Functional neurological disorder (FND) is a complex illness of unclear etiology in which neurological symptoms fail to conform to normal diagnostic processes leading to bias and skepticism often associated with feigning.Reference Ejareh Dar and Kanaan1 Despite levels of disability that compare to other neurological disorders, FND often lacks clear treatment and care pathways, and stigma may be both a cause and consequence of the fractured clinical and research landscapes for the disorder. While stigma against patients with FND has a long history and can originate from multiple sources,Reference Rommelfanger, Factor, LaRoche, Rosen, Young and Rapaport2 the focus of this paper is on the clinical encounter—specifically, the stigmatizing attitudes and stereotypes that can be conveyed during interactions between patients with FND and their healthcare providers (HCPs).
Presenting with symptoms that fall between the traditional boundaries of neurology and psychiatry, patients with FND often encounter frustration and skepticism in the healthcare system and patients report that the experience can be devastating.3, Reference Martiros and Myers4 The time from initial symptom onset to accurate diagnosis of an FND can take years.Reference Duncan, Razvi and Mulhern5 Once a diagnosis is made, the label of FND on a patient’s medical record carries with it the potential to be stereotyped and treated differently as a result.Reference Fernholm, Holzmann, Wachtler, Szulkin, Carlsson and Pukk6, Reference Rommelfanger7 Prominent FND researchers have noted that how such a diagnosis is conveyed, and the biases that can be betrayed by an especially awkward delivery to patients—in contrast to a typical delivery of a diagnosis of a brain disorder such as epilepsy—, and can undermine patient care and recovery.Reference Monzoni, Duncan, Grunewald and Reuber8, Reference Stone, Carson and Hallett9
Stigma, broadly understood, is the social alienation experienced as a result of different or discriminatory treatment.Reference Rao, Choi and Victorson10 Considerable research has addressed stigma in the context of mental illness, however, there are critical differences in the experience of patients with FND and mental illness, and very little research has investigated stigma in the unique context of FND. That said, there is some preliminary evidence that highlights the scope of the problem. Twenty-nine percent of professionals responding to a recent 2020 survey from the Movement Disorder Society reported disliking seeing FND patients.Reference LaFaver, Lang and Stone11, Reference Gilmour, Nielsen and Teodoro12 Discriminatory behavior from providers can range from taking a defensive stance while communicating with patientsReference Monzoni, Duncan, Grunewald and Reuber8, Reference Monzoni, Duncan, Grunewald and Reuber13 to making jokes and negative comments about FND patients on social media.Reference Tolchin, Baslet and Dworetzky14 Despite the growing scientific and medical literature on FND, the attitudes of physicians are slower to evolve.Reference Burke15, Reference Myers, Jones, Boesten and Lancman16 Patients with FND directly experience the consequences of these negative attitudes: in a survey conducted by an FND advocacy organization (FND Hope), 85% of patients reported feeling disbelieved and disrespected when visiting a medical professional (https://fndhope.org/fnd-hope-research/).
We suspect stigma against FND has also impacted research priorities. Lack of research can propagate stigma, and negative attitudes and indifference toward these disorders may limit research funding and translation of findings into medical practice. FND remains poorly understood and receives almost no federal research funds (a search for NIH-funded grants with “functional neurological disorder” in the abstract yields 1 result, compared to over 800 results for “epilepsy”). Even the prevalence of FND lacks consensus depending on the study population. Some studies indicate that FND is uncommon, affecting an estimated 6% to 15% of the population,Reference Carson and Lehn17 while other sources argue that FND is the second most common reason for a neurological visit.Reference Stone, Carson and Duncan18 Research efforts to unify diagnostic criteria, evaluate treatments, and identify biomarkers (described by the accompanying articles in this special issue) could reduce aspects of FND stigma by minimizing uncertainty and providing clear pathways for care. However, biomedical research alone is unlikely to eliminate stigma. In this paper, we propose a stand-alone research agenda specifically focused on reducing stigma in FND that could transform significant aspects of the clinical encounter. Our hope is that the agenda will be taken up broadly by all stakeholders who show do research in the clinical context and we seek for brain health funding leaders at the federal level (eg National Institutes of Health) and philanthropic research funders (eg Wellcome Trust). We believe that addressing stigma will advance care and improve outcomes for many patients.
The Experience and Context of Stigma in FND
We believe stigma for FND is real, creates suffering for patients and diminishes already limited offerings in many healthcare contexts. However, a critical initial step in a research agenda focused on stigma in FND is understanding, documenting, and articulating the experience and prevalence of stigma and the contexts in which it occurs. Patients with functional symptoms enter healthcare systems via diverse care settings, and may interact with a variety of “frontline” HCPs (including emergency medical personnel, primary care physicians, and nurses) and especially specialists (such as neurologists, mental health clinicians, and movement disorder specialists). The attitudes and beliefs that HCPs hold about FND are often conveyed to patients through these clinical encounters, and can be perceived as invalidating or stigmatizing, leading to a demoralizing sense of helplessness (Figure 1).
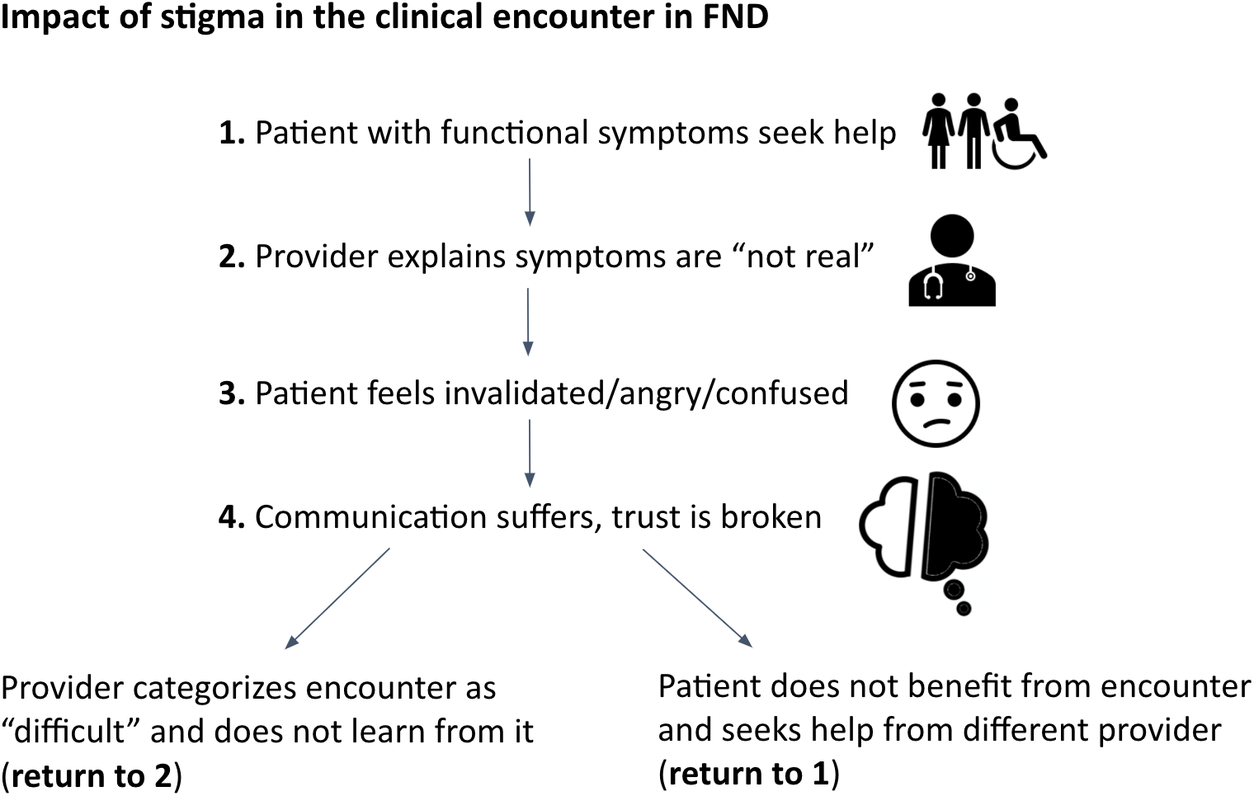
Figure 1. This is a simplified depiction of one potential way that stigma can impact the clinical encounter in FND. Stigma can result in a repeated cycle of negative patient–provider interactions that can (a) cause iatrogenic harm to the patient, (b) fail to improve medical practice, and (c) result in unnecessary use of healthcare resources and delays in receiving treatment.
In a survey conducted by FND Hope, patients reported stigmatizing interactions with a range of HCPs, with interactions with neurologists most likely to be stigmatizing (Figure 2). Another survey asked 135 patients with functional seizures to describe their single worst healthcare interaction; clinical encounters were described as “shocking,” “offensive,” and “disgraceful,” often noting clinicians’ lack of knowledge and understanding of the disorder.Reference Robson and Lian19 Similar to Figure 1, the types of HCPs most often identified as being involved in these negative interactions included neurologists who do not specialize in seizures, emergency medicine physicians, general practitioners, and nursing staff.
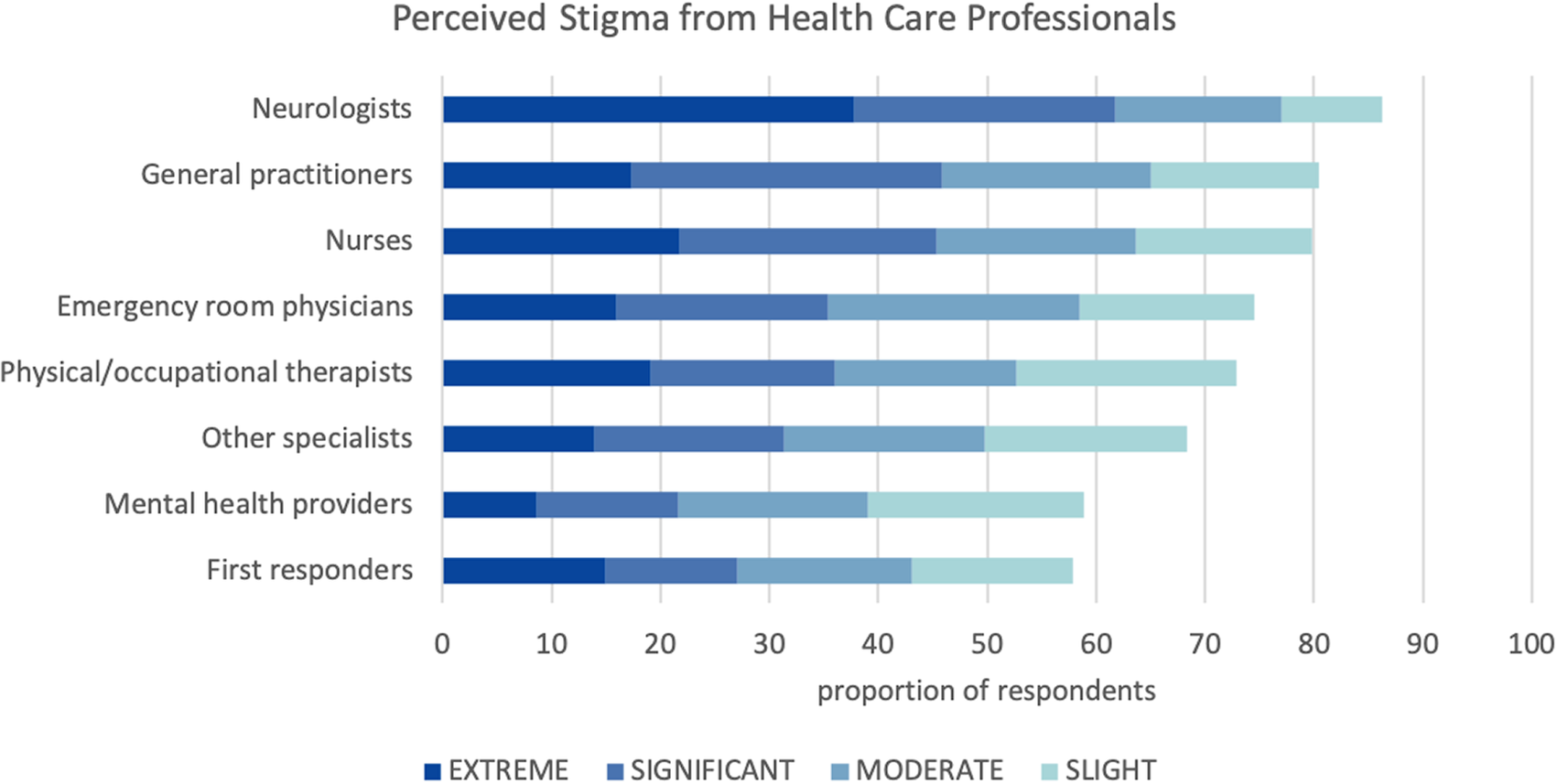
Figure 2. Data from a survey conducted by the FND advocacy association, FND Hope. Respondents were asked to rate the extent to which they have felt discrimination/stigma from members of these groups of health care professionals. Interactions with neurologists were perceived as stigmatizing by the highest proportion of participants. https://fndhope.org/fnd-hope-research/.
Members of the medical community often dismiss symptoms of FNDReference Burke15—which is perceived as highly invalidating for the patient—due to a common misconception that FND symptoms are produced voluntarily.Reference Maurer, LaFaver, Ameli, Epstein, Hallett and Horovitz20 A majority of the existing data on HCP attitudes toward FND focuses on the subset of patients who present with functional seizures.Reference Rawlings and Reuber21 One survey of primary care and emergency medicine physicians revealed that 85% felt the term “pseudoseizure” was appropriate and 38% thought events were voluntary or “fake.”Reference Shneker and Elliott22 A survey of general practitioners found that 35% disagreed with the patient’s diagnosis and 65% did not support psychological intervention.Reference O’Sullivan, Sweeney and McNamara23 Other studies using the Illness Perception Questionnaire and Symptom Attribution Questionnaire found that the majority of neurologists, psychiatrists, and emergency medicine respondents attributed epilepsy to “physical” causes while functional seizures were often attributed to “psychological” causes. Studies interviewing neurologists and psychiatrists on attitudes on FND suggested a strategy of handling medical uncertainty by using psychological explanations and an age old stigma associated with an often oversimplification of the physical and psychologica.Reference Rommelfanger7, Reference Rommelfanger24, Reference Grubbs, Rommelfanger, LSM and Rommelfanger25. In addition, HCPs on these surveys reported that patients with functional seizures had more control over their seizures compared to patients with epilepsy.26-28 Interestingly, patients with either epilepsy or functional seizures responding to the same questionnaires reported a similar combination of physical and psychological causes for their disease, suggesting that patients may accept a more nuanced and complex explanation of their symptoms than do their providers.
The experience of stigma from the patient perspective has also been studied in the context of functional seizures. One qualitative study revealed that while epilepsy patients perceived their HCPs as a knowledgeable source of support and trust, patients with functional seizures identified their HCPs as distrustful, unsupportive, and lacking understanding.Reference Rawlings, Brown, Stone and Reuber29 Measuring perceived stigma revealed that stigma is experienced more often by patients with functional seizures compared to epilepsy. Using a single item from the NEWQOL-6D (a 6-item survey designed to measure health-related quality of life in epilepsy),Reference Rawlings, Brown and Reuber30 87% of patients with functional seizures reported perceived stigma, compared to 45% of patients with epilepsy.
These existing studies suggest a troubling reality for patients with functional seizures and other FND symptoms, but significant gaps remain in our knowledge about the prevalence and origin of stigma in FND. Further research should focus on the measurement of stigmatizing attitudes and biases among different groups of HCPs to identify which providers/disciplines should be prioritized for stigma-reduction interventions. In addition to self-report surveys, studies of provider attitudes should include assessments like the Implicit Association Test (IAT https://implicit.harvard.edu/implicit/takeatest.html), which can reveal biases that may exist beyond conscious awareness. The scope of these studies should also be expanded to include patients with FND who present with symptoms other than functional seizures. Formalized scales such as the Stigma Scale for Chronic IllnessReference Molina, Choi, Cella and Rao31 have been utilized to measure the experience of stigma from the patient perspective in other neurological diseases but have not yet been used in the context of FND. Studies should evaluate whether these currently available assessment tools could be used in this patient population or whether novel measures should be developed. In addition, questions remain regarding the magnitude of stigma in FND and how it compares to other chronic neurological disorders like multiple sclerosis (MS) as well as mental health disorders. Finally, efforts to measure internalized or “self-stigma” could reveal the extent to which stigmatizing attitudes from HCPs and others come to be reflected in how patients conceptualize themselves and their disorders.Reference Rao, Elshafei, Nguyen, Hatzenbuehler, Frey and Go32
The Clinical Impact of FND Stigma
A research agenda focused on stigma requires demonstration of how stigma can be a substantial barrier to effective clinical care, and in turn adversely affect outcomes for patients with FND. A recent paper presenting long-term outcome data for patients with FND revealed that 80% of patients remained symptomatic at follow-up (average 14 years after initial diagnosis) with rates of employment decreasing over time.Reference Gelauff, Carson, Ludwig, Tijssen and Stone33 These data suggest that current approaches for diagnosing and treating FND (and one approach is to simply offer no treatment) have failed to improve life for the majority of patients, and it is possible that stigma may play a role in this failure.Reference Edwards34 Understanding the impact of stigma in FND could have both clinical and economic implications. Addressing stigma-related barriers to medical care could help patients get an accurate diagnosis and effective treatment earlier, thus decreasing patient suffering and the utilization of inappropriate and limited healthcare resources. Measuring the clinical impact of stigma on patients is the focus of this part of the research agenda; however, there may also be important impacts of stigmatizing attitudes on HCPs that warrant further study.
Testimonies from patients with FND reveal stories of interactions with HCPs that minimize the diagnosis (eg “you can control this,” “it’s all in your head”) and invalidate symptoms as “fake” or “not real.”Reference Martiros and Myers4 Yet few systematic investigations have examined the impact of such conveyed stigma on patients’ future treatment-seeking behavior and ultimate health outcomes. One study of patients with functional seizures found that higher perceived stigma was associated with lower health-related quality of life, including subscales measuring seizure worry, emotional wellbeing, and social functioning. Associational studies like this one are important place to start, and should be followed by efforts to associate perceived stigma with objective health outcomes such as FND treatment initiation (eg follow up on referral for outpatient therapy), general healthcare utilization (eg number of repeat emergency room or urgent care visits), and symptom improvement (eg number of seizures). Other relevant outcomes that reflect broader flourishing could include measurement of employment status, relationship satisfaction, and educational achievement. Tracking other physical health outcomes unrelated to FND is also critical as evidence suggests physical symptoms tend to be minimized—with risk of missing important clinical warning signs—for patients with a documented history of psychiatric disorder in their medical record.Reference Fernholm, Holzmann, Wachtler, Szulkin, Carlsson and Pukk6
Existing literature on the impacts of stigma against women and racial/ethnic minorities should also be overlaid with the context of FND. FND is diagnosed twice as often in women than menReference Espay, Aybek and Carson35. Examining intersectional identities in FND could reveal whether patients with certain gender identities, sexual orientations, or racial/ethnic backgrounds experience additional stigma and thus poorer health outcomes. Some evidence from international contexts highlights similar challenges facing FND patients and providers in several countries, suggesting the stigma associated with FND may generalize across culturesReference Fouche, Hartwig and Pretorius36, Reference Korman, Sarudiansky and Lanzillotti37; however, comparative international research could yield important insights on the extent to which broader cultural influences moderate the relationship between stigma and health outcomes in FND. Understanding the extent to which different forms of culturally-based stigma impact the experience of patients with FND could improve the appropriate targeting of stigma-reduction interventions.
Commonly held biases and stereotypes of FND patients also likely impact the behavior of HCPs in important and measurable ways. HCPs who treat patients with undiagnosed diseases often feel unclear as to how to help them and thus may recommend multiple referrals or unwarranted interventions.Reference Rommelfanger24, Reference Anderson, Gruber-Baldini and Vaughan38 This behavior leads to unnecessary utilization of expensive healthcare resources and has the potential to harm patients both physically and psychologically. Negative attitudes may also cause HCPs to underdiagnose FND which prevents those presenting with functional symptoms from accessing appropriate care. HCPs may avoid initiating conversations with patients out of fear that the diagnosis will not be accepted or understood.Reference Monzoni, Duncan, Grunewald and Reuber13 Additional qualitative and observational research can improve our understanding of how stigma contributes to provider reluctance to discuss an FND diagnosis. In addition, HCPs may be internally conflicted when personal values that guide their professional demeanor in other cases (eg treat every patient with empathy) is challenged by colleagues who have inherited historically stigmatizing attitudes toward patients with FND (eg “don’t trust what she says”). The impact of these challenging dynamics on HCPs could be measured through existing measures of job satisfaction, self-efficacy, and moral distress. Finally, structural aspects of the healthcare system—for example, lower reimbursement rates for mental health diagnostic codes compared to a neurological codes—can impact HCP behavior and convey an implicit message that one type of disorder (and thus one type of provider) is more or less valued.Reference Phillips, Benoit, Hallgrimsdottir and Vallance39 Studies focused on measuring the subjective and objective consequences of FND stigma on provider behavior could provide much-needed insight into the complex dynamics of stigmatizing healthcare encounters and inform stigma-reduction interventions.
Interventions to Reduce Stigma in FND
In addition to research measuring the prevalence and clinical impacts of FND stigma, a comprehensive research agenda should ultimately identify and test interventions for reducing stigma in the clinical encounter. Multiple strategies to identify and address health-related stigma have been developed and evaluated for other conditions, particularly those with high levels of medical uncertainty.Reference Nyblade, Stockton and Giger40 In addition, interventions to increase awareness and knowledge of conditions of mental illness and substance use disorders have shown that positive behavior and attitude changes can be leveraged to reduce stigma.Reference Collins, Wong, Cerully, Schultz and Eberhart41 The experience of stigma in FND is likely unique to these disorders; however, adapting strategies from other contexts could provide a useful starting point on the way to developing interventions specific to FND.
Tools for reducing stigma in the clinical encounter could be adapted from those designed to be effective for general audiences.Reference Corrigan, Morris, Michaels, Rafacz and Rüsch42 Presentations and programs delivered by advocates, individuals with lived experience, and clinicians have been shown to increase participant knowledge, inform more positive perceptions, and reduce distress associated with having or caring for something with symptoms.43-45 In the FND community, sites such as nonepilepticseizures.com and neurosymptoms.org provide direct education and support in the form of patient narratives and free downloadable pamphlets for patients and healthcare professionals. Patient advocacy organizations such as FND Hope (fndhope.org) offer a repository of educational resources and host webinars that allow real-time interaction with experienced FND clinicians. While no formal research has yet been conducted on the reach and effectiveness of these resouces-which is what we advocate for—, informal reports from the webmasters suggest that the resources increase knowledge, build confidence during the clinical encounter, offer reassurance and validation, and create a sense of community among healthcare professionals and affected individuals.
Given the high proportion of patients with FND who feel disrespected, demoralized, and stigmatized in interactions with HCPs, stigma-reduction interventions that specifically target medical providers are warranted. Some aspects of stigma may be reduced by simply expanding basic medical curricula to cover FND. A survey of HCPs Australia revealed that only 14% felt that they received adequate FND education as part of their training,Reference Lehn, Bullock-Saxton, Newcombe, Carson and Stone46 and in the recent Movement Disorders Society study, 32% of respondents indicated that a lack of education on FND was a significant treatment barrier.Reference LaFaver, Lang and Stone11 Most training of medical students related to FND occurs through an informal, “hidden curriculum”Reference Rommelfanger24, Reference Montegomery and Berger47 as can be the case with other poorly understood disorders.Reference Silverwood, Chew-Graham, Raybould, Thomas and Peters48 Instead, intentional and structured efforts to convey an understanding of the uncertainty and complexity of FND may be required to reduce stigma amongst HCPs.Reference Rommelfanger, Factor, LaRoche, Rosen, Young and Rapaport2, Reference Klinke, Hjartardottir, Hauksdottir, Jonsdottir, Hjaltason and Andresdottir49 However, no formal studies have yet been conducted to assess the efficacy of stigma reduction in these models.
Promising interventions targeting mental illness stigma could be adapted for HCPs working with patients with FND.Reference Rao, Elshafei, Nguyen, Hatzenbuehler, Frey and Go32, Reference Gronholm, Henderson, Deb and Thornicroft45, Reference Mehta, Clement and Marcus50, Reference Thornicroft, Mehta and Clement51 For example, participation in the National Alliance on Mental Illness (NAMI) Provider program—a 15-hour in-service training led by a mental health clinician, an individual with a mental health diagnosis, and a patient family member—was associated with significant improvements in medical student affect, attitudes, and behavioral intentions toward caring for psychiatric patients, with continued effects 3 months post-intervention. Similar programs specifically focused on FND should be developed and tested for efficacy with trainees as well as mid-career HCPs. Such programs could incorporate strategies shown to be effective for reducing stereotypes toward racial/ethnic minority groupsReference Corrigan and Penn52, Reference Penn and Corrigan53 and should measure outcomes both immediately and long term to demonstrate which approaches are capable of achieving meaningful and enduring change.
We see an opportunity in FND to fill the vacuum left by sorely inadequate coverage in medical education with educational interventions designed to address the multifaceted nature of stigma and improve health outcomes for patients.Reference Rao, Elshafei, Nguyen, Hatzenbuehler, Frey and Go32 One strong indicator of momentum in this direction is the recent formation of the FND Society—a professional organization for members of the healthcare community with a shared interest in improved patient care and research in FND, which aims to hold its first conference in 2022. The time is ripe for advancing research to understand and directly address the harmful impacts of stigma on the lives of patients with FND.
Conclusion
In this paper, we set a research agenda (Table 1) for addressing FND-related stigma in the clinical encounter.
Table 1. Research Agenda for Addressing Stigma in the FND Clinical Encounter
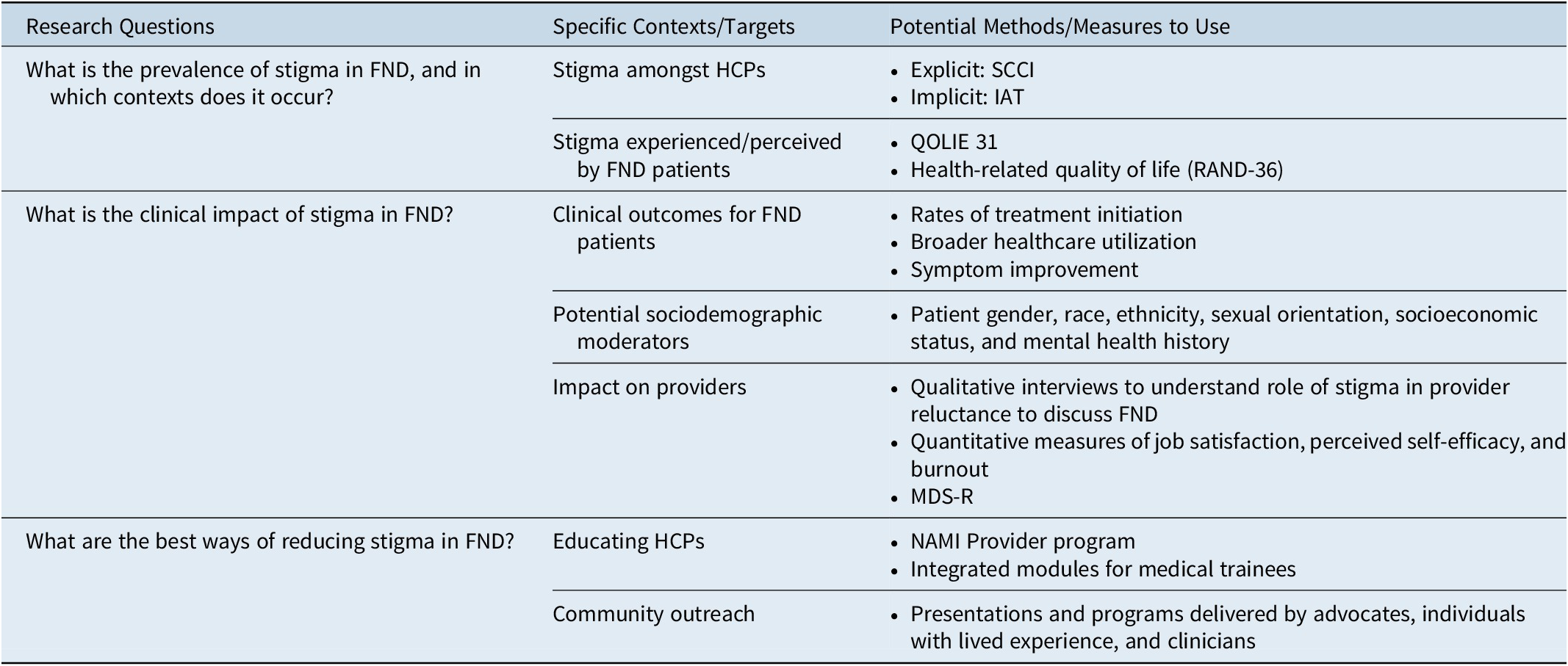
Abbreviations: FND¸ functional neurological disorder; HCP, healthcare providers; IAT, implicit association test; MDS-R, Moral Distress Scale-Revised; QOLIE 31, quality of life in epilepsy; SCCI, stigma scale for chronic illness.
We believe the long history of stigma against FND continues to exert a powerful influence in clinical interactions, despite scientific evidence that has advanced our understanding of the disorder. Positive, non-stigmatizing interactions between clinicians and patients represent a powerful opportunity for the earliest intervention, to establish a therapeutic alliance and support better clinical encounters and outcomes. We believe stigma also influences broader research agendas: conditions that lack a robust community voice are rarely selected for deeper exploration. Addressing stigma in these conditions may encourage funding opportunities for mechanistic, diagnostic, and treatment research. We suggested a series of approaches and existing methods that could be adapted to understand the prevalence and clinical impact of stigma in FND, as well as the efficacy of anti-stigma interventions. Interventions for HCPs that reduce FND stereotypes and biases could help them care more effectively for this patient population, while also introducing new ways to deal with diagnostic uncertainty and gaps in knowledge that are inherent in medical practice more broadly.
Funding Information
Funding for this manuscript was provided by The Mark and Barbara Klein Mind–Body Conference Series, hosted by Emory University.
Disclosures
The conference was paid for by the Mark and Barbara Klein Conference series, hosted by Emory University. Kate MacDuffie, Lindsey Grubbs, Suzette LaRoche, Bridget Mildon, Lorna Myers, and Elizabeth Stafford received travel and lodging from the Mark and Barbara Klein Mind–Body Conference Series meeting, sponsored by Emory University. Karen S. Rommelfanger received funding to host and organize the Mark and Barbara Klein Mind–Body Conference Series meeting from the Department of Psychiatry and Behavioral Neurosciences at Emory University, and she is also a salaried employee of Emory University. Tammyjo Best has nothing to disclose.





