Summations
∙ Among patients with schizophrenia, prevalence of obsessive–compulsive symptom (OCS)/obsessive–compulsive disorder (OCD) is about 14% and 26% respectively.
∙ OCS/OCD is seen in all the phases, that is, At risk mental state (ARMS), acute phase, chronic/residual phase of Schizophrenia.
∙ Presence of OCS/OCD is schizophrenia is associated with poor outcome.
Considerations
∙ There is limited data on the efficacy/effectiveness of various pharmacological measures for management of OCS/OCD in patients with schizophrenia.
∙ There are no clear cut guidelines for management of OCS/OCD in patients with schizophrenia.
Introduction
Psychiatric comorbidities in patients with schizophrenia had been well recognised and presence of co-morbidity often poses several clinical problems in the diagnosis and management of schizophrenia. Several studies have shown that compared to general population, patients with schizophrenia have an increased prevalence of anxiety disorders (approximately 4.3–15.4% of panic disorder,4–20.8% of post-traumatic stress disorder, 8.1–21.8% of social phobia, 12–37.5% have OCD) (Reference Achim, Maziade, Raymond, Olivier, Mérette and Roy1,Reference Rapp, White-Ajmani, Antonius, Goetz, Harkavy-Friedman, Savitz, Malaspina and Kahn2), depression (13–25%) (Reference Baynes, Mulholland, Cooper, Montgomery, MacFlynn, Lynch, Kelly and King3) and substance use disorders (45–50%) (Reference Buckley, Miller, Lehrer and Castle4). Of the various psychiatric co-morbidities, OCS/OCD has received special attention since the very beginning of the concept of co-morbidity in schizophrenia. The exact prevalence of OCS/OCD in patients with schizophrenia is unknown, however, studies which have tried to evaluate the prevalence of OCS/OCD in first episode schizophrenia and chronic schizophrenia have reported rate of OC phenomena to be as high as 3–59% but on an average the clinical studies which have used proper diagnostic interview [Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV; Structured Clinical Interview for DSM-IV Axis I Disorders (SCID)] and Yale–Brown Obsessive–Compulsive Symptom checklist (YBOCS) have estimated the prevalence to range between 14% and 26% (Reference Poyurovsky, Kriss, Weisman, Faragian, Kurs, Schneidman, Fuchs, Weizman and Weizman5–Reference Bottas, Cooke and Richter10). In addition, persons with schizotypal personality disorder (SPD) have also been found to have a high prevalence (as high as 50%) of OCS/OCD (Reference Poyurovsky and Koran7,Reference Poyurovsky, Faragian, Pashinian, Heidrach, Fuchs, Weizman and Koran8,Reference Baer, Jenike, Ricciardi, Holland, Seymour, Minichiello and Buttolph11,Reference Matsunaga, Kiriike, Matsui, Oya, Iwasaki, Koshimune, Miyata and Stein12). However, despite the high prevalence of OCS in patients with schizophrenia, these symptoms are not considered to be primary symptoms of schizophrenia and patients with schizophrenia are not routinely screened for OCS. Due to this, in general OCS/OCD has not received as much attention as other symptoms of schizophrenia. But, over the last two decades, there has been resurgence in the interest related to these, yet there are no guidelines/treatment protocols for the assessment and management of these symptoms when seen in patients with schizophrenia.
This narrative review attempts to evaluate the evolution of the concept, epidemiology, association of OCS/OCD with other symptoms of schizophrenia, possible explanations for this comorbidity, impact of OCS/OCD on neurocognition and impact of OCS/OCD on course and outcome of schizophrenia. In addition an attempt is made to evaluate the current nosological status and provide an outline as to how to assess and manage OCS/OCD in patients with schizophrenia.
Historical concepts
In general, psychotic and neurotic disorders were considered as distinct from each other and historically OCS/OCD has been understood as a neurotic disorder. Emil Kraepelin did not consider OCS as a psychopathological component of schizophrenia, but he suggested that the evidence of transition from obsessions to paranoia is lacking (Reference Decker13). In contrast to this, Bleuler suggested that OCS may be part of At Risk Mental States (ARMS) of schizophrenia and regarded these symptoms as automatisms in patients with schizophrenia which are comparable to auditory and visual hallucinations, and can be considered as hallucinations of thinking, striving and wanting (Reference Steinberg, Carius, Fontenelle, Steinberg, Carius and Fontenelle14). in addition, he also regarded OCS in patients with schizophrenia as a neurotic condition, independent of symptoms of schizophrenia (Reference Bleuler15).
Subsequently, many authors, especially Stengel (Reference Stengel16) postulated that obsessions and delusions lie in a continuum. Stengel for the first time systematically studied OCS in patients with schizophrenia. Based on the information from amnestic recall, direct interview and follow-up of patients, he concluded that OCS precede the onset of psychosis and do not follow psychosis, usually disappear during the psychotic episodes and re-emerge during remission, usually preserve their characteristic features and do not transform to delusions. In addition, he concluded that presence of obsessions lead to difficulty in interpreting delusions and hallucinations, suggesting that obsessions modify the psychotic symptoms (Reference Stengel16). It was also observed that patients with OCS have a positive family history, suggesting hereditary and constitutional predisposition for both schizophrenia and OCS. Further, he observed that OCS were not seen in any of the cases of catatonic or hebephrenic schizophrenia, indicating a protective role of OCS against these subtypes of schizophrenia. In terms of clinical course, it was concluded that subjects with co-morbid OCS usually have a benign course, with marked tendency for remission. Hoch and Polatin (Reference Hoch and Polatin17) described patients with schizophrenia with OCS as having pseudo-neurotic schizophrenia, characterised by pan-anxiety, pan-neurosis and pan-sexuality. Follow-up studies after 5–20 years of these patients showed that about 20% patients initially diagnosed with pseudo-neurotic schizophrenia later develop typical paranoid, catatonic and hebephrenic symptoms of schizophrenia and almost 40% of patients with pseudo-neurotic schizophrenia needed frequent hospitalisations (Reference Hoch, Cattell, Strahl and Pennes18).
After these initial evaluations, there was a decrease in interest in this area till 1980, although many small sample size, cross-sectional studies continued to note the presence of OCS/OCD among patients with schizophrenia. These studies also reported OCS not only in the prodromal phase (Reference Niendam, Berzak, Cannon and Bearden19), but also in other phases of schizophrenia (Reference Poyurovsky, Hramenkov, Isakov, Rauchverger, Modai, Schneidman, Fuchs and Weizman6,Reference Eisen, Beer, Pato, Venditto and Rasmussen20–Reference Tibbo, Kroetsch, Chue and Warneke22). However, the revisions in the nosological systems (DSM and International Classification of Diseases – ICD) during this time period did not consider OCS as main symptoms of schizophrenia. Although pseudo-neurotic/latent subtype was retained till DSM-II, but in DSM-III, pseudo-neurotic subtype was collapsed and it was considered that OCD cannot be diagnosed in presence of schizophrenia.
However, the interest in OCS/OCD in schizophrenia was renewed by Fenton and McGlashan (Reference Fenton and McGlashan23) by the famous Chestnut Lodge follow-up study, which found that about 13% of patients with schizophrenia have OCS, which is significantly higher than that seen in general population. This study also showed that OCS precede the onset of psychotic symptoms and compared to those without OCS, those with OCS have worse outcome in multiple domains (longer hospitalisation, poor employment rates and poor functioning) (Reference Fenton and McGlashan23). This led to further studies in this area and findings of these studies resulted in clubbing of pseudo-neurotic schizophrenia under schizotypal disorder in ICD-10 and DSM-IV, which allowed consideration of a comorbid diagnosis of OCD in patients with schizophrenia (Reference de Haan, Schirmbeck and Zink24). In addition, this development coincided with the introduction of atypical antipsychotics in early 1990s and reports of new onset OCS/OCD after starting atypical antipsychotic emerged, which showed that rates of OCS/OCD were much higher among those receiving atypical antipsychotics (Reference Bottas, Cooke and Richter10). With the emergence of more and more data the association of OCS/OCD was postulated to have one of the five possible sequences, that is, presence of OCS/OCD before the onset of psychosis as independent diagnosis, presence of OCS/OCD prior to psychotic manifestation as part of the ARMS, simultaneous occurrence of OCS/OCD and psychotic symptoms as first manifestation of psychosis, emergence of OCS/OCD as aftermath of an acute episode during the course of chronic schizophrenia and as de novo OCS/OCD after initiation of antipsychotic treatment (Reference Schirmbeck and Zink25).
Epidemiology of OCS/OCD in Schizophrenia
A number of studies have evaluated the prevalence of OCS/OCD among patients with schizophrenia. Most of these studies are cross-sectional in nature, with sample size varying from 37–400 participants, have included patients of different age groups (adult, adolescents, elderly) recruited from either inpatients/outpatient population. These studies have relied up on Mini International Neuropsychiatric Interview, SCID and DSM-IV criteria for diagnosis OCD and YBOCS for assessment of severity of OCS/OCD. These studies suggest that the prevalence of OCS and OCD is much higher among patients of schizophrenia, when compared to general population, with prevalence range of OCS to be 2.5–64%, whereas prevalence rates for OCD ranging from 0% to 37.5% (Reference de Haan, Schirmbeck and Zink24,Reference Schirmbeck and Zink25). These studies have come from different countries suggesting that these symptoms are seen all over the World, indicating universal occurrence of phenomenon with greater rates of OCS/OCD. Further, the data suggests that prevalence of OCS/OCD is higher among outpatients, when compared to inpatients. The higher prevalence in outpatients suggests that OCS is more easily detectable after remission of psychosis. Further data also suggests higher rates of OCS/OCD among patients with multiple episodes compared to that in those with first episode psychosis (FEP) (Reference de Haan, Schirmbeck and Zink24). Few studies have evaluated incidence of OCS/OCD and the incidence at 24 months in patients with FEP were noted to range from 3.5% to 4.3% for OCS and between 0% and 1.8% for OCD (Reference de Haan, Sterk and Van der Valk26,Reference de Haan, Sterk, Wouters and Linszen27).Very few studies have evaluated the prevalence among patients with different phases of illness. According to a study by Schirmbeck and Zink (Reference Schirmbeck and Zink25), the prevalence of OCS and OCD in ARMS, FEP and overall patients of schizophrenia were 12.1% and 5.2%, 17.1% and 7.3%, 25% and 12.1%, respectively, with comparable prevalence rates among adolescents, adults and elderly (Reference Schirmbeck and Zink25). A meta-analysis of 43 studies with 3978 subjects exploring prevalence rates of OCS in schizophrenia reported the mean prevalence of OCD and OCS to be 12.3% and 30.7%, respectively, with prevalence influenced by the method of assessment and higher prevalence in chronic patients (Reference Swets, Dekker, Van Emmerik-van Oortmerssen, Smid, Smit, de Haan and Schoevers28).
Explanations for the comorbidity: OCS/OCD and schizophrenia
Four possible explanations for comorbid OCS/OCD among patients with schizophrenia had been put forward, that is, one disorder is a risk factor for another, presence of some common risk factors for both mental disorders, OCS/OCD being an integral part of the psychotic syndrome and lastly obsessive pathology may be an outcome of administration of neuroleptics (Reference de Haan, Schirmbeck and Zink24,Reference Frías-Ibáñez, Palma-Sevillano and Farriols-Hernando29,Reference Scotti-Muzzi and Saide30) (Table 1).
Table 1 Explanations for the comorbidity of obsessive–compulsive symptom/ obsessive–compulsive disorder (OCS/OCD) with schizophrenia

Phenomenology of OCS/OCD among patients with schizophrenia
Aggressive and contamination obsessions are the most prevalent (but sexual and somatic obsessions have also been documented) types of obsessions and the most prevalent compulsions are those of washing and checking (but repeating and hoarding compulsions have also been reported) (Reference de Haan, Schirmbeck and Zink24,Reference Oulis, Konstantakopoulos, Lykouras and Michalopoulou47,Reference Tonna, Ottoni, Paglia, Monici, Ossola, DE Panfilis and Marchesi48).The mean YBOCS total scores of schizo-obsessive patients have been shown to range from 15 to 28, indicating moderate to severe OCS/OCD. The characteristics of OCS in schizo-obsessive patients are similar to those presented in OCD patients, including the factor structure (Reference Boyette, Swets, Meijer and Wouters49–Reference Seedat, Roos, Pretorius, Karayiorgou and Nel51).
However, it is important to distinguish OCS/OCD in schizophrenia from presence of features of schizotypal personality disorder in patients with OCD. Features of schizotypal personality disorder in patients with OCD have been well studied both in non-clinical samples (Reference Roth and Baribeau52) and in OCD subjects (Reference Poyurovsky, Faragian, Pashinian, Heidrach, Fuchs, Weizman and Koran8). Despite several methodological issues, it has been consistently reported that OCD patients with SPD have a deteriorative course with poor insight and poor prognosis (Reference Baer, Jenike, Ricciardi, Holland, Seymour, Minichiello and Buttolph11,Reference Eisen and Rasmussen53). Certain clinical parameters like male gender, early age of onset of OC symptoms, counting compulsions and history of specific phobia in patients with OCD increases the likelihood of schizotypy (Reference Poyurovsky and Koran7). Further those with comorbid SPD perform poorly on neurocognitive tests as compared with pure OCD (Reference Harris and Dinn54). In addition, treatment response to standard pharmacological agents [selective serotonin reuptake inhibitors (SSRIs)] and behaviour therapy is usually poor in patients with OCD and SPD (Reference Jenike, Baer, Minichiello, Schwartz and Carey55,Reference Mundo, Erzegovesi and Bellodi56). Addition of low-dose antipsychotics to SSRIs has proven to benefit these patients (Reference McDougle, Goodman, Price, Delgado, Krystal, Charney and Heninger57,Reference Bogetto, Bellino, Vaschetto and Ziero58). Therefore, the entity of Schizotypic OCD or OCD with SPD is different from schizophrenia with OCD and pure OCD.
Association of OCS/OCD with other symptom dimensions of Schizophrenia
Meta-analysis of studies published between 1950 and 2006 suggest that presence of OCS is associated with significantly higher severity of global and negative psychotic symptoms (Reference Cunill, Castells and Simeon59). Studies also suggest that compared to patients of schizophrenia without OCS/OCD, patients of schizophrenia with comorbid OCS/OCD have higher severity of bizarre behaviour, lower severity of delusions, hallucinations, formal thought disorder and have lower anergia. In addition, studies have also found that the severity of OCS correlates significantly with the negative and general psychopathology subscale scores of the Positive and Negative Syndrome Scale (PANSS), as well as with depressive symptoms (Reference Schirmbeck and Zink25).
Based on the inter-relationship between OCS and psychotic symptoms, some authors have tried to classify these patients into two groups, that is, (1) patients with classical ego-dystonic obsessions and/or compulsions that were unrelated to the content of psychotic symptoms; and (2) patients with obsessions and/or compulsions related to delusional and/or hallucinatory content (Reference Poyurovsky, Weizman and Weizman60).
With regard to the specific relationships between psychotic and OCS dimensions among patients with schizophrenia, studies which have evaluated the dimensional scores of both schizophrenia and OCS have found that the symptoms of schizophrenia collapse into four dimensions (disorganisation, bizarre delusions, auditory hallucinations and diminished expression) and OCS also have four dimensions (obsessions, compulsions, somatic obsessions and hoarding/collecting compulsions) (Reference Cunill and Castells61,Reference Ritsner62). Further, bizarre delusions and obsessions have been found to have positive correlation, supporting the view that these reflect a manifestation of the same mechanism, that is, over-valued ideas lying on a continuum of obsessional doubts to delusional certainty and hallucinations have been found to be positively correlated with compulsions, also suggesting a common underlying mechanism that may be related to a decreased capacity to inhibit behaviours or thoughts (Reference Kozak and Foa63).
Impact of OCS/OCD on neurocognitive functions
Initial studies which evaluated the neurocognitive functioning reported that patients with schizophrenia with OCS performed worse than patients with schizophrenia without OCS on a number of domains such as visual memory, cognitive and motor shifting abilities and visual-spatial skills (Reference Berman, Merson, Viegner, Losonczy, Pappas and Green64). However, subsequent studies have shown inconsistent findings with respect to memory and attention, with few showing greater impairments in verbal memory, spatial memory and attention in patients with schizophrenia with OCS/OCD when compared to those with schizophrenia without comorbid OCS/OCD (Reference Ongür and Goff65–Reference Whitney, Fastenau, Evans and Lysaker67).Studies have even reported that presence of poorer executive functions predicted higher levels of OCS both concurrently and prospectively (Reference Tumkaya, Karadag, Oguzhanoglu, Tekkanat, Varma, Ozdel and Ateşçi66–Reference Schirmbeck, Rausch, Englisch, Eifler, Esslinger, Meyer-Lindenberg and Zink69). Overall, the evidence suggests that compared to patients of schizophrenia without comorbid OCS/OCD, those with comorbid OCS/OCD have greater cognitive impairment when compared to patients with OCD.
Course of OCS/OCD in schizophrenia
Very few longitudinal studies have examined the course of OCS/OCD among patients with schizophrenia. Some of the studies suggest that among patients with pre-existing OCS/OCD, symptoms usually persist or worsen independent of the course of schizophrenia, whereas, other studies suggest that a small proportion (13.4%) of patients with comorbid OCS/ OCD have persistent symptoms (Reference de Haan, Sterk, Wouters and Linszen27). Further, studies have also revealed that compared to patients with schizophrenia those with OCS/OCD have higher psychosocial dysfunction, poorer social and vocational functioning, poorer general quality of life, higher level of hopelessness, more frequently use avoidant focussed coping strategies and higher rates of suicidal ideations and attempts (Reference Cunill, Castells and Simeon59,Reference Cunill and Castells61).
Nosological issues
In view of high comorbidity, some of the authors have proposed the term ‘schizo-obsessive’ and have proposed this to be considered as a subtype of schizophrenia. Studies using a categorical definition consider a patient to be having schizo-obsessive disorder/subtype, if in addition to a diagnosis of schizophrenia; the patient meets the full diagnostic criteria for OCD or symptomatic criteria for OCS as per DSM nosological system (70).
Status in DSM-5 and ICD 11
DSM-5, has not accepted the concept of ‘Schizo-obsessive’ or ‘Schizo-OCD’ disorder in Psychotic disorders group or OC spectrum disorders (70). However, one can consider co-morbid diagnosis of two disorders simultaneously as per DSM-5. In contrast to DSM-5, ICD-10 does not permit a diagnosis of OCD in the presence of schizophrenia (71). Yet there have been some recommendations to improve the diagnosis of schizophrenia with OCS/OCD, that is, to replace ICD-10 guidelines for differential diagnosis with a more detailed description of disorders that share some symptoms with OCD (anxiety disorders, depressive disorders, other obsessive–compulsive and related disorders, tic disorders, eating disorders, psychotic disorders) and in order to enhance clinical utility, disorders that commonly co-occur with OCD should also be outlined in the text of ICD-11 (Reference Luciano72–74). However, as per the available ICD-11 β draft, ‘Schizo-obsessive’ disorder has not been considered yet. Pseudo-neurotic schizophrenia has been retained in inclusion list of schizotypal disorder. Insight has been added as specifier from good/fair to absent/no insight. But it is still not clear whether a patient with schizophrenia can be diagnosed with co-morbid OCD or not as per ICD-11 nosological system.
Management of OCS/OCD in schizophrenia
The management of OCS/OCD among patients with schizophrenia poses a clinical challenge and the most important step in the management is proper assessment of OCS/OCD in relation to the sequence of appearance of OCS in relation to other symptoms of schizophrenia, use of atypical antipsychotics, phase of illness and severity of OCS/OCD. For this, one need to take a proper history with special focus on the natural long term course of schizophrenia and the occurrence of OCS during the course of illness (Fig. 1). It is also important to evaluate the OCS by using one of the structured assessment instruments like YBOC checklist, Maudsley Obsessive–Compulsive Inventory and Padua inventory (Reference Schirmbeck and Zink25,Reference Zink75) and rate the severity by using YBOCS.

Fig. 1 Assessment of OCS/OCD in a patient with Schizophrenia
In addition, Obsessive–Compulsive Inventory-Revised, which is a self-rated inventory which measures six symptom dimensions of OCD (Checking, Washing, Ordering, Hoarding, Obsessing, and Neutralising) (Reference Huppert, Walther, Hajcak, Yadin, Foa, Simpson and Liebowitz76) can be used to assess OCS in patients with schizophrenia. This inventory has been used in patients with schizophrenia and has been found to be quite useful in assessing subjective suicide risk (Reference Opakunle, Aloba, Akinsulore, Opakunle and Fatoye77) and in estimating prevalence of OCS in patients with chronic schizophrenia on clozapine (Reference Fernandez-Egea, Worbe, Bernardo and Robbins78).
Many a time’s clinicians are faced with difficulty in distinguishing obsessions with poor insight from delusions, compulsions from mannerisms, and obsessional slowness from thought blocking. Although no universally accepted method is available for identifying OCS in patients with schizophrenia, yet some recommendations have been suggested in order to facilitate this task. It has been proposed that a recurrent, intrusive, ego-dystonic thought should not be considered an obsession if these revolves exclusively around delusional themes (e.g. violent images in response to delusion of persecution) and repetitive acts should only be considered a compulsion if these occurs only in response to an obsession, not if these occurs in response to a delusion (e.g. repetitive checking in response to paranoid fears does not constitute a compulsion) (Reference Oulis, Konstantakopoulos, Lykouras and Michalopoulou47,Reference Kozak and Foa63). In addition, at times it is difficult to identify OCS in the presence of formal though disorder as these patients are unable to articulate their obsessions and do not exhibit compulsions and hence, it might not be possible to determine if apparent OCS in the presence of psychosis represent real OCS. Thus, it is necessary to reassess for OCS once formal thought disorder and psychotic symptoms have resolved or are controlled. It is also important to note that at times, primary obsessive slowness can be mistaken as a psychotic symptom. Hence, assessment need to be considered as an ongoing process and if the OCS cannot be ascertained in the initial evaluation, than the patients should be re-evaluated for the same after remission of positive symptoms (Fig. 1).
The various treatment options which have been used to manage OCS/OCD in patients of schizophrenia include anti-psychotics, antidepressants, mood-stabilisers and somatic modalities like electroconvulsive therapy (ECT), repetitive trans-cranial magnetic stimulation (rTMS) and non-pharmacological modalities like cognitive behaviour therapy (CBT). At present, the level of evidence for the currently available treatment options of patients with schizophrenia and co-morbid OCD is low/poor. There are limited number of well-designed good-quality randomised controlled trials (RCTs).
Antipsychotics
Antipsychotics are known to cause and alleviate OCS/OCD. Various anti-psychotics have differential effects, which are related to the varying effects on serotonin and dopaminergic receptors. Second generation antipsychotics (SGAs), especially clozapine, olanzapine and risperidone have been known to cause/induce OCS/OCD. However, various SGAs with predominantly dopaminergic activities are also reported to reduce OCS/OCD. It is postulated that anti-serotonergic 5-HT2 property is pro-obsessive, whereas anti-dopaminergic property is anti-obsessive (Reference Schirmbeck, Rausch, Englisch, Eifler, Esslinger, Meyer-Lindenberg and Zink42,Reference Schirmbeck, Esslinger, Rausch, Englisch, Meyer-Lindenberg and Zink43). Evidence for role of antipsychotics in management of OCS/OCD comes from two types of studies, that is, those evaluating the beneficial effect of antipsychotics in patients with refractory OCD and from those studies evaluating the beneficial effect of antipsychotics among patients of schizophrenia with OCS/OCD (Fig. 2).
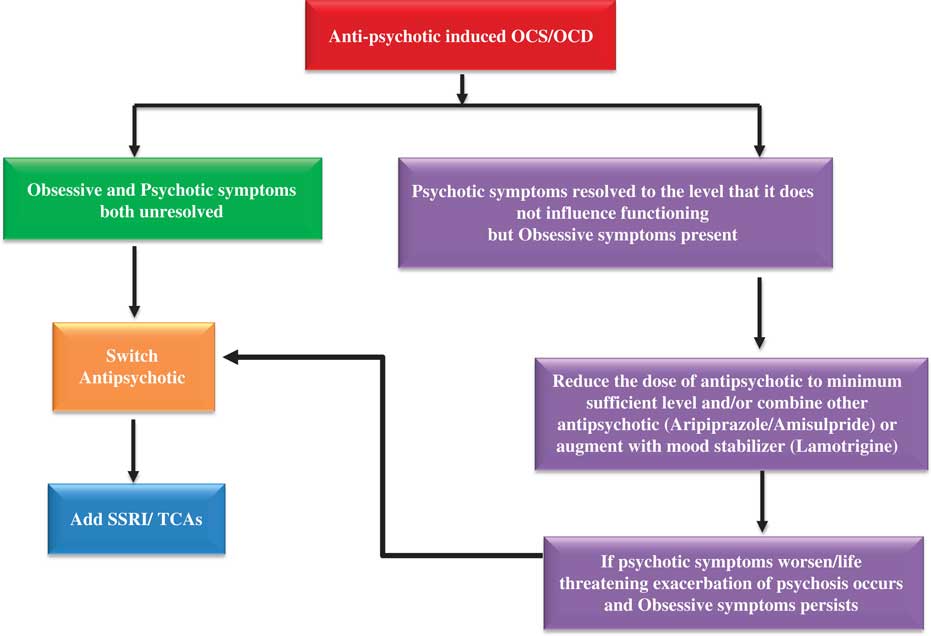
Fig. 2 Steps for management of antipsychotic induced OCS/OCD in Schizophrenia
Evidence of beneficial effect of SGAs in management of pure refractory OCD is more robust with the availability of multiple RCTs. A meta-analysis of studies evaluating the beneficial effect of antipsychotics among patients with treatment resistant OCD (TR-OCD) suggest that haloperidol, risperidone, aripiprazole and pimozide lead to improvement in the OCS, and olanzapine, quetiapine and clozapine do not have any beneficial effect on OCS (Reference Fernandez-Egea, Worbe, Bernardo and Robbins78). Previous meta-analysis have also reached to similar conclusions (Reference Veale, Miles, Smallcombe, Ghezai, Goldacre and Hodsoll79). However, data are limited to small sample size case studies with respect to the beneficial effect of antipsychotics in the management of OCS/OCD among patients with schizophrenia. Some studies have shown the beneficial effect of aripiprazole and amisulpride in treating denovo OCS as well as reversing the OCS secondary to other antipsychotics like clozapine (Reference Englisch, Esslinger, Inta, Weinbrenner, Peus, Gutschalk, Schirmbeck and Zink81–Reference Schönfelder, Schirmbeck, Waltereit, Englisch and Zink83). It is suggested that FGAs with a stronger D2 affinity are better than the ‘pines’ (i.e. olanzapine, quetiapine, clozapine) in the management of OCS among patients with schizophrenia. However, it is important to note that there is lack of high quality data evaluating the efficacy of antipsychotics in schizo-obsessive patients when compared with data on use of low dose add-on antipsychotics in pure OCD. Based on the current level of evidence, it is difficult to make any recommendations in favour of the use of any specific antipsychotics for management of OCS among patients with schizophrenia (Reference Poyurovsky84).
Antidepressants
Among the various antidepressants, clomipramine is the most studied drug. An initial double blind cross-over study which involved six patients with schizophrenia with comorbid OCS/OCD showed beneficial effect of clomipramine compared to placebo (Reference Berman, Sapers, Chang, Losonczy, Schmildler and Green85). Some case reports also support the use of clomipramine for the management of OCS in patients with schizophrenia (Reference Zohar, Kaplan and Benjamin86). However, some of the studies done in the last one decade or so, suggest that antidepressants, especially tricyclic antidepressants (TCAs) can lead to worsening of positive symptoms among patients with psychotic symptoms and hence careful considerations need to be made prior to starting of TCAs in patients with schizophrenia (Reference Kantrowitz and Tampi87). Among the SSRIs fluvoxamine is one of the best studied molecule with data available in the form of open label studies and case reports. Data from open label studies (Reference Poyurovsky, Isakov, Hromnikov, Modai, Rauchberger, Schneidman and Weizman88) and a RCT (Reference Reznik and Sirota89)suggest that fluvoxamine not only leads to considerable improvement in OCS but also leads to improvement in other symptoms of psychosis. Besides the data in the form of case reports, open label studies also support the beneficial effect of fluoxetine (Reference Agarwal and Agarwal90). Beneficial effect of paroxetine and sertraline are supported by few case reports (Reference Geller, Biederman, Stewart, Mullin, Farrell, Wagner, Emslie and Carpenter91–Reference Rahman, Grace, Pato and Priest93). To summarise, the evidence for effectiveness/efficacy of various antidepressants for management of OCS/OCD in patients with schizophrenia is based upon a limited number of inferior design studies and these do not allow for the direct comparison of treatment response. It is also quite evident that a substantial proportion of patients with schizophrenia with comorbid OCS/OCD do not respond to addition of a SSRI suggesting that OCS in schizophrenia are not readily amenable to anti-obsessional agents. An additional pitfall of the use of SSRI-antipsychotic drug combinations is the potential for clinically significant pharmacokinetic drug interactions, especially fluvoxamine and clozapine must be kept in mind while prescribing (Reference Hemeryck and Belpaire94).
Mood stabilisers
Evidence for glutaminergic dysfunction in OCS has emerged recently with a hypothesis that increased levels of glutamine as well as glutamate in brain causes OCS/OCD. It is proposed that mood-stabilisers reduce the extra-synaptic glutamate release and thus, can be of use in treatment of OCS/OCD in schizophrenia. Based on this hypothesis, these have been tried as augmenting agent to antipsychotics so as to overcome residual psychotic symptoms among patients with schizophrenia and among patients with treatment resistant OCD. Overall, the main concept behind using mood stabilisers (lamotrigine) as augmenter is to reduce the dosage of pro-obsessive SGAs (clozapine/olanzapine) (Reference Schirmbeck and Zink95,Reference Poyurovsky, Glick and Koran96). However, the results are conflicting and the evidence supporting the use of mood stabiliser is poor. An open-label study which included 11 patients showed beneficial effect in the form of some improvement in their OCS/OCD with lamotrigine in 5 out of 11 patients of schizophrenia with comorbid OCS/OCD (Reference Poyurovsky, Glick and Koran96). Evidence in the form of case reports also suggests improvement in OCS/OCD in patients with schizophrenia with the use of valproate (Reference Schwarz, Volz, Li and Leucht97). Overall, it can be said that there is very meager data on use of mood-stabilisers for OCS/OCD in schizophrenia.
CBT
Meta-analysis of case-reports supporting the use of CBT in OCS/OCD with schizophrenia shows that CBT is beneficial for both OCD and schizophrenia (Reference Schirmbeck and Zink25). However, it is important to note that for adequate application of CBT, the positive psychotic symptoms of the subject must be adequately controlled with antipsychotics.
Studies have found CBT to be safe (does not worsen psychosis) and well accepted (low discontinuation rate) and quite effective (similar to that of patients with pure OCD) (Reference Tundo and Necci98,Reference Tundo, Salvati, Spigno, Di Spigno, Cieri, Parena, Necci and Sciortino99).
A recent systematic review of studies evaluating the effectiveness of CBT for OCD in patients with psychosis which included eight case reports and one case series suggests that CBT is safe (does not worsen psychosis), well-accepted and quite effective in reduction of OCS in patients with psychosis with co-morbid OCD either induced by antipsychotics (de novo) or not induced by antipsychotics (OCD as a part of illness) (Reference Tundo and Necci98). The treatment guidelines [National Institute of Clinical Excellence Guidelines (NICE)] for schizophrenia also recommends CBT for co-morbid OCD in patients with schizophrenia (100).
ECT and rTMS
A meta-analysis of studies evaluating the effectiveness of ECT for the management of OCD in patients with schizophrenia which included 25 case-reports, 22 case-series, one cohort study, one non-randomised study and one case-control study, with total sample size of 186 in the meta-analysis revealed that only 3.1% of patients had psychosis/mania/agitation along with OCS/OCD and of all patients only <50% responded to ECT (Reference Fontenelle, Coutinho, Lins-Martins, Fitzgerald, Fujiwara and Yücel101). Similarly, a case-series (n=3) (Reference Mendes-Filho, Belmonte-de-Abreu, Pedrini, Cachoeira and Lobato102) and a double blind RCT (n=12) (Reference Mendes-Filho, De Jesus, Belmonte-de-Abreu, Cachoeira and Rodrigues Lobato103), evaluated the usefulness of rTMS for the management of OCS/OCD in patients with schizophrenia revealed some improvement at 4 weeks, but there was subsequent relapse after discontinuing treatment for a month (Reference Mendes-Filho, Belmonte-de-Abreu, Pedrini, Cachoeira and Lobato102) and the outcome measures were not statistically significant (Reference Mendes-Filho, De Jesus, Belmonte-de-Abreu, Cachoeira and Rodrigues Lobato103). These findings suggest that ECT or rTMS might not be very useful modalities in managing OCS/OCD in schizophrenia as there is no robust evidence in favour of their efficacy in managing OCS/OCD in schizophrenia. However, further studies are needed to prove or refute these findings.
Available treatment guidelines for the management of OCS/OCD in schizophrenia
American Psychiatric Association (APA) (Reference Lehman, Lieberman, Dixon, McGlashan, Miller, Perkins and Kreyenbuhl104) guidelines for management of schizophrenia suggest addition of antidepressant for the management of OCS/OCD along with close monitoring for exacerbation of psychosis. Other treatment options include switching to another SGA, or attempting a trial of CBT. APA guidelines also suggest hospitalisation and ECT if required based on clinical judgement.
NICE guidelines (100) suggests inpatient treatment as well as ECT if required for patients with schizophrenia with comorbid OCD. Further, it makes a note of carrying out further research for the evaluation of ‘anti-obsessional agents’ in management of comorbid OCS/OCD in schizophrenia.
Based upon the available literature, it is difficult to make any robust evidence based recommendations for management of OCS/OCD among patients with schizophrenia. Therefore, based on the available evidence in terms of association of OCS/OCD with schizophrenia and effectiveness data, we attempt to formulate certain general treatment recommendations, which can be practiced on case to case basis, after considering various clinical aspects.
First and foremost step in management is assessment of relationship of OCS/OCD with symptoms of schizophrenia and use of antipsychotic medications (Reference Poyurovsky105) (Fig. 1). Next step involves assessment of severity of OCS/OCD and positive psychotic symptoms.
It is generally suggested that OCS/OCD which occur as part of ARMS of schizophrenia, usually recovers with onset of full-fledged psychotic symptoms and hence, no specific treatment for OCS/OCD may be required in most cases. When comorbid OCD occurs during the acute phase of illness and it persists and worsens regardless of symptoms of schizophrenia as an independent co-existing disorder then, there is need to treat OCD and schizophrenia as two separate disorders. In such a scenario a SSRIs/ TCAs should be added to the antipsychotic regimen being used to manage psychotic symptoms. However, these patients must be closely monitored for worsening of psychotic symptoms. If the OCS/OCD occurs denovo as a result of use of antipsychotic medications (second generations antipsychotics, mostly clozapine), then at the first step, if the clinical situation permits, than an attempt must be made to reduce the dose of antipsychotic medication implicated in the causation of OCS/OCD. In many cases, minor reduction in the antipsychotic dosage may help in improving the OCS. However, if OCS/OCD does not resolve or there is worsening of psychosis than a change of antipsychotic must be considered. However, the situation becomes tricky, especially when the OCS/OCD is associated with use of clozapine. The pros of stopping clozapine must be weighed against the risk of emergence of threatening exacerbation /severe worsening of psychosis. Further, currently there is no evidence to support to make the recommendation that patient should be switched from clozapine to any other antipsychotics due to clozapine induced OCS. Hence, it is important to provide information to the patient and caregivers about the possibility and an informed decision must be taken. If a change is agreed upon, then the antipsychotic with lower risk of inducing OCS/OCD, such as amisulpride, aripiprazole and FGAs must be chosen. However, if OCS/OCD persist despite change of antipsychotics then, addition of a SSRI/TCAs need to be considered (See Fig. 3).
If the OCS/OCD is a part of acute psychotic illness then it usually improves with the improvement in psychotic symptoms. In such a case, the main stay of treatment are anti-psychotics with preferred antipsychotics being those with lower anti-obsessive potential (e.g. amisulpride, aripiprazole and risperidone). However, if the OCS/OCD does not resolve with use of antipsychotic medication, than the management is usually determined by the severity of both OCS/OCD and psychotic symptoms. If both OCS/OCD and psychotic symptoms are unresolved after initial adequate trial with an antipsychotic, then switch to another antipsychotic is to be considered. However, if the initial antipsychotic trial lead to resolution of psychotic symptoms without much benefit in the OCS/OCD than addition of SSRI is a good strategy. If an adequate trial of SSRI does not lead to improvement in OCS/OCD than a change of antipsychotic to amisulpride or aripiprazole may be considered. If initial antipsychotic trial lead to worsening of OCS with improvement in psychotic symptoms, than reduction of dosage of the current antipsychotic or addition of other antipsychotic (aripiprazole/amisulpride) and /or augmentation with mood stabiliser (lamotrigine) may be considered with close monitoring for psychotic relapse (Reference Poyurovsky105,Reference Poyurovsky, Zohar, Glick, Koran, Weizman, Tandon and Weizman106). In case there is no response in OCS/OCD even after reducing the dose of antipsychotic medication then addition of SSRI is to be considered. Further in case there is no change in severity of OCS/OCD even after adding SSRI, then change of antipsychotic to amisulpride or aripiprazole can be considered (Fig. 3).

Fig. 3 Use of antipsychotics in management of OCS/OCD in Schizophrenia
If OCS/OCD is seen as an aftermath of psychosis, that is, OCS/OCD emerges when the positive psychotic symptoms are receding or have receded, in such a scenario OCS/OCD usually improves on its own with further improvement in symptoms of schizophrenia and no special treatment may be needed for same. However, if this does not occur, than SSRIs or CBT can be considered.
In all the above mentioned sequences of OCS/OCD and psychotic symptoms, it is important to recognise OCS/OCD at the earliest. It is important to remember that in all the scenarios, CBT is always an option in patients of mild to moderate OCS with fully treated psychosis or those with good level of insight. ECT can be considered as a last resort treatment. While using antidepressants, the clinicians must monitor the patients closely for worsening of psychosis. Further, while using combination of antipsychotics and antidepressants, pharmacokinetic and pharmacodynamic interactions must be kept in mind, in selecting the various agents. Further, if a combination does not lead to desirable effect than stopping one of the agents, depending on the clinical situation must always be practiced.
Conclusions
Prevalence of OCS/OCD in patients with schizophrenia is much higher than prevalence in general population. OCS/OCD is seen in all the stages of schizophrenia, starting from ARMS to chronic/ stabilisation/deficit phases. Putative etiological factors responsible for the presence of OCS/OCD in schizophrenia are still to be clarified. A proportion of OCS/OCD in schizophrenia can be attributed to use of SGAs. Presence of OCS/OCD is associated with higher severity of symptoms of schizophrenia and more negative outcome. Symptom profile of OCS/OCD in schizophrenia is similar to that seen in patients with OCD only. Treatment strategies are not well evaluated, but there is an upsurge in the evidence pointing towards certain antipsychotics, antidepressants and CBT.
Acknowledgements
None






