Introduction
Lifestyle choices affect the risk of developing a major non-communicable disease and health status in general (Jang et al., Reference Jang, Choi and Kim2009; Tubeuf et al., Reference Tubeuf, Jusot and Bricard2012; Murray et al., Reference Murray, King, Sorensen, Bunick and King2018). Smoking, physical inactivity, unhealthy diet, obesity and other lifestyle behaviours are associated with the development of diseases such as cancer, heart disease, stroke and diabetes (Roos et al., Reference Roos, Lahti and Rahkonen2018). The societal and monetary costs of the negative effects of these modifiable behaviours are significant (Scarborough et al., Reference Scarborough, Bhatnagar, Wickramasinghe, Allender, Foster and Rayner2011; von Humboldt et al., Reference von Humboldt, Leal and Pimenta2014; Okulicz-Kozaryn & Valente Reference Okulicz-Kozaryn and Valente2019) and increase with age. Previous studies have investigated the effects of single lifestyle behaviours on health (Doll et al., Reference Doll, Peto, Boreham and Sutherland2000; Laditka & Laditka, Reference Laditka and Laditka2001; Hung et al., Reference Hung, Joshipura and Jiang2004; Adams et al., Reference Adams, Schatzkin and Harris2006; Warburton et al., Reference Warburton, Nicol and Bredin2006), but a combined and conditioned probability approach may yield a more accurate picture. The investigation of predictive factors should consider several variables, including health factors (such as chronic health conditions) as well as lifestyle.
Governments and other regional health policy agencies can influence healthy lifestyles, for instance by offering economic and other incentives to encourage certain behaviours (McPake & Hanson, Reference McPake and Hanson2016). However, the use of tax money for such purposes should be justified and prioritized on a cost-benefit basis.
Of particular interest is the economic burden of different diseases, specifically two: heart attack (myocardial infarction) and stroke (cerebrovascular accident). These adverse cardiovascular events are the two highest causes of death in Europe (Donnan et al., Reference Donnan, Fisher, Macleod and Davis2008). Luengo-Fernandez et al. (Reference Luengo-Fernandez, Violato, Candio and Leal2020) argued that in 2017 stroke cost the 32 European countries about 60 billion Euros (about 60 Euros per person). Pavlušová et al. (Reference Pavlušová, Klimes, Špinar, Zeman, Jarkovský and Benešová2018) estimated that the prevalence of stroke-afflicted patients in the global adult population is 4%, reaching 10% for adults aged 70 years and older. The overall societal cost is thus expected to increase because the population in that age bracket is expected to increase (United Nations, 2017; Benjamin et al., Reference Benjamin, Muntner, Alonso, Bittencourt, Callaway and Carson2019).
Previous studies have estimated the economic burden of heart attack and stroke (e.g. Lesyuk et al., Reference Lesyuk, Kriza and Kolominsky-Rabas2018; Shafie et al., Reference Shafie, Tan and Ng2018; Luengo-Fernandez et al., Reference Luengo-Fernandez, Violato, Candio and Leal2020). This paper’s contribution is to add the marginal effects of background health indicators on the resulting diseases. This line of investigation may offer a unique, comprehensive way of looking at the economic impact of lifestyle on self-rated health determinants among older adults in Europe.
Thus, the research question was the following: ‘Do socio-demographic characteristics and risky health behaviours predict self-assessment of health?’ A derived second question was: ‘What is the probability of health outcomes (heart attack and stroke) given the presence or absence of health predictors (high blood pressure and high cholesterol)?’ and ‘What are the monetary consequences of high blood pressure and high cholesterol deriving from their association with an increased probability of heart attack and stroke?’
The data used in this study pertain to persons aged 50 or older who participated in Wave 6 (year 2015) of the Survey of Health, Aging and Retirement in Europe (SHARE): two subsamples of the age profile – younger (50–65 years of age) and older (66+) – and analysis of the sample as a whole. To ensure robust statistical results and enable cross-national comparisons, the data for the entire spectrum of eighteen countries that participated in SHARE were used.
Methods
Data source and study sample
The first wave of SHARE was carried out in 2004 in eleven countries representing various regions of Europe, from Scandinavia (Denmark and Sweden) and Central Europe (Austria, France, Germany, Switzerland, Belgium and the Netherlands) to the Mediterranean (Spain, Italy and Greece) (Börsch-Supan et al., Reference Börsch-Supan, Brandt, Hunkler, Kneip, Korbmacher and Malter2013). With time more countries began participating in the survey, such as Israel, Czech Republic, Poland, Ireland, Luxembourg, Hungary, Slovenia, Estonia and Croatia. SHARE includes information on a wide range of variables, from socioeconomic, social environment and physical functioning, to health and health behaviours among persons aged 50 or older in the first study period (Katz et al., Reference Katz, Lowenstein, Halperin and Tur-Sinai2015; Tur-Sinai & Litwin, Reference Tur-Sinai, Litwin and Börsch-Supan2015; Lowenstein et al., Reference Lowenstein, Katz, Tur-Sinai, Fernandez-Ballesteros, Robine and Benetos2019; Tur-Sinai et al., Reference Tur-Sinai, Shuldiner and Bentur2019; Shuldiner et al., Reference Shuldiner, Tur-Sinai and Bentur2020; Silverstein et al., Reference Silverstein, Tur-Sinai and Lewin-Epstein2020; Tur-Sinai & Soskolne, Reference Tur-Sinai and Soskolne2020; Carmel & Tur-Sinai, Reference Carmel and Tur-Sinai2021). The data used in the present analysis were published in Wave 6 of SHARE (Wave 6 – DOI: 10.6103/SHARE/w6.710).
The research population was comprised of persons aged 50 and older and the information collected included, among others, socio-demographic characteristics, self-reported health (SRH) indicators and risky health behaviours. The average household response rate in Wave 6 was 51.3%, ranging from 30.3% in Luxembourg and to around 56–57% in Estonia and Denmark and 69.1% in Greece (Bergmann et al., Reference Bergmann, Kneip, De Luca and Scherpenzeel2019). Individual response rates, i.e. the numbers of interviewed individuals divided by the numbers of eligible persons in the household, ranged from 74.3% in Luxembourg to 95.7% in Croatia, the average being 90.5%. The data included 67,300 interviewed individuals aged 50 and above, where 29,956 were aged 50–65 years, and 37,344 were above the age of 65 during the survey time; 45.2% of the interviewed individuals were males.
Measures
Three groups of measures and indicators were used: health measures, behavioural risk factors and socio-demographic risk factors. Together, these data provide a comprehensive view of the economic impact of lifestyle on self-rated health determinants among older adults in Europe.
Health measures
Like all sections in the survey, health measures were based on self-reported answers. Four health status measures were taken: blood pressure (BP), cholesterol level (CH), stroke (ST) and heart attack (HA) (Tong et al., Reference Tong, Lai, Yang, Ren, Dai and Lai2005; Yi et al., Reference Yi, Shin, Kim, Yi and Ohrr2018; Benjamin et al., Reference Benjamin, Muntner, Alonso, Bittencourt, Callaway and Carson2019; Chu et al., Reference Chu, Chun-Hsien, Chih-Hao, Yi Ting, Meng and Chung-Wei2020). The question was: ‘Has a doctor ever told you that you had/do you currently have any of the conditions: high blood pressure or hypertension/high blood cholesterol/a stroke or cerebral vascular disease/a heart attack, including myocardial infarction or coronary thrombosis or any other heart problem including congestive heart failure?’ The answers were coded as dummy variables of having or not having a problem with any of the four events (0=not having).
Behavioural risk factors
Some examples of risky health behaviours are smoking (1=ever smoked cigarettes, cigars, cigarillos or a pipe for a period of at least one year, 0=no), drinking habits (on an 8-point Likert scale, 0=never, 7=almost every day), obesity (measured by body mass index [BMI]) and physical inactivity, measured by two variables: light activity such as gardening, cleaning the car or going for a walk or doing a strenuous activity such as sport, heavy housework or a job that involves physical labour. Both variables were measured by self-rated answers on a scale of 1 to 4 (1=hardly ever or never, 4=more than once a week), without limiting the reported time. In addition, country differences were considered by means of a categorical variable with fifteen different values, one for each country. This was done in order to neutralize the effects of different national policies and/or norms. Nevertheless, country-specific differences were not the focus of the current inquiry and are not detailed.
Socio-demographic risk factors
Several socio-demographic variables were examined as possible predictors for the four health measures: age was measured in completed years; sex compared females (=0) with males (=1). Socioeconomic status was represented by years of education. Another variable was equalized disposable wealth of the respondent’s household (in Euros), equal to the sum of real and financial assets net of liabilities. This variable was comprised of four categories, according to level of wealth in terms of wealth distribution quartiles. Other variables were immigrant status (0=native) and living alone or not (living alone=1). Following Lee et al.’s (Reference Lee, Colditz, Berkman and Kawachi2003) finding that a high level of care provision to grandchildren may increase the risk of coronary heart disease among women, the number of grandchildren was added.
Cost of disease
To monetize health damages, the cost-of-illness (COI) method was employed. This analysis involves the measurement of resources related to an adverse effect (Leal et al., Reference Leal, Luengo-Fernández, Gray, Petersen and Rayner2006). These included not only health care costs but had a broader social cost perspective and also included opportunity costs associated with unpaid care and productivity losses associated with premature death or morbidity.
Segel (Reference Segel2006) mentions two main approaches: the prevalence approach and the incidence approach. The first estimates costs for a given time frame (usually one year) for the overall costs. The second uses costs over the lifetime of a disease. The second approach was chosen since a significant part of the costs for both heart failure and stroke lasts for more than 12 months. An important piece of information needed for the incidence approach is the survival rate (Payne et al., Reference Payne, Huybrechts, Caro, Green and Klittich2002), which should be incorporated in order to know what the life span is after the appearance of the given disease.
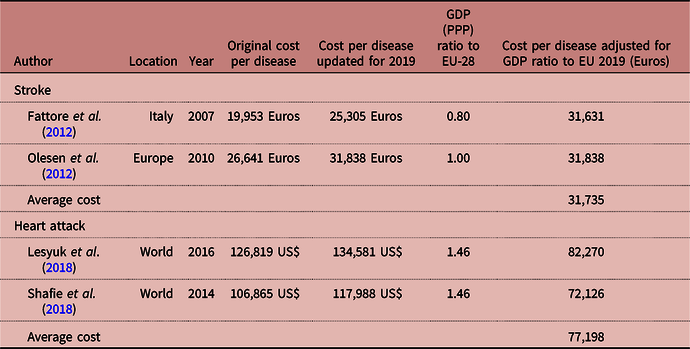
Costs-of-illness are not given in a trivial way across the literature. They combine different aspects of costs, not always the incidence cost but rather preventive, and do not always concentrate on the European continent. Nevertheless, this investigation included the latest studies that combined all these necessary characteristics: Lesyuk et al. (Reference Lesyuk, Kriza and Kolominsky-Rabas2018) and Shafie et al. (Reference Shafie, Tan and Ng2018) for heart attack and Fattore et al. (Reference Fattore, Torbica, Susi, Giovanni, Benelli, Gozzo and Toso2012) and Olesen et al. (Reference Olesen, Gustavsson, Svensson, Wittchen and Jönsson2012) for stroke. Fattore et al. (Reference Fattore, Torbica, Susi, Giovanni, Benelli, Gozzo and Toso2012) focused on Italy, and Olesen et al. (Reference Olesen, Gustavsson, Svensson, Wittchen and Jönsson2012) on all of Europe. The other two studies dealt with countries in and out of Europe but used a conversion method to international dollars that were converted into Euros.
Costs were converted to 2019 prices using the consumer price index for each country (Eurostat, 2021). National currencies were converted to Euros using 2019 exchange rates using the purchasing power parity (PPP) method. This measures the price of the same bundle of goods in different countries using Euros as a common currency, thus allowing the comparison of costs, adjusted for cost of living, between countries.
Estimation of the probability of having a heart attack or a stroke
Pairwise comparison
To estimate the conditional probabilities, the following (Bayes) equation was used:
where Pr stands for probability, DI is type of disease (HA or ST) and RF is type of predisposing risk factor (high blood pressure [BP] or high cholesterol [CH]). A combined variable (indicated by CO) in which a respondent may have the two effects together was also invoked.
The right-hand side of Equation (1) is the conditional probability of having a disease given the fact that an individual has indicated a predisposing risk factor appearance. This is equal to the ratio of the mutual probability of both risk behaviour and disease over the overall probability of individuals who reported having the predisposing risk factor.
To estimate the reduced probability of a disease, the difference between the RHS of Equation (1) and a similar equation that calculates Pr(DI/NRF) was used. This yields the reduced probability for a disease when the predisposing risk factor vanishes. This is given by:
where RP stands for reduced probability of the disease DI due to elimination of the predisposing risk factor (RF); Pr(DI/RF) is the conditional probability of the disease given the presence of a predisposing risk factor; and Pr(DI/NRF) is the probability of the disease given that there is no predisposing risk factor. (Note that another option is to calculate the odds ratio and to use the inverse of the estimate in order to estimate the reduction of probability if the risk factor is eliminated.)
Econometric estimation
To estimate the probability of having a heart attack or a stroke in old age, factors that may explain these events (predisposing risk factors) were taken into account: the probability of the patient having high cholesterol and/or having hypertension (
![]() $x$
). Also estimated was the probability of having predisposing risk factors, depending on a range of possible explanatory factors for the occurrence of one of these illnesses in old age, including behavioural risk factors (BRF) such as smoking, drinking habits, obesity and physical inactivity; and socio-demographic risk factors (DS) such as age, sex, education and equalized disposable wealth.
$x$
). Also estimated was the probability of having predisposing risk factors, depending on a range of possible explanatory factors for the occurrence of one of these illnesses in old age, including behavioural risk factors (BRF) such as smoking, drinking habits, obesity and physical inactivity; and socio-demographic risk factors (DS) such as age, sex, education and equalized disposable wealth.
The predisposing risk factors were considered as endogenous explanatory variables and the structural equation is:
where
![]() $y$
is the probability of having a heart attack or a stroke in old age and i indicates an old-aged individual.
$y$
is the probability of having a heart attack or a stroke in old age and i indicates an old-aged individual.
Due to the endogenous statistical relation between the explained predisposing risk factors variables and the probability of having a heart attack or a stroke in old age (Lehto et al., Reference Lehto, Rönnemaa, Pyörälä and Laakso2000; Tong et al., Reference Tong, Lai, Yang, Ren, Dai and Lai2005; Calvert, Reference Calvert2011), a two-stage least-square (2SLS) econometric method was applied.
In Stage 1, each endogenous variable that acts as a regressor in Equation (1) was regressed – the probability of having high cholesterol, the probability of having hypertension and the probability of having high cholesterol and hypertension concurrently – on all exogenous variables that were not included in Equation (1), i.e. the behavioural risk factors and the socio-demographic risk factors. Using this approach made it necessary to regress each endogenous variable being used as a regressor on all the exogenous variables in the system and using the estimated value of the endogenous variable from this regression as the required instrumental variables (Schouten, Reference Schouten2018). Each estimated value was the ‘best’ instrumental variable in the sense that, of all combinations of the exogenous variables, it had the highest correlation with the endogenous variable (Kennedy, Reference Kennedy2008). Therefore, the first-stage equation was:
where
![]() ${x_i}$
is the probability of the patient having high cholesterol and/or having hypertension.
${x_i}$
is the probability of the patient having high cholesterol and/or having hypertension.
In Stage 2, the probability of having a heart attack and that of having a stroke was estimated given the estimated probability of the occurrence of one of the previous conditions. In other words, the second-stage equation was:
where
![]() ${\hat x_i}$
are the fitted values derived from Equation (4).
${\hat x_i}$
are the fitted values derived from Equation (4).
The derived reduced probability here involves a variant of instrumental-variables estimation as explained above, as it comes to insurance in the regression coefficient of either BP or CH on either one of the regressions: HA and ST.
Results
Descriptive statistics
The descriptive statistics of the research population are presented in Table 1. The average age of participants was 65.6 years. Less than a half were men (45.2%), 44.6% of those aged 50–65 were men, while 45.9% of the people age 65+ were men. Average formal education was 10.6 years, and only 10.5% were immigrants. A quarter of the sample declared that they were living alone. The average number of grandchildren was 2.9.
Table 1. Descriptive characteristics of older adults in eighteen European countries, SHARE Wave 6
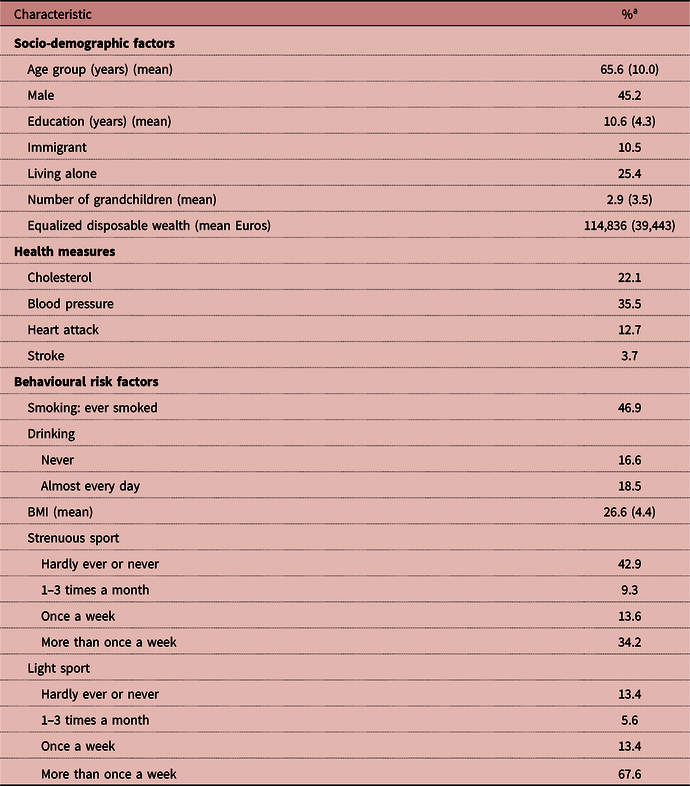
a Percentages unless indicated otherwise. Values in parentheses are standard deviations.
In response to the question of whether they had ever or still had a high blood cholesterol problem, 22.1% of the participants said they had; when asked about high blood pressure or hypertension, 35.5% of them endorsed. When asked whether they had ever had a heart attack, including coronary thrombosis, or any other heart problem, including congestive heart failure, 12.7% declared that they had, but only 3.7% responded positively to the same question regarding stroke or cerebral vascular disease. The percentage who stated they ever smoked was 46.9%; 16.6% declared they never drank, 18.5% declared that they drank almost every day and the answers of all the others fell between these two.
Previous research has indicated a problem of overweight among older adults (according to BMI) (Adams et al., Reference Adams, Schatzkin and Harris2006; Peralta et al., Reference Peralta, Ramos, Lipert, Martins and Marques2018). Two-thirds of the research participants indicated that they engaged in light sport more than once a week, but only one-third said they engaged in more strenuous sport more than once a week. Finally, 42.9% of the participants reported that they hardly ever or never engaged in any strenuous sporting activity.
Pairwise probabilities: separate, mutual and conditional
Table 2 describes different pairwise probabilities of risk factors and diseases by age. The upper section (the first three rows) shows the probabilities of being identified with predisposing risk factors, i.e. high cholesterol (CH), high blood pressure (BP) or either one. The next two rows present the probabilities of each of the diseases heart attack (HA) and stroke (ST) and the middle section describes the probability of having both. The final section describes the conditional probabilities, i.e. the likelihood of being identified with a disease conditional upon having or not having a predisposing risk factor.
Table 2. Pairwise probabilities of risk factors and diseases

a See Methods section for calculation of conditional probabilities.
The findings indicate that age was a significant factor in the probability of heart attack and stroke. The probability of being identified with HA increased from 0.071 for ages 50–65 to 0.194 (an increased predisposing risk ratio of 2.73) for ages 66+. Stroke affected 0.018 of the population aged 50–65 but escalated to 0.058 for ages 66+. High CH level was associated with 0.199 of the 50–65 age group, compared with 0.246 for the 66+ group. A similar trend was seen for BP. High BP was associated with 0.283 of the younger population (50–65) and 0.441 of the older population (66+).
Mutual probability followed the same trend. Age was a significant factor in all the combinations involved. The same trend was found in the conditional probabilities. However, age was a non-manageable variable. The differences within the age groups with respect to with and without predisposing risk factors are probably more important. For example, a person who is no longer characterized by a high cholesterol level has reduced his or her probability of HA from 0.212 to 0.103. This reduction accounts for a 51% reduction in the original probability.
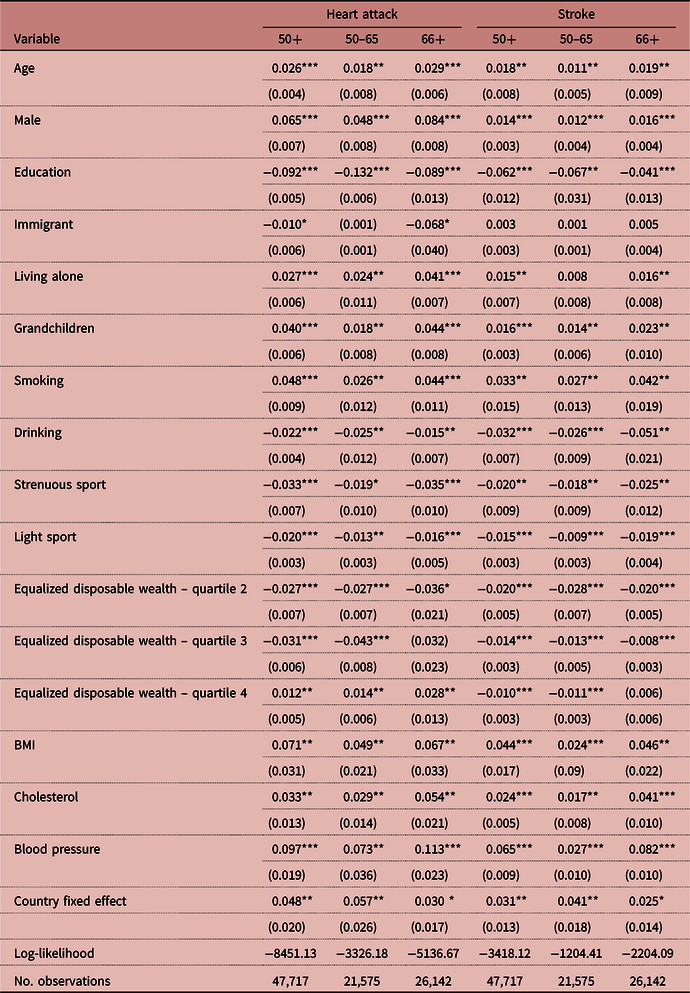
Econometrics analysis
The model reports on the regression in which the relevant explanatory variables were defined as having either of the two predisposing risk factors (dummy=1). In Stage 1, the probability of having a high cholesterol problem and/or a blood pressure problem in old age was estimated. In Stage 2, the probability of having a heart attack in old age was estimated given the probability of having a high cholesterol problem and/or a blood pressure problem in old age. To estimate the probability of having a stroke in old age, given the probability of having a high cholesterol problem and/or a blood pressure problem in old age, both stages were repeated. The coefficients are presented as average marginal effects (AME). Multiplying the marginal effect by 100 yields the change in percentage points (Achdut et al., Reference Achdut, Tur-Sinai and Troitsky2015).
Table 3 shows the Stage 2 estimators from the 2SLS procedure. It demonstrates the impact of having a high cholesterol problem and/or a blood pressure problem on the probability of suffering a heart attack or stroke in old age. Observation of the magnitude of the marginal effects of the explanatory variables reveals that the probability of having high cholesterol or high blood pressure raised the probability of a heart attack by 11.3% for the entire sample. Splitting by age groups indicated an increased risk of only 9.3% among those in the 50–65 age bracket, and 14.1% among those aged 66+. A one-unit increase in BMI raised the probability of having a heart attack by 6.9% overall, by only 4.8% in the 50–65 age bracket and by 7.0% among those aged 66+.
Table 3. Probability of having a heart attack or stroke by age, given a cholesterol and/or a blood pressure problem (2SLS results, second stage, marginal effect)
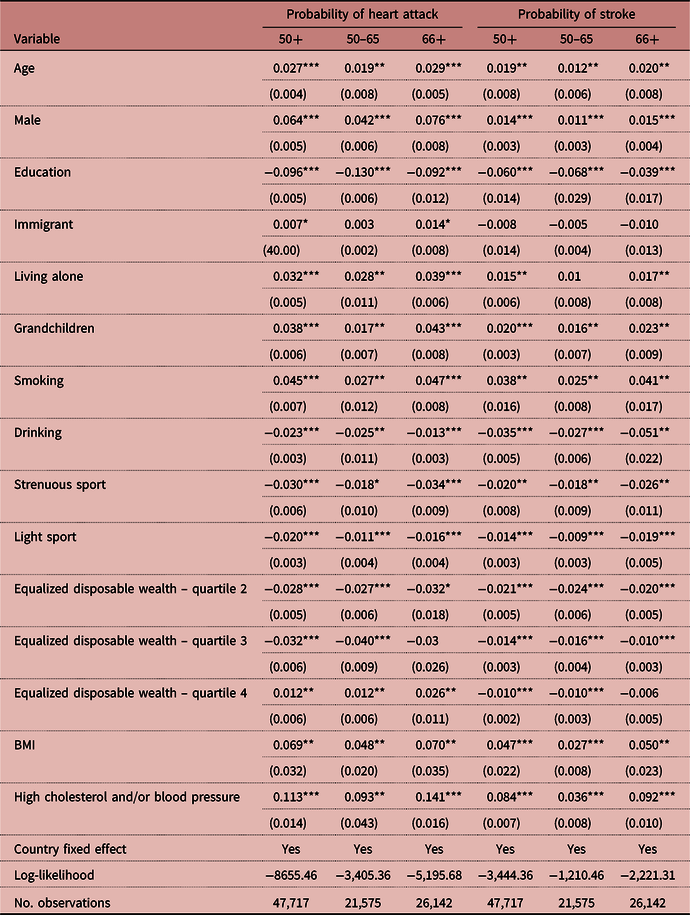
Standard errors in parentheses.
***p<0.01; **p<0.05; *p<0.1.
The probability of having a heart attack increased with age: each year increased the likelihood of having a heart attack by 2.7%, so that the likelihood of those aged 66+ was greater than those aged 50–65 (2.9% compared with 1.9%). In addition, the results indicate that the probability was greater among men than among women aged 50+ (by 6.4%). Being a native of one’s country of residence decreased the likelihood of having a heart attack by 1.2% (Sohail et al., Reference Sohail, Chu, Rezai, Donovan, Ko and Tu2015); each additional grandchild raised it by 3.8%; and living alone had a similar impact (a marginal effect of 3.2%).
The findings regarding the behavioural risk factors show that smoking increased the probability of having a heart attack by 4.5%, but all the other factors had the opposite influence: drinking, engaging in strenuous sport and engaging in light sport decreased the probability of having a heart attack by 2.3%, 3.0% and 2.0%, respectively. In addition, an increase in equalized disposable wealth decreased the likelihood of having a heart attack. Finally, country differences were significant, justifying that they have been controlled (with fixed effects for each country included).
Analysis of the effect of having high cholesterol or blood pressure on the probability of having a stroke revealed somewhat different results to those regarding heart attack. The probability of having high cholesterol or blood pressure increased the probability of suffering a stroke by 8.4%, in general. However, the figure for those aged 50–65 was only 3.6%, and for the group aged 66+ it was 9.2%. A one-unit increase in BMI increased the probability of a stroke by 4.7%, in general, by age 2.7% for the 50–65 age bracket and by 5.0% among those aged 66+.
The findings indicate an increase in the probability of having a stroke with age: each year increased the likelihood of having a stroke by 1.9%, with the likelihood among those aged 66+ being greater than among those aged 50–65 (2.0% compared with 1.2%). The analysis indicated that the probability was 1.4% greater among men than among women. Each additional grandchild raised the probability of having a stroke by 2.0% and living alone had a very similar impact (a marginal effect of 1.5%).
The findings regarding the behavioural risk factors showed that smoking increased the probability of having a stroke by 3.8%. All other factors affected the probability of stroke in the opposite direction: drinking, engaging in strenuous sport and engaging in light sport decreased the probability by 3.5%, 2.0% and 1.4%, respectively. In addition, an increase of equalized disposable wealth decreased the likelihood of having a stroke. Finally, country differences were significant, justifying having been controlled. It might be that country-specific differences occur due to national policies, as well as other assimilated factors. Country-specific differences were not the focus of the current inquiry and are not detailed. A further research will give a special attention to this social aspect.
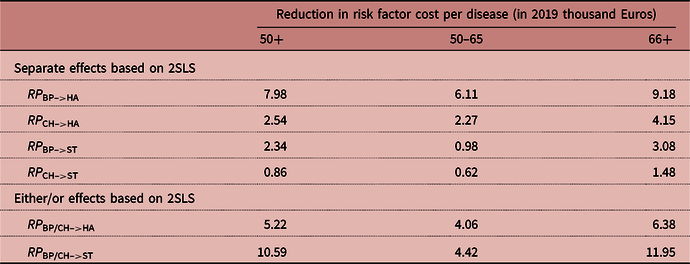
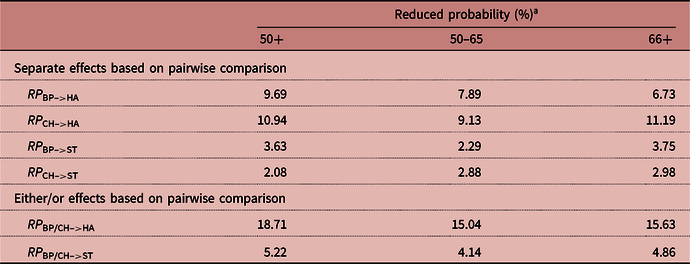
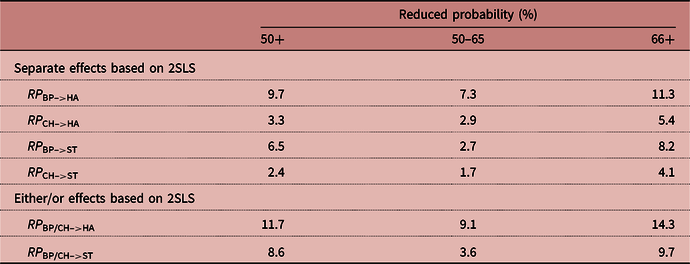
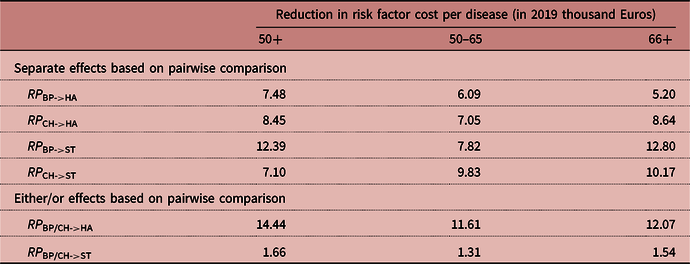
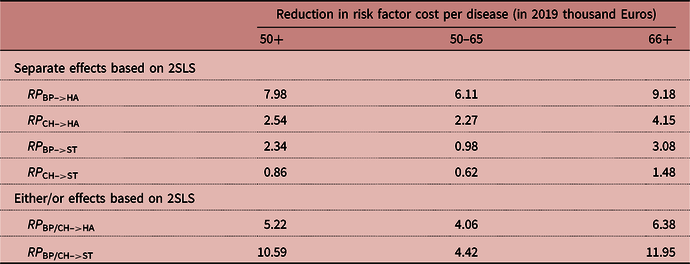
Tables 4 and 5 present a summary of the reduced probabilities based on the models described above. Table 4 shows the reduced probabilities for the pairwise comparison while Table 5 presents the reduced probabilities for the regression analysis. The range of reduced probabilities was from as low as 1.7% for the effect of high cholesterol level on probability of stroke for ages 50–65 up to 11.3% effect of high blood pressure on the probability of heart attack. Both cases are for the regression analysis.
Table 4. Reduced probability due to elimination of a risk factor based on pairwise comparison
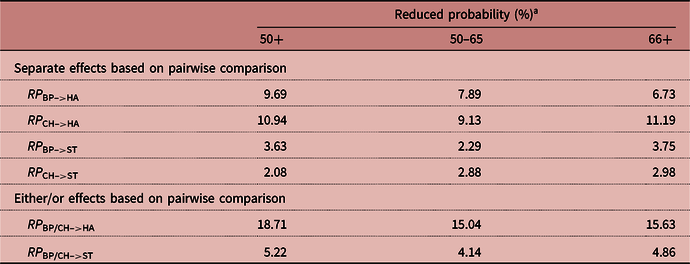
a See Methods section for calculation of reduced probabilities.
Table 5. Reduced probability due to elimination of a risk factor based on regression coefficients
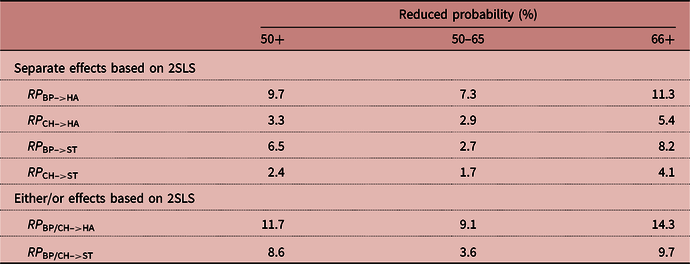
To estimate the impact of a single risk factor, another equation not discussed in the paper but shown in Table 6 was estimated.
Table 6. Regression table with coefficients indicating the single impact of a risk factor (2SLS results, second stage, marginal effect)
Standard errors in parentheses.
***p<0.01; **p<0.05; *p<0.1.
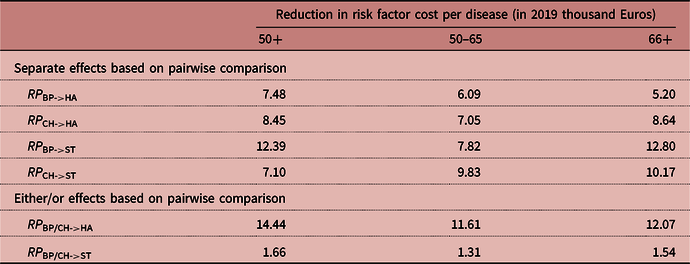
Cost of illness
Table 7 shows the data on heart attack and stroke on the basis of the various studies surveyed. To obtain a single estimate only, the geometric mean of the different studies for the two events was used. The mean costs for heart attack and stroke were 77,198 Euros and 31,735 Euros, respectively. To calculate the expected cost reduction due to elimination of a predisposing risk factor, the reduced probability due to elimination of the given risk factor (BP, CH) was multiplied by the cost per disease (HA, ST). The results are presented in Tables 8 and 9 for the pairwise and regression analysis, respectively. As can be seen from the tables, the marginal benefit of eliminating a predisposing risk factor depends on the disease and the age and ranges from 0.62 thousand Euros (effect of high cholesterol on the probability of stroke for age 50–65 in the case of regression analysis) up to 12.8 thousand Euros (effect of high blood pressure on the probability of stroke in the pairwise comparison analysis).
Table 7. Summarized data for the incidence cost of diseases from different sources
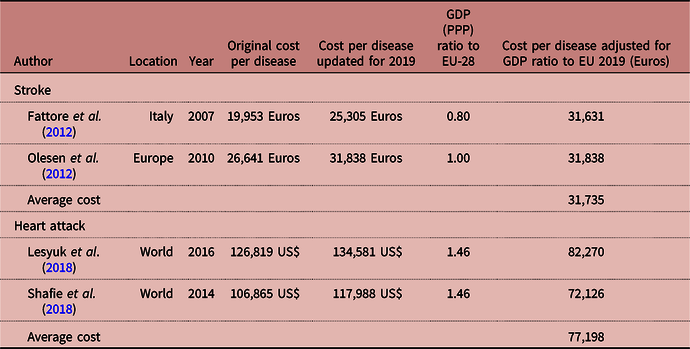
Table 8. Monetary estimate for reduction in risk factor cost per disease based on pairwise comparison
Discussion
The two predisposing risk factors high blood pressure (BP) and high cholesterol (CH) were found to be significant in all cases, when they were taken separately and in the either/or form. Furthermore, the role of sex was found to be significant. In all age groups, men had a higher risk than women of suffering both heart attack and stroke. There is no a priori evidence of a given sign (that men should have a higher risk than women of suffering both heart attach and stroke) in the literature (Bardage et al., Reference Bardage, Pluijm, Pedersen, Deeg, Jylha and Noale2005; Kunst et al., Reference Kunst, Bos, Lahelma, Bartley, Lissau and Regitor2005). A few studies have investigated the association between sex and general health, but the results have not been consistent. For example, a study conducted in Taiwan found that women had an increased tendency for deterioration of health, expressed in a decline in ADLs (Activity of Daily Living) (Pan et al., Reference Pan, Hung, Shaw, Lin, Lee, Chiu and Su2005), but a study of self-reported health in eleven European countries based on SHARE 2004 (Wave 1) data concluded that, in most instances, women were significantly less likely than men to report poor as opposed to very good health (Verropoulou, Reference Verropoulou2009).
The importance of socioeconomic status for health outcomes is well established in the international literature (Kunst et al., Reference Kunst, Bos, Lahelma, Bartley, Lissau and Regitor2005; Tubeuf et al., Reference Tubeuf, Jusot and Bricard2012). In the current analysis, this was represented by educational attainment, a variable that has been found to be an important indicator among older adults (Tsimbos, Reference Tsimbos2010). For example, a European study based on SHARE data indicated a strong association between level of education and the probability of having a high quality of life (which includes health aspects) among older adults (Wahrendorf et al., Reference Wahrendorf, Knesebeck and Siegrist2006). Brunello et al. (Reference Brunello, Fort, Schneeweis and Winter-Ebmer2016) found about a 30% impact of education on good health status. Braakmann (Reference Braakmann2011), however, found no causal effect between education and health status but his study did not concentrate on older adults.
Living alone was found to increase the likelihood of having a heart attack or stroke. These findings support prior studies, which found that loneliness was a significant risk factor for coronary heart disease among older adults (Sorkin et al., Reference Sorkin, Rook and Lu2002; Gomes et al., Reference Gomes, Santos, Christofaro, Santos and Júnior2013; Shiovitz-Ezra & Litwin, Reference Shiovitz-Ezra, Litwin, Nyqvist and Forsman2015). Lastly, in a study on health disparities between blacks and whites, Sharma (Reference Sharma2012) concluded that lower levels of education have a highly significant effect on health. Income, a factor associated with high educational attainment, has also been shown to significantly impact health status (Bós & Bos Reference Bós and Bos2007; Jang et al., Reference Jang, Choi and Kim2009).
Another advantage of using level of education as a variable is its establishment early in life, so that it is not affected by subsequent decline in health and is a fairly robust measure for addressing issues of causality. The findings of the present research suggest that higher educational attainment has a strong protective effect, significantly reducing the chances of a decline, at least in the two diseases examined in this study. In addition, a higher number of grandchildren increased the probability of having either of the studied diseases. This might be explained by the role of many older adults in caring for and feeding their grandchildren, which might be accompanied by changes in their own regular diet and increase the risk of coronary heart disease (Lee et al., Reference Lee, Colditz, Berkman and Kawachi2003).
Regarding the role of behavioural risk factors, in the present study, levels of physical activity were strongly negative associated with a decline in SRH. Leinonen et al. (Reference Leinonen, Heikkinen and Jylha2001), Holme and Anderssen (Reference Holme and Anderssen2015) and Humphreys et al. (Reference Humphreys, McLeod and Ruseski2014) reported similar results. A negative association was also found between obesity, either measured by BMI or self-reported. Smoking has been shown to be negatively related to a lower level of self-reported health (Mohammadnezhad et al., Reference Mohammadnezhad, Tsourtos, Wilson, Ratcliffe and Ward2015), while in contrast, drinking alcohol four to five times a week was found to significantly increase the chances of having a higher-level health status. Antonanzas et al. (Reference Antonanzas, Rodrigues-Ibeas, Barco, Ramirez and Pinillos2008), Horton (Reference Horton2015) and Davies et al. (Reference Davies, Cillard, Friguet, Cadenas, Cadet and Cayce2017) supported this result, by arguing that there was evidence of some health benefits related to wine consumption. They showed what is called the ‘French paradox’ theme, where epidemiological studies indicate that consumption of alcohol can reduce risk coronary heart disease.
As expected, this study found that age had a significant coefficient, both within and between the two age brackets (Rudd et al., Reference Rudd, Hoffman, Down, Pearson and Lowe2007; Stenholm et al., Reference Stenholm, Westerlund, Head, Hyde, Kawachi, Pentti and Vahtera2015). Each year from age 50 to age 65 contributed 1.8% and 1.1% to the chances of heart attack and stroke, respectively. These percentages increased to 2.9% and 1.9% for the population aged 66+. Finally, being an immigrant was not a significant factor for stroke in either age group (Sohail et al., Reference Sohail, Chu, Rezai, Donovan, Ko and Tu2015). This finding supports the assumption that the probability of suffering a stroke is mainly affected by general health, socio-demographic and behavioural risk factors, which are not significantly different among European countries. Another factor that was found not to be significant was the third quintile of equalized disposable wealth among the 66+ age group regarding heart attack.
This analysis concentrated on the cost and probability estimation of two diseases, namely heart attack and stroke. As can be seen from Table 8, the benefit of reducing one disease ranges between 5.2 and 12.8 million Euros per saved case. However, this should not serve as the basis for suggesting resource allocation. For that purpose, it is also necessary to include the difference in the cost of treatment of heart attack and stroke, which was beyond the scope of the present research.
The analysis shows a significant reduction of the probability of self-reporting one of two adverse events (heart attack and stroke) with and without two predisposing risk factors (BP and CH). The estimates for the costs of both diseases were the corner stone for estimating the marginal effect of risk factors. But these reflect only a part of what should be considered when studies based on cost-benefit analysis or cost-effectiveness are to be carried out. Studies of the cost-of-illness method, as those that Table 7 was based on, can be combined with studies that measure the effect of risk factors on diseases (e.g. Kronish et al., Reference Kronish, Lynch, Oparil, Whittle, Davis and Simpson2016; Ahmed et al., Reference Ahmed, Hameed and Abd-Ali2017; Yi et al., Reference Yi, Shin, Kim, Yi and Ohrr2018; Chu et al., Reference Chu, Chun-Hsien, Chih-Hao, Yi Ting, Meng and Chung-Wei2020). Conditional probability based on either self-report or a more objective assessment can lead to a more educated budget allocation based on monetary value per reduced health hazard unit value.
Conclusion
Smoking, physical inactivity, unhealthy diet, obesity and other lifestyle behaviours are known to be associated with the development of diseases such as cancer, heart disease, stroke and diabetes (Lopez et al., Reference Lopez, Mathers, Ezzati, Jamison and Murray2006). Previous studies have investigated the effects of single lifestyle behaviours on health, but a combined and conditioned probability approach may yield a more accurate picture. Predictions should consider several variables, including not only lifestyle but also health factors (e.g. the effect of blood pressure on heart attacks). Using data on the self-reported health of persons aged 50 or higher, as reported in Wave 6 of SHARE, factors were sought that might predict a decline or an improvement in two diseases, namely heart attack and stroke. The results of reduced probabilities were then used to assess the expected cost of eliminating one of two predisposing risk characteristics, namely high blood pressure (BP) and cholesterol (CH).
The results revealed the significant role of socioeconomic status, particularly educational attainment, in health outcomes. The findings of the study demonstrated that higher educational attainment had a strong protective effect, significantly reducing the chances of deterioration, at least in the two diseases examined. In addition, a higher number of grandchildren raised the probability of having either of the diseases. This may be explained by the role of many older adults in caring for and feeding their grandchildren, which may be accompanied by some changes in their own regular diets. As expected, the findings demonstrate a significant coefficient, both within and between the two age brackets. In addition, immigrant status was found not to be a significant factor for any age group regarding stroke risk. This result supports the assumption that the probability of suffering a stroke is mainly affected by general health, socio-demographic and behavioural risk factors and are not significantly different among European countries. Income, a factor associated with high educational attainment, was also found to significantly impact health status.
Regarding the role of behavioural risk factors, in the present study low and high levels of physical activity were strongly related to a decline in self-reported health. Obesity, as measured by BMI, was negatively associated with a decline in self-reported health. By contrast, drinking alcohol four to five times a week significantly increased the chances of improvement in the health status. This result is being supported by the ‘French paradox’ theme (Antonanzas et al., Reference Antonanzas, Rodrigues-Ibeas, Barco, Ramirez and Pinillos2008; Horton, Reference Horton2015; Davies et al., Reference Davies, Cillard, Friguet, Cadenas, Cadet and Cayce2017). Smoking was also found to be significant. Another factor that was found not to have a significant effect was the third quintile of equalized disposable wealth among the age group of 66+ regarding heart attack. Finally, country differences were significant, justifying there having been controlled.
The study finding support the claim that socioeconomic factors, age, income and behavioural risk factors are the most powerful predictors of a decline, or improvement, in the risk for heart attack and stroke. Since national health budgets are limited, health policies such as screenings and brief interventions might be prioritized by such studies and especially by the cost required to achieve a given goal as estimated monetarily in the paper.
Risk behaviour was found to be a significant component that determines the probability of being identified with heart attack and stroke. Two models are presented in which monetary estimates could be derived for the marginal effect of one or two risk behaviours on the probability of suffering one of these diseases. More studies should attempt to estimate the different risk behaviours for different diseases. This can be done either by self-reported surveys or more objective risk assessments. The study has one limitation that should be mentioned: it was a pure cross-sectional analysis that could adequately answer the question of causality.
Acknowledgments
This study used data from SHARE Wave 6 (doi: 10.6103/SHARE.w6.600; see Börsch-Supan et al. (Reference Börsch-Supan, Brandt, Hunkler, Kneip, Korbmacher and Malter2013) for methodological details. The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: No. 211909, SHARE-LEAP: No. 227822, SHARE M4: No. 261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the US National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Funding
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.