INTRODUCTION
Physical activity is associated with a range of health benefits, and its absence can have harmful effects on health and well-being, increasing the risk for coronary heart disease, diabetes, certain cancers, obesity, hypertension and all-cause mortality (CDC, 1996). Physical inactivity may also be associated with the development of mental disorders; some clinical and epidemiological studies have shown associations between physical activity and symptoms of depression and anxiety in cross-sectional and prospective-longitudinal studies (Farmer et al. Reference Farmer, Locke, Mosciki, Dannenberg, Larson and Radloff1988; Bhui & Flechter, Reference Bhui and Fletcher2000; Lampinen et al. Reference Lampinen, Heikkinen and Ruopplia2000; Dunn et al. Reference Dunn, Trivedi and O'Neal2001; Goodwin, Reference Goodwin2003; Abu-Omar et al. Reference Abu-Omar, Rütten and Lehtinen2004; Haarasilta et al. Reference Haarasilta, Marttunen, Kapiro and Aro2004; Motl et al. Reference Motl, Birnbaum, Kubik and Dishman2004). Although the issue of physical activity has been addressed in substance use prevention studies with mixed results (Collingwood et al. Reference Collingwood, Sunderlin, Reynolds and Kohl2000), little is known about the effect of physical activity on the risk of developing other incident or recurrent mental disorders as defined by DSM-IV.
In the present study, we aimed to examine (1) the cross-sectional baseline association of regular physical activity with 12-month and lifetime mental disorders according to DSM-IV criteria, and (2) whether regular physical activity at baseline is prospectively associated with decreased risks of incident DSM-IV mental disorders in adolescence and young adulthood as the peak period for first onset of most mental disorders. Because age, gender and educational status (Bhui & Fletcher, Reference Bhui and Fletcher2000; Dunn et al. Reference Dunn, Trivedi and O'Neal2001) may significantly interact with physical activity, we (3) also examined the effect of interaction of these factors with physical activity on the prevalence and incidence of mental disorders. We used data from a 4-year prospective-longitudinal epidemiological community survey of over 2500 individuals aged 14–24 years at the outset of the study.
METHOD
Subjects and setting
The Early Developmental Stages of Psychopathology (EDSP) is a prospective cohort study of the prevalence, incidence, familial risk and other risk factors, co-morbidity, and the course of mental disorders in a representative sample of adolescents and young adults in Munich, Germany. The study consists of a baseline survey, three follow-up surveys, and two family supplements. The baseline sample was drawn randomly from the 1994 government registries of all residents aged 14–24 years in metropolitan Munich and the surrounding counties. Respondents aged 14–15 and 16–21 years were sampled at four and two times the probability of 22- to 24-year-olds respectively. A detailed description of the study and details about the sampling, representativeness and characteristics of the sample have been reported previously (Wittchen et al. Reference Wittchen, Perkonigg, Lachner and Nelson1999; Lieb et al. Reference Lieb, Isensee, Sydow and Wittchen2000). The baseline survey was conducted in 1995 (n=3021; response rate 74·6%). The first follow-up study was conducted on average 20 months later only for subjects from 14 to 17 years of age at baseline (n=1228). The second and third follow-up studies were conducted for all subjects (second follow-up: 42 months after baseline, n=2548; third follow-up: 8·4 years after baseline, n=2210). Taking into account a wide range of variables (age, education, mental disorders), no evidence was found for selective attrition in the total sample from the baseline to the third follow-up, except for subjects with substance use disorders. The younger cohort had up to four and the older cohort up to three assessments.
For the purpose of the present analyses, only 2548 respondents with a full data set (conditional wave 2 follow-up response rate: 84·3%) from all applicable waves were considered for the cross-sectional analyses. Analyses for incident disorders are based on the subset of individuals not having the respective diagnoses at baseline. Thus, for each diagnostic level, fewer individuals were analysed accordingly. At the final follow-up, 61% of the sample had completed higher education (13+ years), 29% had middle education (11–12 years of schooling) and 10% had only visited the mandatory school (9–10 years of schooling) and had no further schooling. Sixty-two per cent were employed, 21% attended university or some kind of vocational training and 0·3% still attended school. With regard to marital status, 74% were single, 23% married and 3% separated, divorced or widowed.
Diagnostic assessment
At baseline and follow-up, diagnostic assessments according to DSM-IV were based on the computer-assisted version of the Munich-Composite International Diagnostic Interview (DIA-X/M-CIDI; Wittchen, Reference Wittchen1994). The interview covers somatoform disorder, anxiety disorders including post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder, mood and substance disorders, including nicotine dependence, and also eating disorders. At baseline, the lifetime and 12-month versions of the CIDI were used, at the first and second follow-ups the interval and 12-month versions were applied to assess incident diagnoses as well as changes in the diagnostic status. The reliability and validity of the M-CIDI have been investigated extensively and reported previously (Wittchen, Reference Wittchen1994). Diagnostic findings and co-morbidity rates were obtained by using the M-CIDI/DSM-IV diagnostic algorithms. Interviews at all waves were administered by highly trained clinical interviewers, most of whom were clinical psychologists.
Assessment of physical activity
Physical activity was assessed in a series of four questions as part of an interview module, at baseline and follow-up. Subsequent to gate questions (Do you exercise?/Do you engage in any sports activities?), the interview probed all individuals acknowledging the gate question further by asking: What kind of sports? (verbatim description). The interviewer was further prompted to assess the frequency of physical activity (How frequently do you exercise?) by using the following coding options: daily, several times a week, once a week, 1–3 times a month, less than once a month. For the present analysis these codings were grouped into three categories: (a) daily and several times a week (‘regular’), (b) 1–4 times a month (‘non-regular’) and (c) less than once a month or no exercise at all (‘no’).
Analyses
Cross-sectional associations between physical activity and mental disorders were calculated using the 12-month data from the baseline assessment, estimating logistic regressions controlling for age and gender. In additional analyses, educational status, body mass index (BMI), other mental disorders and the number of impairment days due to physical problems in the last 4 weeks before baseline assessment were included in the logistical model to examine whether the association for any incident mental disorder was attenuated when controlling for (a) education and (b) health-related factors. Prospective analyses used the baseline physical activity status information among unaffected individuals, taking the onset of incident disorders as the outcome. Incidence rates were calculated for each diagnosis, groups of disorders, any mental disorder, and also the presence of co-morbid diagnoses. For depressive disorders we also examined whether baseline physical status was related to the number and the duration of incident depressive episodes. Analyses were performed using Stata 9 (Stata Corporation, College Station, TX, USA) and applying the information sandwich estimator for accurate assessment of the precision of estimated measures in the case of weighted data. Associations with categorical outcomes (non-regular, regular versus no physical activity) were quantified with odds ratios (ORs) and 95% confidence intervals (CIs) from (multinomial) logistic regression. Associations with count variables as outcomes (e.g. the number of depressive episodes) were assessed with mean ratios from negative binominal regression after subtracting the minimum possible value (=1 for the number of possible depressive episodes among individuals with a depressive disorder) from the outcome. We also aimed to assess the possible interaction of gender, age and physical activity on the prevalence and incidence of mental disorders. We did not adjust for multiple testing because we considered specific mental disorders to be related to individual hypotheses.
The population attributable fraction (PAF) was computed for the diagnoses found in the prospective analyses to be related to regular physical activity (in the total sample or among females or males respectively). PAF is defined as the fraction of incident cases that could potentially be prevented if a risk factor had not been present in a single individual provided that the association found was causal and the binary factor was not preventive for any individual. We therefore computed the PAFs of no regular (versus no or non-regular) physical activity. PAF is a function of both the risk ratio and the prevalence of the risk factor and increases as one or both quantities increase. We used the aflogit procedure of Stata, which computes PAFs on the basis of the previously fitted logistic regression (Greenland & Drescher, Reference Greenland and Drescher1993).
RESULTS
Physical activity and sociodemographic variables
The following analyses are based on the 2548 individuals who completed the T0 and T2 investigations. At baseline, 50·2% of individuals reported regular, 14·6% non-regular and 35·2% no physical activity. At follow-up, regular physical activity was reported by 44·5%, non-regular by 17% and no physical activity by 38·5% of the participants. Table 1 reports the baseline sociodemographic variables by physical activity in the sample and shows that males were more likely than females (58·1% v. 42·0%; OR 0·4, 95% CI 0·3–0·5) to report current regular physical activity versus no current activity. There is also evidence for an age difference, revealing that the rate of physical activity was lower in the older age group (OR 0·6, 95% CI 0·5–0·7). In addition, we found a significant interaction indicating that the reduction in physical activity in 18- to 24-year-olds versus 14- to 17-year-olds was 1·5 times as high (95% CI 1·1–2·1) in females than in males. A middle or high educational level was also associated with higher rates of regular (OR 2·7, 95% CI 1·6–4·4 and OR 4·2, 95% CI 2·6–6·8 respectively) and non-regular (OR 1·4, 95% CI 1·1–1·9 and OR 2·4, 95% CI 1·8–3·2 respectively) physical activity.
Table 1. Physical activity of respondents (n=2548) at baseline by sociodemographic variablesFootnote a
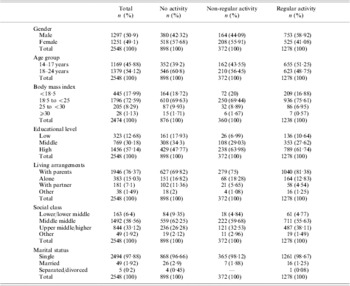
a Percentages have been weighted.
Baseline associations of mental disorders and physical activity
At baseline, individuals with regular physical activity were less likely to meet criteria for any DSM-IV mental disorder (35·2%; OR 0·7, 95% CI 0·6–0·8) than subjects with no physical activity (46·1%) (Table 2). They were also less likely to have co-morbid conditions (OR 0·7, 95% CI 0·6–0·9). The lower 12-month rates among those with regular activity were largely due to significantly lower rates for any anxiety disorder (OR 0·7, 95% CI 0·5–0·9) and lower rates for substance use disorders (OR 0·6, 95% CI 0·5–0·8). Among mood disorders, only dysthymia was significantly associated with regular physical activity (OR 0·5, 95% CI 0·2–0·9). Findings for non-regular physical activity were relatively similar; however, possibly because of the lower number of subjects in this groups, the results seem to be less consistent and do not reach significance except for nicotine dependence (OR 0·5, 95% CI 0·4–0·8). Associations of baseline physical activity with lifetime mental disorders revealed almost identical findings (data available on request).
Table 2. Twelve-month prevalences and associations of mental disorders according to physical activity at baseline (n=2548)Footnote a

CI, Confidence interval; OR, odds ratio.
a Percentages have been weighted. ORs were derived from logistic regressions while adjusting for gender and age.
b Significant at p<0·05.
Incidence of mental disorders in the follow-up period and physical activity
The following analyses are based on 2548 individuals who completed T0 and T2 minus those who met lifetime criteria for the respective disorder at T0. Taking a strictly prospective approach, Table 3 reports the incidence rates of mental disorders over the 4-year follow-up period by respondents' baseline physical activity status, along with ORs estimated with logistic regressions controlling for age and gender. Overall, the prospective analyses revealed that individuals with regular and non-regular physical activity at baseline had a substantially reduced risk compared to the reference group (no activity) to (a) experience any incident disorder (OR 0·4, 95% CI 0·3–0·7 and OR 0·7, 95% CI 0·5–0·9 respectively) and (b) to develop co-morbid conditions (OR 0·5, 95% CI 0·2–0·9 and OR 0·8, 95% CI 0·5–1·1 respectively). These findings remained unchanged when controlling additionally for (a) educational status and (b) BMI, other mental disorders and impairment days due to physical problems.
Table 3. Four-year follow-up incidence of mental disorders according to physical activity level at baselineFootnote a

CI, Confidence interval; OR, odds ratio.
a Percentages have been weighted. ORs were derived from logistic regressions while adjusting for gender and age.
b n's vary according to the number of indi for the respective disorder at T0.
c Significant at p<0·05.
Anxiety disorders
Except for obsessive-compulsive disorder and generalized anxiety disorder among individuals with non-regular activity, the 5-year incidence of any anxiety disorder was considerably lower in the regular and non-regular activity groups as compared to the group without baseline physical activity. Consistent with the cross-sectional findings, any anxiety disorders were less frequent among those with regular physical activity as compared to those with no activity (OR 0·5, 95% CI 0·4–0·7). For specific anxiety disorders, however, this could only be shown for agoraphobia (OR 0·4, 95% CI 0·2–0·8) and specific phobia (OR 0·6, 95% CI 0·40–0·9). In addition, the 4-year incidence of agoraphobia and PTSD was significantly lower in the non-regular activity group than in the no activity group.
Mood disorders
Associations for mood disorders were variable. Significant lower risks were found for dysthymia in the regular versus no physical activities comparison, whereas for bipolar disorder the risk was increased in both the regular and the non-regular group as compared to the reference group without physical activity. For major depressive disorder (MDD), incidence rates in the sample were lower in both activity groups as in the reference group, but did not reach significance. We also examined whether physical activity was related to the duration and the number of episodes and found no consistent results.
Substance use disorders
For substance use disorders the findings suggested lower incidence rates in both the non-regular and regular activity groups compared to the group without baseline physical activity; however, the OR was only significant in the aggregated group of any substance use disorder (OR 0·7, 95% CI 0·5–1·0). We further explored this issue by examining cross-sectional associations, as well as collapsing regular and non-regular activity. However, the findings did not get any clearer. For alcohol abuse, the incidence rate in the sample was higher in the regular activity group, but was not significant (OR 1·4, 95% CI 1·0–2·0).
Eating and somatoform disorders
For eating disorders there was no significant association with regular physical activity level. The rates for any somatoform disorder/syndrome (persistent pain, somatization and undifferentiated somatoform disorders) were significantly lower in the physical activity groups as compared to the reference group (OR 0·7, 95% CI 0·5–0·97 for the non-regular and OR 0·7, 95% CI 0·5–0·9 for the regular group).
Interaction of gender, age and physical activity
Prevalence of mental disorders
For the 21 outcome diagnoses we found nine two-way interactions, three with sex and six with age. Seven of them occurred for non-regular versus no physical activity, most of them indicating particularly decreased rates of disorders in younger participants and in women respectively (data available on request). In females, regular physical activity was stronger associated with lower rates of alcohol dependence (OR 0·6, 95% CI 0·08–0·9); in younger respondents, regular physical activity was more strongly associated with lower rates of illicit substance abuse (OR 1·4, 95% CI 1·2–1·7, per year of age). Moreover, we found three three-way interactions: (a) non-regular activity was associated with lower rates of specific phobia in older (baseline 18–24) females (OR 1·3, 95% CI 1·02–1·7, per year of age); and regular activity was associated with lower rates of (b) nicotine dependence (OR 0·9, 95% CI 0·8–0·98) and (c) any substance abuse diagnosis (OR 0·9, 95% CI 0·8–0·95) in older females.
Incidence of mental disorders
We found nine significant two-way interactions, again three with sex and six with age; eight of these interactions were found for non-regular physical activity, indicating particularly decreased disorder rates in females and an inconsistent pattern over age (data available on request). Regular physical activity increased the incidence for bipolar disorders in older probands (OR 1·51, 95% CI 1·32–1·72, per year of age). In addition, we found four three-way interactions, all with regular activity. Regular activity appeared to be particularly protective for mood disorder in older males (OR 1·2, 95% CI 1·01–1·3, per year of age) as well as for any incident mental disorder (OR 1·2, 95% CI 1·1–1·3), any incident substance abuse disorder (OR 1·2, 95% CI 1·07–1·3) and incidence of alcohol dependence (OR 1·2, 95% CI 1·1–1·4) in older females.
Population attributable risk fraction
We repeated the analyses in Table 3 separately for males and females to see whether there were significant differences not found in the overall analyses. Incident MDD (OR 0·5, 95% CI 0·3–0·8) and PTSD (OR 0·1, 95% CI 0·02–0·4) were predicted by regular versus no activity only in males. No additional differences were found for females. In males the PAFs were 48·0% [standard error of the mean (s.e.m.=21·6)] for agoraphobia, 38·2% (s.e.m.=13·1) for specific phobia, 86·9% (s.e.m.=33·2) for PTSD, 34·1% (s.e.m.=10·6) for MDD, 59·5% (s.e.m.=17·6) for dysthymia and 19·0% (s.e.m.=6·7) for any somatoform disorder/syndrome. In females the PAFs were smaller: 29·3% (s.e.m.=22·4) for agoraphobia, 14·1% (s.e.m.=9·7) for specific phobia, 77·4 (s.e.m.=21·5) for PTSD, 30·2% (20·9%) for dysthymia and 6·2% (s.e.m.=4·2) for any somatoform disorder/syndrome. These differences are due to higher risk ratios in males because no regular activity was more frequent in females (59·0 v. 44·6% in the entire baseline sample).
DISCUSSION
Overall, the cross-sectional and prospective-longitudinal analyses suggest that physical activity is associated with lower rates of mental disorder and a substantially reduced incidence of mental disorder, particularly the frequency of co-morbid disorders, suggesting a substantial protective effect, especially in those with regular, daily or more frequent, participation in sports. The association of regular activity with mental disorder differs by age and gender and type of disorder. Significant associations were found for anxiety disorders such as agoraphobia, specific phobia and PTSD, for somatoform disorders, dysthymia and less consistently for substance dependence, which all revealed lower rates among those with regular physical activity and were less impressive for non-regular activity levels. By contrast, regular and non-regular physical activity at baseline was associated with increased incidence rates of bipolar disorder. Limitations of our study include the lack of objective indicators of physical activity and fitness and the sample size, which might be unable to detect minor associations of physical activity with rare diagnostic categories.
To our knowledge, this is the first large-scale study to explore prospectively, and in detail, the relationship between levels of physical activity and sports, assessed by interview, and a wide range of DSM-IV mental disorders in a community during the peak risk period for the onset of most mental disorders. Our finding that respondents undertaking sports have a decreased risk for the onset of mental disorders, however, is not entirely new. Exercise treatment components have been reported to be valuable not only in the treatment of depression and anxiety disorders (Orwin, Reference Orwin1973; Broocks et al. Reference Broocks, Bandelow, Pekrun, George, Meyer, Bartmann, Hillmer-Vogel and Rüther1998; Ströhle et al. Reference Ströhle, Feller, Onken, Godemann, Heinz and Dimeo2005) but also in substance use disorders such as alcohol or nicotine dependence (Palmer et al. Reference Palmer, Vacc and Epstein1988; Russell et al. Reference Russell, Epstein, Johnston, Block and Blair1988). In addition, cross-sectional studies have repeatedly pointed out the relevance of this association (Goodwin, Reference Goodwin2003; Abu-Omar et al. Reference Abu-Omar, Rütten and Lehtinen2004; Motl et al. Reference Motl, Birnbaum, Kubik and Dishman2004). These studies were, however, based on less comprehensive psychopathological coverage. An important difference from previous studies is that we found no consistent cross-sectional or prospective associations of physical activity and major depression, as highlighted, for example, by Goodwin (Reference Goodwin2003) or Motl et al. (Reference Motl, Birnbaum, Kubik and Dishman2004). Future studies on the association of physical activity and mental disorder are advised to use a recently established measure of physical activity (Craig et al. Reference Craig, Marshall, Sjostrom, Baumann, Booth, Ainsworth, Pratt, Ekelund, Yngve, Sallis and Oja2003). In addition, fitness, energy expenditure, organized sporting activities in groups versus personal conditioning as well as school versus sports clubs activities should be recorded.
We have demonstrated in our analyses that associations between physical exercise and mental disorder are partly diagnosis specific. Our finding that physical activity is associated with increased incidence rates of bipolar disorder is particularly significant and has not been reported before. Given the time-frame of assessment and the fact that the point prevalence of bipolar disorder was only a fraction of the 12-month rate, it is unlikely that prodromal or acute bipolar symptomatology has directly affected this association. It is more likely that non-clinical dispositions (traits) are involved. Because we also found an association between prior bipolar disorder and subsequent onset of exercise participation (data available on request), models of shared vulnerability may explain the relationship between these two phenomena. However, because of the small number of individuals with bipolar disorder, this result needs to be replicated in a larger sample. Similar effects have also been seen in some exploratory analyses for anorexia nervosa, but low base rates meant that we were unable to substantiate this observation. These findings might suggest that individuals with increased risk for bipolar disorder and possible for eating disorders probably need to be treated differentially if physical activity is thought to prevent mental disorders.
Developmental, neurobiological and psychological factors (Cohen & Rodriguez, Reference Cohen and Rodriguez1995; Cotman & Berchtold, Reference Cotman and Berchtold2002) might underlie, mediate and/or moderate the association of physical activity and some mental disorders in a very dynamic way. Thus, the effects of physical activity might stimulate a complex system and trigger a cascade of events that, for example, result in higher resilience to mental disorders (Cohen & Rodriguez, Reference Cohen and Rodriguez1995; Cotman & Berchtold, Reference Cotman and Berchtold2002; Charney, Reference Charney2004). Further characterization and randomized intervention studies are needed before we can conclude that participating in sports is a promising target to prevent the onset of specific anxiety disorders, dysthymia, substance dependence and somatoform disorders. Such a preventive effect may be especially relevant for individuals at high risk for these disorders either encoded genetically, acquired during pre-morbid life, or as an imprint from previous disease episodes or traumatic events (Ströhle & Holsboer, Reference Ströhle and Holsboer2003). In this context it is a notable that some of our PAFs were very high, especially in males (e.g. 86·9% for PTSD). These high values might be due to large random error or bias (e.g. shared factors that affect both lack of physical activity and mental disorder). However, even if the true PAFs were only a fraction of our certainly biased estimates, the benefit of intervening by increasing physical activity would be substantial. Note that the effect of prevention always depends on the mode of invention in a multivariate framework (Greenland, Reference Greenland2005) and regular physical activity may be more preventive (Pate et al. Reference Pate, Pratt and Blair1995). Unfortunately, however, the study was not powered and designed to reveal clear evidence of whether physical activity should be addressed within universal or more targeted preventive efforts. However, limiting speculation to mental disorders, the partially differential diagnostic associations seem to suggest that targeted interventions might be more promising.
In summary, our results suggest that physical inactivity might be associated with the development of not only some major medical but also some major mental disorders. Our data underscore the possibility that physical activity, exercise or sports participation might be a promising target for research on factors that might prevent the onset of anxiety disorders, dysthymia and somatoform disorders.
APPENDIX. EDSP Study Group
Principal investigators: Dr Hans-Ulrich Wittchen, Dr Roselind Lieb. Core staff members: Dr Kirsten von Sydow, Dr Gabriele Lachner, Dr Axel Perkonigg, Dr Peter Schuster, Dipl.-Stat. Michael Höfler, Dipl.-Psych. Holger Sonntag, Dipl.-Psych. Tanja Brückl, Dipl.-Psych. Elzbieta Garczynski, Dr Barbara Isensee, Dipl.-Psych. Agnes Nocon, Dr Chris Nelson, Dipl.-Inf. Hildegard Pfister, Dr Victoria Reed, Dipl.-Soz. Barbara Spiegel, Dipl.-Psych. Andrea Schreier, Dr Ursula Wunderlich, Dr Petra Zimmermann, Dipl.-Psych. Katja Beesdo and Dipl.-Psych. Antje Bittner. Scientific advisors: Dr Jules Angst (Zurich), Dr Jürgen Margraf (Basel), Dr Günther Esser (Potsdam), Dr Kathleen Merikangas (NIMH, Bethesda), Dr Ron Kessler (Harvard, Boston) and Dr Jim van Os (Maastricht).
ACKNOWLEDGEMENTS
This work was part of the Early Developmental Stages of Psychopathology (EDSP) Study and was funded by the German Ministry of Research and Technology, project nos 01EB9405/6, 01EB 9901/6 and EB01016200. The fieldwork and analyses were also partially supported by grants from the Deutsche Forschungsgemeinschaft (DFG) LA1148/1-1 and WI2246/1-1.
DECLARATION OF INTEREST
None.





