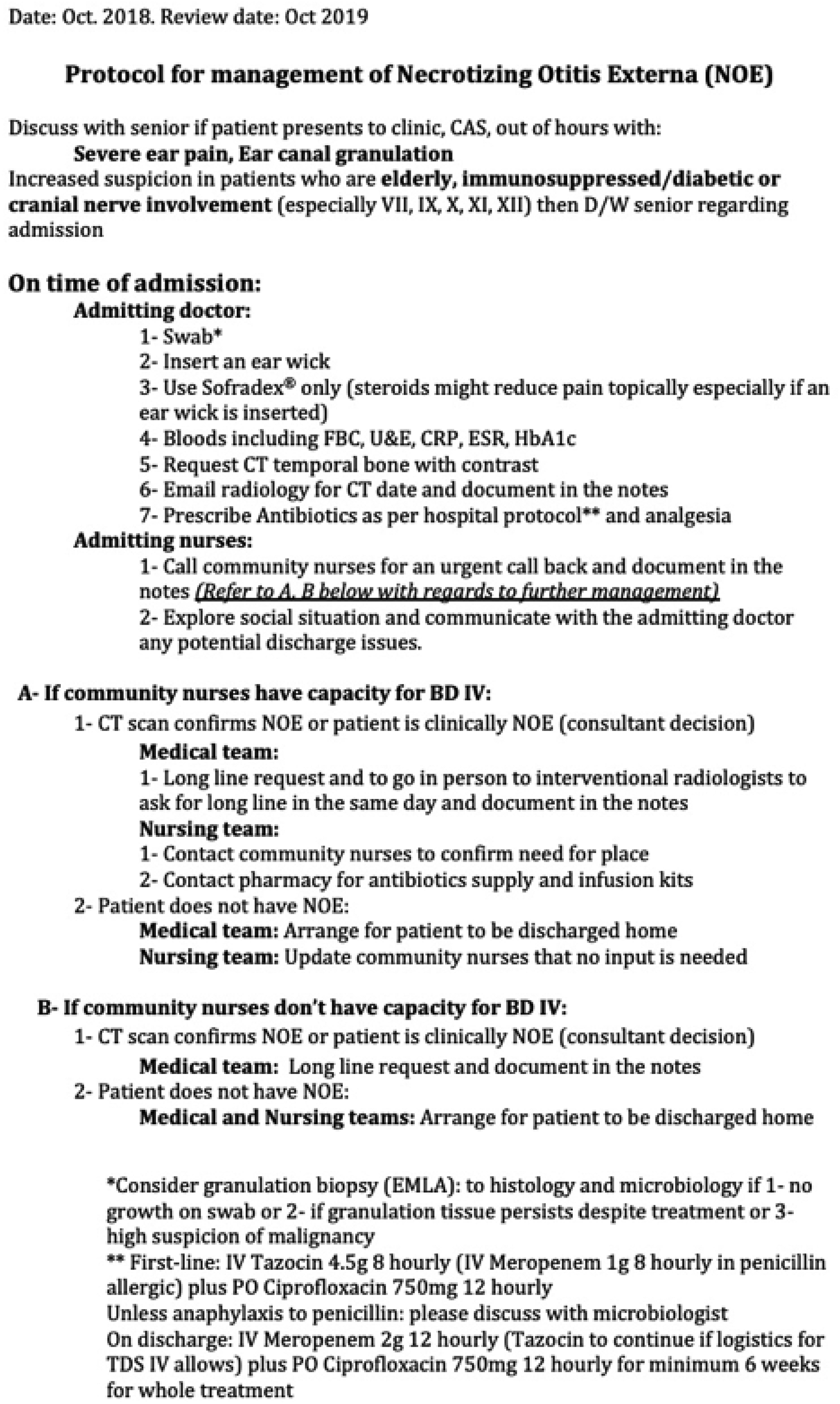
Fig. 3. Necrotising otitis externa (NOE) management protocol used in the second cycle. CAS = casualty clinic; D/W = discussed with; FBC = full blood count; U&E = urea and electrolyte; CRP = C-reactive protein; ESR = erythrocytes sedimentation rate; HbA1c = haemoglobin A1c; CT = computed tomography; BD = twice a day; IV = intravenous; EMLA = eutectic mixture of local anaesthetics; PO = oral; TDS = three times a day
Second cycle audit
Six months later a second audit was conducted. A total of 11 hospital admissions for 9 patients were included with a mean length of stay of 7.1 days. Table 2 summarises the time taken for key interventions for first and second cycle (dates for CT and peripherally inserted venous catheter requests were unavailable for two patients). Discussions following the second cycle led to modification of the protocol (Figure 4).

Fig. 4. Necrotising otitis externa (NOE) management protocol current version. CAS = casualty clinic; D/W = discussed with; FBC = full blood count; U&E = urea and electrolyte; CRP = C-reactive protein; ESR = erythrocytes sedimentation rate; HbA1c = haemoglobin A1c; CT = computed tomography; ID = infectious diseases; RVI = Royal Victoria Infirmary; f/u = follow up; IV = intravenous; PO = oral; TDS = three times a day
Table 2. Details of time taken for main interventions in both cycles

*n = 24: these are the number of admissions in which patients underwent all requests and procedures as in-patients; †n = 7: full data available for only 7 patients. CT = computed tomography
Statistical analysis
A two-tailed Mann–Whitney U Test was used to compare the difference in length of stay before and after intervention in patients in whom radiological investigations and peripherally inserted venous catheter insertions were both requested and performed during admission. There was a statistically significant (p = 0.02) decrease in length of stay in the second cycle of the audit compared with the first.
Discussion
The number of patients admitted with necrotising otitis externa in England is increasing at a concerning rate. However, length of stay in hospitals appears to be relatively stable over the last 15 years.8 The average length of stay of necrotising otitis externa patients in our hospital before intervention was longer than the national average in England according to Hospital Episode Statistics data.8 Shorter stay in hospital reduces unnecessary complications, is more cost-effective and aligns with the NHS Long Term Plan9 goals of minimising unnecessary and prolonged admissions.
In accordance with the literature, necrotising otitis externa mainly presented in male patients in our study. Prevalence of facial nerve palsy was also in line with the literature. However, diabetes was not as common in our cohort compared with other studies.Reference Mahdyoun, Pulcini, Gahide, Raffaelli, Savoldelli and Castillo4 In this study, CT scan with contrast was utilised as the main radiological diagnostic modality because of availability and its use in previous studies as the chosen imaging modality.Reference Mahdyoun, Pulcini, Gahide, Raffaelli, Savoldelli and Castillo4 However, it is important to point out that CT and magnetic resonance imaging (MRI) complement each other.Reference Kroonenburgh, Meer, Bothof, Tilburg, Tongeren and Postma10 In situations where clinical suspicion is high but intravenous (IV) treatment is cumbersome for the patient and CT is not conclusive, it might be advisable to organise an MRI scan to be performed as well in order to help confirm diagnosis of necrotising otitis externa before committing to the treatment course.
With regards to length of admission, careful analysis of the first cycle data in our study helped with identifying the causes of delays in discharge, which were similar to causes highlighted nationally by NHS England in 2017: namely, awaiting completion of assessment and awaiting further care outside of the hospital.Reference Fernandez, McGuire and Raikou11 In our cohort, the main critical steps necessary in order to achieve earlier discharge were CT scan, peripherally inserted venous catheter insertion and arrangements for administration of IV antibiotics in the community.
The first version of our protocol (Figure 3) was designed to save time at each of these steps. Successful implementation of our protocol would have been impossible without trans-specialty co-operation of all stakeholders. Implementation of our protocol helped identify other areas for improvement. For example, in the first cycle, ensuring prompt peripherally inserted venous catheter insertion once diagnosis was confirmed was challenging because of lack of funding for the service in our hospital. At the time, this was overcome by highlighting the significance of peripherally inserted venous catheter fitting in facilitating discharge and by the interventional anaesthetic team dedicating protected time, resources and personnel. Consequently, our first cycle results supported the establishment of a regular service for peripherally inserted venous catheter provision that was piloted in our hospital.
The overall results of our second cycle were promising in terms of timely management and discharge of patients with a shorter length of stay compared with the national average. Additionally, the second version of our protocol acknowledged the interest of our hospital's infectious diseases department who were keen to offer their expertise in managing patients resistant to treatment and to supervise out-patient administration of antibiotics.
Finally, it is worth noting that our protocol might not be generalisable because of local differences in provision of services. Standardising in-patient necrotising otitis externa management across NHS hospitals in England is desirable, and building a national network would allow for stronger conclusions and recommendations to be reached regarding necrotising otitis externa diagnosis and management.
Limitations
The diagnostic criteria of necrotising otitis externa are still a point of debate. In our study, diagnosis was clinical with radiological confirmation. Positive radiological findings in our study were either the presence of bony erosion or the presence of soft tissue enhancement in the skull base region.
Another limitation was the small numbers in the post-protocol cohort. However, necrotising otitis externa is not common, and the patients included were sufficient to show that statistically significant reduction in length of stay took place.
Conclusion
Patients with necrotising otitis externa require prompt diagnosis and management in order to shorten length of stay in hospital and avoid serious complications. However, prompt management can be hindered by contextual factors that differ from one hospital to another. Multi-disciplinary protocol development and implementation could help in reducing length of stay of necrotising otitis externa patients.
Competing interests
None declared








