Hierarchical structure of psychopathology
Categorical diagnostic systems such as the DSM and ICD have well documented problems, including excessive co-occurrence between putatively discrete diagnoses, and inaccurate mapping onto putative etiological factors (e.g. genetic and neurobiological underpinnings; e.g. Brainstorm consortium, 2018; Zald & Lahey, Reference Zald and Lahey2017). Quantitative dimensional models of psychopathology have been proposed as a viable alternative that solves many of the problems inherent in existing categorical systems. For instance, the Hierarchical Taxonomy Of Psychopathology (HiTOP) consortium recently proposed a dimensional model of psychopathology based on evidence accumulating in the past few decades (Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby and Zimmerman2017).
The model organizes homogeneous signs and symptoms (e.g. anhedonia) into a hierarchy of increasingly general constructs that range from disorders/syndromes [e.g. major depressive disorder (MDD) and social anxiety disorder] to subfactors (e.g. fear disorders and eating pathology) to broad spectra (e.g. internalizing, externalizing, and thought disorders). This hierarchical arrangement allows researchers to consider whether risk factors (e.g. genetic or neurobiological factors) contribute to psychopathology at different levels of specificity (Conway et al., Reference Conway, Forbes, Forbush, Fried, Hallquist, Kotov and Eaton2019; Gillan et al., Reference Gillan, Kalanthroff, Evans, Weingarden, Jacoby, Gershkovich and Simpson2020). It is assumed that while some risk factors may contribute to individual disorders (e.g. MDD) or symptoms (e.g. anhedonia) others confer risk to a broad set of psychopathologies (e.g. internalizing disorders).
The structure of obsessive-compulsive and related disorders
Although significant progress has been made in determining the hierarchical structure of common disorders, such as mood and anxiety disorders, there is a paucity of data available on the transdiagnostic structure underlying obsessive-compulsive spectrum disorders (Watson, Reference Watson2005; Watson, Stasik-O'Brien, Ellickson-Larew, & Stanton, Reference Watson, Stasik-O'Brien, Ellickson-Larew and Stanton2018). The aim of the current study was to begin filling this gap by examining the higher-order structure of the obsessive-compulsive and related disorders (OCRDs) in DSM-5. The OCRD chapter (APA, 2013) includes five main diagnoses: obsessive-compulsive disorder (OCD), hoarding disorder (HD), body dysmorphic disorder (BDD), trichotillomania (hair-pulling disorder; HPD), and excoriation (skin-picking) disorder (SPD). The decision to group these disorders together (Phillips et al., Reference Phillips, Stein, Rauch, Hollander, Fallon, Barsky and Leckman2010; Stein et al., Reference Stein, Grant, Franklin, Keuthen, Lochner, Singer and Woods2010) was based on evidence showing that these disorders share broad similarities in symptom presentation (e.g. compulsive/repetitive behaviors) and other clinical validators (e.g. shared family history; Bienvenu et al., Reference Bienvenu, Samuels, Wuyek, Liang, Wang, Grados and Nestadt2012). However, no consensus exists about the scope or the nature of the ‘OC spectrum’ (Hollander, Friedberg, Wasserman, Yeh, & Iyengar, Reference Hollander, Friedberg, Wasserman, Yeh, Iyengar, Abramowitz and Houts2005) and the OCRD chapter in DSM-5 has been controversial. Specifically, the inclusion of HPD and SPD in the chapter has been debated (Abramowitz & Jacoby, Reference Abramowitz and Jacoby2015).
HPD and SPD share strikingly similar symptom presentation with each other (Snorrason, Belleau, & Woods, Reference Snorrason, Belleau and Woods2012); however, the two disorders differ in important ways from other OCRDs. Most notably, both HPD (Snorrason et al., Reference Snorrason, Ricketts, Olafsson, Rozenman, Colwell and Piacentini2018) and SPD (Snorrason, Olafsson, Houghton, Woods, & Lee, Reference Snorrason, Olafsson, Houghton, Woods and Lee2015) are characterized by appetitive urges to engage in the compulsive/repetitive behaviors (hair pulling and skin picking) and pleasure or gratification during the act. This is not typical of other OCRDs. Repetitive acts in OCD and BDD are usually associated with aversive internal events such as distressing thoughts, fear, disgust, or a sense of incompleteness. Hoarding behaviors in HD, although more ego-syntonic than symptoms of OCD and BDD (Grisham, Williams, & Kadib, Reference Grisham, Williams, Kadib and Johnson2010), rarely involve the same immediate sense of pleasure or gratification that is characteristic of hair pulling and skin picking in HPD and SPD. Thus, diagnostic concepts other than OCRDs have often been used to describe SPD and HPD, including impulse control disorders (APA, 2000), behavioral addictions (Grant, Odlaug, & Potenza, Reference Grant, Odlaug and Potenza2007), grooming disorders (Bienvenu et al., Reference Bienvenu, Wang, Shugart, Welch, Grados, Fyer and Nestadt2009), and body-focused repetitive behavior (BFRB) disorders (APA, 2013; Stein et al., Reference Stein, Grant, Franklin, Keuthen, Lochner, Singer and Woods2010). Similarly, several theorists organize psychopathology along impulsive-compulsive dimensions (e.g. Berlin & Hollander, Reference Berlin and Hollander2014; Robbins, Gillan, Smith, de Wit, & Ersche, Reference Robbins, Gillan, Smith, de Wit and Ersche2012) where it is assumed that SPD/HPD belong to the impulsive dimension and other OCRDs to the compulsive dimension.
Twin research indicates that symptoms of OCD, BDD, and HD share a common genetic risk factor (López-Solà et al., Reference López-Solà, Fontenelle, Bui, Hopper, Pantelis, Yücel and Harrison2016; Monzani, Rijsdijk, Harris, & Mataix-Cols, Reference Monzani, Rijsdijk, Harris and Mataix-Cols2014) that also has substantial genetic correlation with symptoms of anxiety disorders (López-Solà et al., Reference López-Solà, Fontenelle, Bui, Hopper, Pantelis, Yücel and Harrison2016). However, the shared genetic risk underlying OCD, BDD, and HD may be relatively less important for the risk of SPD and HPD. A community twin study (Monzani et al., Reference Monzani, Rijsdijk, Harris and Mataix-Cols2014) showed that two heritable risk factors underlay the five OCRDs. One factor reflected risk for OCD, BDD, and HD, and to lesser degree SPD and HPD. The other factor conferred risk to SPD and HPD exclusively. Moreover, the genetic variance captured by this factor was entirely shared between HPD and SPD suggesting the possibility that the two disorders may be different phenotypic expressions of the same underlying condition (Monzani et al., Reference Monzani, Rijsdijk, Harris and Mataix-Cols2014). Studies have also identified risk genes that may be preferentially related to BFRBs, and possibly less to other OCRDs. In a mouse model, deletion of the SAPAP3 gene causes a phenotype characterized by anxiety-like behaviors and excessive grooming resulting in hair loss and skin lesions (Welch et al., Reference Welch, Lu, Rodriguiz, Trotta, Peca, Ding, Feliciano and Dudek2007). Human association studies have shown that variants of this gene may be linked to HPD and SPD as well as to OCD (Bienvenu et al., Reference Bienvenu, Wang, Shugart, Welch, Grados, Fyer and Nestadt2009; Boardman et al., Reference Boardman, van der Mewre, Lochner, Kinnear, Seedat, Stein and Hemmings2011; Züchner et al., Reference Züchner, Wendland, Ashley-Koch, Collins, Tran-Viet, Quinn and Krishnan2009), although, the largest study to date has shown association with pathological hair pulling, skin picking and nail biting, but not OCD (Bienvenu et al., Reference Bienvenu, Wang, Shugart, Welch, Grados, Fyer and Nestadt2009).
Finally, placebo-controlled trials have shown that selective serotonin reuptake inhibitors (SSRIs) may have limited efficacy in the treatment of HPD and SPD (Arbabi et al., Reference Arbabi, Farnia, Balighi, Mohammadi, Nejati-Safa, Golestan and Darvish2008; Bloch et al., Reference Bloch, Landeros-Weisenberger, Dombrowski, Kelmendi, Wegner, Nudel and Coric2007), but SSRIs have repeatedly shown efficacy in the treatment of other OCRDs and are recommended as first line pharmacotherapy for OCD and BDD (e.g. Bloch, McGuire, Landeros-Weisenberger, Leckman, and Pittenger, Reference Bloch, McGuire, Landeros-Weisenberger, Leckman and Pittenger2010; evidence for HD are more limited and mixed; Mataix-Cols et al., Reference Mataix-Cols, Frost, Pertusa, Clark, Saxena, Leckman and Wilhelm2010). In contrast, clinical trials have indicated that glutamatergic (N-acetylcysteine; Grant, Odlaug, & Kim, Reference Grant, Odlaug and Kim2009; Grant et al. Reference Grant, Odlaug, Chamberlain, Redden, Leppink, Odlaug and Kim2016) and dopaminergic (olanzapine; van Ameringen, Mancini, Patterson, Bennett, and Oakman, Reference van Ameringen, Mancini, Patterson, Bennett and Oakman2010) medications can be effective in the treatment of HPD and SPD.
The present study
The aim of the present study was to examine the higher-order structure of OCRDs in a transdiagnostic psychiatric sample. We administered a dimensional measure of the five OCRDs to patients in a partial hospital program. We used confirmatory factor analyses (CFA) to compare competing models derived from the previous literature. Although the OCRD chapter in DSM-5 implies that a single factor may underlay all five OCRDs, the evidence reviewed above suggests that the structure may be best represented in a two-factor model where HPD and SPD form a factor distinct from other OCRDs. We therefore compared a single-factor model with a correlated two-factor model comprised of a BFRB factor (including HPD and SPD) and obsessions-compulsions (OC) factor (including OCD, HD, and BDD). Additionally, because research shows high prevalence of skin picking among individuals with BDD (Grant, Menard, & Phillips, Reference Grant, Menard and Phillips2006), we also tested models where BDD was placed on the BFRB factor, allowed to cross-load on both factors, or formed a distinct factor along with SPD. We then examined a model where OCD and BDD form one factor and HD, SPD, and HPD form another factor. This model was derived from the observation that the compulsive/repetitive behaviors in the three latter disorders are primarily ego-syntonic in nature. Based on previous twin research (Monzani et al., Reference Monzani, Rijsdijk, Harris and Mataix-Cols2014), we hypothesized that a two-factor model with OC factor (OCD, HD, and BDD) and BFRB factor (HPD and SPD) would fit the data well, and significantly better than competing models.
We further hypothesized that the two factors would have divergent associations with internalizing and externalizing symptoms, including MDD symptoms, generalized anxiety disorder (GAD) symptoms, trait neuroticism, and drug/alcohol cravings. Specifically, we were interested in examining to what extent the two factors had unique (non-shared) associations with these symptoms. OCD, BDD, and HD are often construed as a form of internalizing psychopathology, and these disorders have been shown to have genotypic and phenotypic correlations with internalizing symptoms (e.g. Kotov, Gamez, Schmidt, & Watson, Reference Kotov, Gamez, Schmidt and Watson2010; López-Solà et al. Reference López-Solà, Fontenelle, Bui, Hopper, Pantelis, Yücel and Harrison2016). We therefore expected that the OC factor would have robust moderately strong associations with indicators of the internalizing spectrum, but no association with drug/alcohol cravings.
In contrast, HPD and SPD appear quite distinct from internalizing disorders with respect to symptom presentation (e.g. pleasure and gratification) and response to pharmacotherapy (e.g. limited response to SSRIs). Thus, we expected that the BFRB factor would have more limited unique associations with internalizing symptoms. Additionally, given the conceptualization of HPD and SPD as reward-driven habits akin to behavioral addictions and impulse control disorders (APA, 2000; Grant et al., Reference Grant, Odlaug and Potenza2007; Odlaug & Grant, Reference Odlaug and Grant2010), we examined whether the BFRB factor would have a unique association with drug/alcohol cravings.
Method
Participants
Participants were adult patients receiving treatment in the Behavioral Health Partial (BHP) hospital program at McLean Hospital in Belmont, Massachusetts. The BHP is not a specialty clinic for OCRDs. However, most patients who attend the program are diagnosed with internalizing disorders, including major depressive episode (61%), GAD (46%), social anxiety disorder (34%) panic disorder (19%), post-traumatic stress disorder (13%), OCD (19%), and BDD (8%) (these figures are based on a previous cohort; see Snorrason, Beard, Christensen, Bjornsson, and Björgvinsson, Reference Snorrason, Beard, Christensen, Bjornsson and Björgvinsson2019). The program provides intensive short-term (1–3 weeks) treatment aimed at stabilizing acute symptoms. About one-half of the patient population is referred from inpatient hospitalization and the other half from the community/outpatient providers. Patients attend the program every weekday (from 9 AM to 3 PM) and receive group and individual psychotherapy, typically along with pharmacotherapy.
The current sample included patients consecutively admitted over 11 months (30 November 2018–16 October 2019). There were 561 admissions to the program during this period. Seventeen individuals admitted more than once and only data from the first admission were included. Twenty-nine patients (5.2%) did not complete the study measures due to logistic or clinical reasons (n = 25) or were judged to have given unreliable responses by the clinic staff (n = 4). The study sample included 532 individuals, thereof, 283 (53.2%) identified as female, 239 (44.9%) as male, and 10 (1.9%) as transgender or nonbinary. The average age was 34 years (s.d. = 14.2, range 18–72 years). Most participants identified as White/Caucasian (n = 454; 88%). Other racial categories endorsed were Asian (n = 27; 5.2%), Black/African-American (n = 14; 2.7%), multi-racial (n = 16; 3%), other (n = 9; 1.7%), and not known (n = 5; 1%). The majority identified a non-Hispanic/Latinx ethnic origin (n = 493, 93.4%).
Measures
Obsessive-compulsive and related disorders symptoms
To assess symptoms of OCRDs we administered the Obsessive-Compulsive and Related Disorders-Dimensional Scales (OCRD-DS; LeBeau et al., Reference LeBeau, Mischel, Simpson, Mataix-Cols, Phillips, Stein and Craske2013). The OCRD-DS is a self-report questionnaire that includes five modules designed to provide dimensional measures of the five OCRDs in DSM-5: OCD, BDD, HD, HPD, and SPD. The modules were created by the DSM-5 OCRD workgroup (LeBeau et al., Reference LeBeau, Mischel, Simpson, Mataix-Cols, Phillips, Stein and Craske2013) and are modeled after the Florida OCD inventory develop by Storch et al. (Reference Storch, Bagner, Merlo, Shapira, Geffken, Murphy and Goodman2007). For each module, responders read a brief description of the relevant condition (e.g. OCD, BDD, etc.) before answering five questions about the symptoms of the disorder in the past week: (1) time occupied by symptoms, (2) distress due to symptoms, (3) control over symptoms, (4) avoidance due to symptoms, and (5) functional impairment. Each item is rated on a 5-point scale ranging from 0 (e.g. none) to 4 (e.g. extreme). Thus, higher score indicates greater severity (possible range = 0–20). Previous studies have shown that the scales have good psychometric properties (Carey, del Pozo de Bolger, & Wootton, Reference Carey, del Pozo de Bolger and Wootton2019; Cheyne, del Pozo de Bolger, & Wootton, Reference Cheyne, del Pozo de Bolger and Wootton2018; LeBeau et al., Reference LeBeau, Mischel, Simpson, Mataix-Cols, Phillips, Stein and Craske2013; Moreno-Amador, Piqueras, Rodriguez-Jimenez, Marzo, & Mataix-Cols, Reference Moreno-Amador, Piqueras, Rodriguez-Jimenez, Marzo and Mataix-Cols2018; Storch et al., Reference Storch, Bagner, Merlo, Shapira, Geffken, Murphy and Goodman2007).
We made minor changes to the scales. In the HPD and SPD modules, when asking about hair pulling or skin picking behaviors, we added the caveat ‘out of habit, not with the purpose of harming yourself’. This was done to avoid assessing skin picking or hair pulling that occurs in the context of non-suicidal self-injury (APA, 2013). In the BDD module, we deleted ‘skin picking’ from examples of repetitive behaviors to minimize artificial overlap between BDD and SPD. Finally, in the OCD module, we provided examples of typical OCD symptoms (e.g. fear of contamination and checking compulsions) to avoid assessing repetitive thoughts and behaviors related to other conditions (e.g. worry or depressive rumination).
Major depressive disorder symptoms
The 9-item Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, and Williams, Reference Kroenke, Spitzer and Williams2001) was used to assess symptoms of MDD. The nine items describe depressive symptoms in the past 2 weeks. Responders rate each item on a 4-point scale (not at all, several days, more than half the days, and nearly every day). Possible score ranges from 0 to 27 and higher score indicates greater severity. The PHQ-9 has been shown to have good psychometric properties among patients admitted to the partial hospital (Beard, Hsu, Rifkin, Busch, & Björgvinsson, Reference Beard, Hsu, Rifkin, Busch and Björgvinsson2016).
Generalized anxiety disorder symptoms
Symptoms of GAD were assessed with the 7-item Generalized Anxiety Disorder scale (GAD-7; Spitzer, Kroenke, Williams, and Lowe, Reference Spitzer, Kroenke, Williams and Lowe2006). The items refer to anxiety and worry in the past two weeks and are rated on 4-point scale (0 = not at all to 3 = nearly every day). Total score can range from 0 to 21 and higher score indicates greater severity. A previous work in the partial hospital has shown that the GAD-7 has good psychometric properties (Beard & Björgvinsson, Reference Beard and Björgvinsson2014).
Neuroticism
We used the 12-item neuroticism scale from the NEO-Five Factor Inventory-3, a widely used self-report measure that has been shown to have good psychometric properties (Costa & McCrae, Reference Costa and McCrae1992). Each item is rated on a 5-point scale ranging from 0 (strongly disagree) to 4 (strongly agree). Four items are reversed score. Higher scores indicate greater levels of neuroticism. The internal consistency of this measure in the current sample was high (α = 0.88).
Drug and alcohol craving
Drug/alcohol cravings were assessed with a modified 3-item Alcohol and Drugs Craving Scale (adapted from the Cocaine Craving Scale; Weiss et al., Reference Weiss, Griffin, Mazurick, Berkman, Gastfriend, Frank, Barber and Moras2003). The items are rated on a 0–10 scale with anchors on each end (e.g. 0: not at all to 10: extremely) and refer to cravings for drugs or alcohol presently and over the past week. A composite craving score is obtained by calculating the average rating on the three items. Thus, possible score ranges from 0 to 10 and higher score indicates more craving. The internal consistency of the items in the current sample was acceptable (α = 0.80).
Data analysis
CFA and structural equation models (SEM) were conducted in the lavaan package (Rosseel, Reference Rosseel2012) in R, version 3.5.2 (R Core Team, 2013). We used maximum likelihood estimator with robust standard errors. We examined six measurement models based on the literature. Model 1 included a single factor manifested by all five OCRDs. Model 2 included two correlated factors: an OC factor with OCD, BDD, and HD and a BFRB factor with HPD and SPD. Model 3 was a version of this two-factor model where BDD was placed on the BFRB factor, and model 4 a version where BDD was allowed to cross-load on both factors. In model 5, BDD and SPD were placed on a separate factor from the other OCRDs (OCD, HD, and HPD) and in model 6 OCD and BDD represented one factor and HD, HPD, and SPD another factor. Based on suggested guidelines (Hu & Bentler, Reference Hu and Bentler1999; Marsh, Hau, & Wen, Reference Marsh, Hau and Wen2004), model fit was judged to be adequate if the root mean square of approximation and the standardized root mean square residual was 0.08 or lower and comparative fit index and Tucker–Lewis index was 0.90 or higher. To compare models, we used the sample-size adjusted Bayesian information criterion where lower value indicates better fitting model. Once measurement models had been established, we conducted SEMs where the latent factors from the best fitting model(s) were used to predict internalizing and externalizing symptoms (i.e. MDD symptoms, GAD symptoms, trait neuroticism, and drug/alcohol cravings). In all models, the variance of the latent factor(s) was fixed to 1. The sample was sufficiently powered to conduct the CFAs/SEMs described herein (Wolf, Harrington, Clark, & Miller, Reference Wolf, Harrington, Clark and Miller2013). The data and the lavaan code can be found on www.osf.io/yjng4/.
Procedures
Participants completed the study questionnaires as part of a routine clinical evaluation on the first and second day in the program; the OCRD scales were administered on the second day, and other measures were administered on the first day.Footnote †Footnote 1 The study was approved as an exempt protocol (using an existing de-identified dataset) by the hospital's IRB. The hypotheses were based on the prior literature, but the study was not formally preregistered.
Results
Average scores and zero order correlations
Table 1 shows the average scores of the study measures and the correlations between them. The average scores on the OCRD scales indicated that symptoms of OCD and BDD were substantially more common than the other OCRDs. (HPD was the least commonly endorsed symptoms in the sample; nevertheless, 23% reported at least some HPD symptoms.) The OCD, HD, and BDD scales all had moderate correlations with each other. The SPD and HPD scales also had a moderately strong intercorrelation, but a small correlation with the other OCRDs, except the SPD scale had moderately strong correlation with the BDD scale.
Table 1. Average scores and Spearman's rho correlations between the OCRD dimensional scales and other study measures
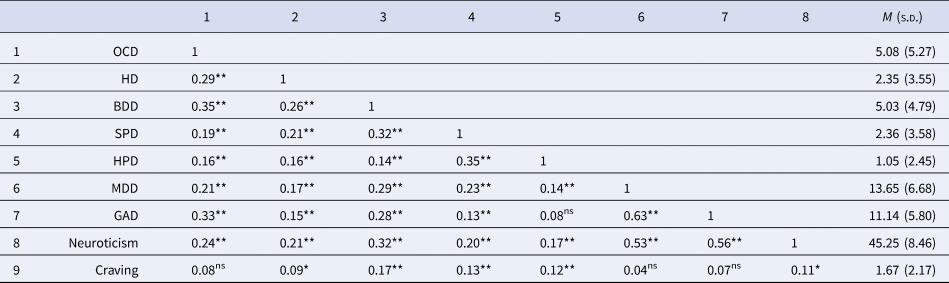
OCD, obsessive-compulsive disorder symptoms; BDD, body dysmorphic disorder symptoms; HD, hoarding disorder symptoms; HPD, hair-pulling disorder (trichotillomania) symptoms; SPD, skin-picking (excoriation) disorder symptoms; MDD, major depressive disorder symptoms; GAD, generalized anxiety disorder symptoms; craving, drug/alcohol craving; ns, not significant; M, mean; s.d., standard deviation.
*p < 0.05, **p < 0.01.
Measurement models
The CFA fit indices and factor loadings for the six measurement models are shown in Tables 2 and 3, respectively. Model 1, where all the OCRDs loaded on the same factor, provided poor fit to the data. In contrast, model 2, which included a separate OC (OCD, HD, and BDD) and BFRB (HPD and SPD) factors, provided good fit according to all fit indices. A version of this model where BDD symptoms were allowed to cross-load on both factors (model 4) also fits well; however, this model was not viable because the BDD symptoms did not load significantly on the BFRB factor. The other models tested did not fit the data well (models 3, 5, and 6). Thus, model 2 was clearly favored over other models. In this model, the OC and BFRB factors were highly correlated and all indicators had at least moderately strong loadings (>0.40) on their respective latent factor, suggesting that the factors are well represented by the manifest symptom variables (see Fig. 1).

Fig. 1. Path diagram of the best-fitting CFA model. OC, obsessions-compulsions latent factor; BFRB, body-focused repetitive behaviors latent factor; OCD, obsessive-compulsive disorder symptoms; HD, hoarding disorder symptoms; BDD, body dysmorphic disorder symptoms; SPD, skin-picking (excoriation) disorder symptoms; HPD, hair-pulling disorder (trichotillomania) symptoms. All parameter estimates are standardized and significant at p < 0.01.
Table 2. Model fit statistics

df, degrees of freedom; SRMSR, standardized root mean square residual; RMSEA, root mean square of approximation; CFI, comparative fit index; TLI, Tucker–Lewis index; BIC, sample-size adjusted Bayesian information criterion.
Table 3. Standardized factor loadings

f1, factor 1; f2, factor 2; OCD, obsessive-compulsive disorder symptoms; BDD, body dysmorphic disorder symptoms; HD, hoarding disorder symptoms; HPD, hair-pulling disorder (trichotillomania) symptoms; SPD, skin-picking (excoriation) disorder symptoms; MDD, major depressive disorder symptoms; GAD, generalized anxiety disorder symptoms.
Correlations between latent factors were as follows: model 2 = 0.66, model 3 = 0.87, model 4 = 0.59, model 5 = 1.00, and model 6 = 0.75. Unless otherwise noted, all loadings are significant at p < 0.001.
a p = 0.322.
Structural regression models
The results from the structural regression models are summarized in Table 4. The OC factor, but not the BFRB, had significant unique associations with all three internalizing symptoms (MDD symptoms, GAD symptoms, and neuroticism), and in all cases the associations were positive and moderately strong. The BFRB factor, but not the OC factor, had a small marginally significant positive association with drug/alcohol craving.
Table 4. Structural regression coefficients

MDD, major depressive disorder; GAD, generalized anxiety disorder; OC, obsessions-compulsions factor; BFRB, body-focused repetitive behaviors factor.
Discussion
The concept of OC spectrum disorders has received considerable attention in the nosological literature (Phillips et al., Reference Phillips, Stein, Rauch, Hollander, Fallon, Barsky and Leckman2010) and both DSM-5 and upcoming ICD-11 now include a distinct OCRD chapter. However, empirical research on the structure of OCRDs has been scarce. In the current study, we examined the higher-order structure of OCRD symptoms in a clinically severe psychiatric sample. The results indicated that the OCRDs in DSM-5 are best represented by two correlated higher-order factors that have divergent associations with symptoms across the internalizing and externalizing spectra. The OC factor accounted for the covariance of OCD, BDD, and HD, and had robust associations with internalizing symptoms. The BFRB factor accounted for the covariance of HPD and SPD, but had no unique associations with internalizing symptoms, and a small marginally significant association with drug/alcohol cravings.
The structure of OCRDs
The current study was the first to examine the higher-order structure of OCRDs in a transdiagnostic clinical population. We tested six plausible models based on the prior literature. The results showed that the OC v. BFRB factor model was the only viable model tested. These findings are consistent with results from non-clinical samples showing greater phenotypic associations between HPD and SPD v. other OCRDs (Maraz, Hende, Urbàn, & Demetrovics, Reference Maraz, Hende, Urbàn and Demetrovics2017; Monzani et al., Reference Monzani, Rijsdijk, Harris and Mataix-Cols2014, supplementary material; Watson et al., Reference Watson, Stasik-O'Brien, Ellickson-Larew and Stanton2018). Our findings are also consistent with twin research that have documented a distinct heritable risk factors underlying HPD and SPD v. OCD, BDD, and HD (Monzani et al., Reference Monzani, Rijsdijk, Harris and Mataix-Cols2014). Thus, there appears to be a convergence between the phenotypic and genotypic structure of OCRD symptoms. A similar convergence has been documented in other dimensions of psychopathology, including internalizing disorders (Waszczuk et al., Reference Waszczuk, Eaton, Krueger, Shackman, Waldman, Zald and Kotov2020).
Associations with internalizing and externalizing symptoms
As expected, the OC factor had robust moderately strong associations with internalizing symptoms (standardized estimates = 0.42–0.66), which is consistent with previous studies showing that OCD, BDD, and HD have genetic and phenotypic associations with internalizing symptomatology (e.g. López-Solà et al., Reference López-Solà, Fontenelle, Bui, Hopper, Pantelis, Yücel and Harrison2016). In contrast, the BFRB factor did not have significant unique associations with any of the internalizing symptoms. Studies have frequently documented comorbid anxiety and depression among those who seek treatment for HPD and SPD and negative affect is often recognized as a maintaining factor in BFRBs. However, clinical comorbidity studies rarely account for base-rates of emotional disorders in treatment seeking populations generally (Christenson, Chernoff-Clementz, & Clementz, Reference Christenson, Chernoff-Clementz and Clementz1992) and studies examining the role of negative affectivity in BFRBs typically do not control for coexisting symptoms or disorders (e.g. OCD). Thus, the nature of the association between BFRBs and internalizing symptomatology remains poorly understood. The current results suggest that there is a limited association between BFRBs and internalizing symptoms, once other OC psychopathology is accounted for.
Interestingly, we did find that the BFRB factor had a small marginally significant association with drug/alcohol cravings. These findings suggest that BFRBs may have some associations with the externalizing spectrum, although further research is clearly needed to explore this possibility. The association between BFRBs and externalizing psychopathology, particularly addictive disorders, has been noted previously in the literature. Several authors have pointed out that symptom features in HPD and SPD resemble addictive disorders (e.g. urges, craving, and gratification), and SPD and HPD have historically been conceptualized as impulse control disorders (APA, 2000) or behavioral addictions (Grant et al., Reference Grant, Odlaug and Potenza2007; Odlaug & Grant, Reference Odlaug and Grant2010). Furthermore, randomized-controlled trials have shown that glutamatergic medications (e.g. N-acetylcysteine), which are known for reducing cravings across psychiatric and addictive disorders (Duailibi et al., Reference Duailibi, Cordeiro, Brietzke, Ribeiro, LaRowe, Berk and Trevizol2017), significantly reduce symptoms of SPD (Grant et al., Reference Grant, Odlaug, Chamberlain, Redden, Leppink, Odlaug and Kim2016) and HPD (Grant et al., Reference Grant, Odlaug and Kim2009). Additionally, an early study (Schlosser, Black, Blum, & Goldstein, Reference Schlosser, Black, Blum and Goldstein1995) found that first-degree family members of individuals with HPD were more likely to have substance use disorders (21.6% alcohol use disorder and 14.7% drug use disorders) than first-degree family members of healthy comparison subjects (7.7% alcohol use disorder and 2.2% drug use disorders). Further research is therefore warranted to examine to what extent BFRBs share liability with addictive disorders and externalizing psychopathology more broadly (Gerstenblith et al., Reference Gerstenblith, Jaramillo-Huff, Ruutiainen, Nestadt, Samuels, Grados and Rasmussen2019).
Implication for HiTOP
In the HiTOP model, OCD is placed on the fear subfactor under the internalizing spectrum, but other OCRDs have not yet been included in the model (Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby and Zimmerman2017). Our results suggest that OCD as well as BDD may belong to the internalizing spectrum, although their exact location on inter-mediate levels remains to be determined (e.g. under a fear subfactor v. a distinct OC subfactor). Our findings have less to say about the placement of HD because the OCRD-DS measure does not adequately distinguish between OCD-related hoarding (e.g. hoarding related to obsessive fear of harm) and HD proper (discussed below). Also, more research is needed to examine the placement of BFRBs within the HiTOP model. Although the OC and BFRB factors were highly correlated, the overall pattern of results suggested that the placement of BFRBs within the internalizing spectrum may not be straightforward.
Limitations and future directions
The main limitation of the study was the use of self-report scales to assess the OCRDs. The OCRD-DS scales provide dimensional assessment of the symptoms, which is consistent with substantial literature supporting dimensional nature of OC psychopathology (e.g. Timpano et al., Reference Timpano, Broman-Fulks, Glaesmer, Exner, Rief, Olatunji and Schmidt2012) and the scales have been shown to have acceptable psychometric properties (e.g. LeBeau et al., Reference LeBeau, Mischel, Simpson, Mataix-Cols, Phillips, Stein and Craske2013; Storch et al., Reference Storch, Bagner, Merlo, Shapira, Geffken, Murphy and Goodman2007). Nonetheless, a replication of the study using comprehensive assessment of symptoms with clinical interviews is needed.
The study is also limited because the OCRD-DS assesses OCRDs at the disorder level, without capturing more narrowly defined symptoms. For example, OCD symptom dimensions are not assessed separately (e.g. checking, washing, etc.), and these dimensions may relate to other OCRDs or internalizing/externalizing symptoms in different ways. In fact, evidence suggests that the strength of the genetic correlation between neuroticism and OCD varies across OC symptom dimensions (Bergin et al., Reference Bergin, Verhulst, Aggen, Neale, Kendler, Bienvenu and Hettema2014). Relatedly, as mentioned above, the HD scale simply assesses problematic hoarding behaviors (e.g. distress and impairment due to hoarding) but does not distinguish between HD and hoarding due to obsessions in OCD. Research show that OCD-related hoarding can be quite distinct from pure HD (Pertusa, Frost, & Mataix-Cols, Reference Pertusa, Frost and Mataix-Cols2010), and may have different relationships with internalizing symptoms, OC symptoms, and other OCRDs (Mataix-Cols et al., Reference Mataix-Cols, Frost, Pertusa, Clark, Saxena, Leckman and Wilhelm2010). Also, the SPD scale does not assess whether skin picking is due to appearance concerns in BDD. Individuals with BDD often engage in skin picking to improve appearance (Grant et al., Reference Grant, Menard and Phillips2006), however, the prevalence of BDD is not substantially elevated among individuals with SPD (Grant, Odlaug, & Kim, Reference Grant, Odlaug and Kim2010). Thus, skin picking in SPD may be quite different from BDD-related skin picking (Snorrason, Stein, & Woods, Reference Snorrason, Stein and Woods2013). Given that we did not distinguish between pure SPD and BDD-related skin picking the correlation found between symptoms of SPD and BDD may have been artificially high. Future studies should empirically determine the structure of OCRDs from the bottom-up using comprehensive and fine-grained assessment of symptom features.
Similarly, given a relatively small number of indicators per factor, and relatively low base-rates of some OCRDs (e.g. HPD), future researchers may want to replicate the study in a larger sample where each OCRD is assessed with multiple indicators (Wolf et al., Reference Wolf, Harrington, Clark and Miller2013). Finally, because we made several changes to the OCRD scales to better assess the disorder constructs (e.g. rule out non-suicidal self-injury in the SPD/HPD modules), it is not clear how well the results generalize to previous literature using the instrument.
Conclusion
The present findings suggest that OCD, BDD, and broadly defined HD may be a manifestation of a shared underlying liability that is associated with internalizing symptoms, whereas, HPD and SPD share a common liability that appears relatively unrelated to internalizing symptoms. Future studies are needed to further explore the nature of these liabilities, their genetic underpinnings, and placement within the meta-structure of psychopathology.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors. Andrew D. Peckham was supported by NIMH grant F32 MH115530 during completion of this work.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.








