Published online by Cambridge University Press: 21 January 2005
Coronary artery fistulas are uncommon in children. We conducted a retrospective review of the case notes of 17 children who presented to our institution with the diagnosis of a coronary fistula since 1970. Their median age was 2.3 years. In five patients, there were associated congenital cardiac anomalies, with four having these as part of the spectrum of tetralogy of Fallot. Surgical correction was performed in nine patients, while in five closure was achieved using percutaneous embolization with coils. No complications or deaths were encountered related to the treatments chosen. In two patients, further procedures were needed to close residual fistulas. The median follow-up was 16 years, and on echocardiography, all fistulas appeared to be successfully closed, albeit that we lost three patients to follow up. We also conducted a review of 426 cases of coronary fistulas reported in children in the English literature. We have compared these findings with our institutional experience.
Coronary artery fistulas are frequently associated with other forms of congenital cardiac disease. Of those described one-quarter drain into the pulmonary circulation (Figs 1 and 2).

Figure 1. Angiogram with contrast injection into the ascending aorta (Ao) demonstrating a large coronary fistula (arrows) supplying the pulmonary arteries. RPA: right pulmonary artery.

Figure 2. Angiogram with contrast injecton into a coronary fistula (CF) via the ascending aorta demonstrating the fistula filling the pulmonary arteries with contrast. The left coronary artery (arrows) is shown to originate from behind the proximal third of the fistula. RPA: right pulmonary artery; LPA: left pulmonary artery.
Small fistulas may close spontaneously, or remain clinically silent. Larger fistulas rarely close spontaneously, and closure is usually established either surgically, with or without the use of cardiopulmonary bypass, or percutaneously.
The objective of this study was to describe our experience of treating these anomalies, comparing our findings with a review of all reported cases in the literature, summarizing the diagnostic and therapeutic strategies. Special emphasis was placed on fistulas associated with other forms of congenital cardiac disease, and fistulas draining to the pulmonary circulation.
From our departmental database, we identified all patients who presented to our institution since 1970 with a subsequent diagnosis of a coronary arterial fistula. The data was supplemented with information obtained via a retrospective review of the case notes. We excluded patients who had small fistulas or sinusoidal communications associated with a diagnosis of pulmonary atresia with intact septum or hypoplastic left heart syndrome.
In addition, we reviewed all reported cases of coronary arterial fistulas described in children in the English literature. Cases were identified using a standard Medline search. Basic data with regards to the course of the fistula, clinical symptoms, and treatment were extracted from the original articles and/or abstracts, and stored together with our institutional data in an electronic database (Microsoft Access). Statistical analysis was performed using StatsDirect (StatsDirect Ltd.) software, which provided us with standard descriptive reports.
Since 1970, we have treated 17 patients with the diagnosis of coronary arterial fistulas (Table 1).
Table 1. Series of patients with coronary fistulas.
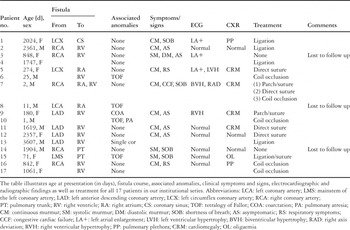
Just over half the patients were female, and the median age at presentation was 2.3 years, with a range from 1 day to 9.8 years. Associated cardiac anomalies that required surgical treatment were present in five patients, and included tetralogy of Fallot with pulmonary stenosis in three cases, and tetralogy with pulmonary atresia and aortic coarctation in one case each. A single coronary artery had been found in one patient. Shortness of breath or other respiratory tract symptoms were present in six patients, whereas five patients were completely asymptomatic. None had presented with complications related to the fistula. A typical continuous murmur was present in eight patients.
Electrocardiographic abnormalities were identified in five patients, predominantly atrial enlargement or ventricular hypertrophy. No patient had ischaemic changes. An increased cardiothoracic ratio was identified on a plain chest X-ray in four patients, pulmonary plethora in two, and three patients had a completely normal chest X-ray. More than one fistula was present in one patient.
In eight patients, the fistula originated from the left coronary arterial system, and in five from the right. The most common site of drainage was the right ventricle in 10 patients, followed by the right atrium in three patients, the pulmonary trunk in two patients, and the coronary sinus in one patient.
The correct diagnosis was made, or suggested, by trans-thoracic echocardiography in five patients. Coronary angiography was performed in all patients. Only one patient had a left-to-right shunt in excess of 2:1.
All but three patients, who were lost to follow up, underwent definitive treatment of the coronary fistula. Dual surgical procedures were needed in one patient, specifically closure of one fistula joining the right coronary artery to the right ventricle, and closure of another fistula between the right coronary artery and the right atrium. In this patient, a residual fistula was occluded percutaneously with coils nine years after the initial surgical procedures. In eight patients, the fistulas were treated exclusively surgically, with the patient described above requiring both surgical and percutaneous procedures. Of the ten surgical procedures performed, four entailed ligation of the fistula, three involved closure by direct suture, and the remaining three were achieved by insertion of patches or combined approaches. All surgical procedures involved the use of cardiopulmonary bypass.
Percutaneous occlusion using coils was chosen in five patients. In one patient, we required three successive attempts at embolization to achieve complete occlusion of the fistula. No complications were encountered during these procedures.
We lost three patients to follow up. The median follow-up in the remainder was 16 years, with a range from 1.5 years to 28 years. All patients remain well, without any evidence of residual or recurrent fistulas.
We found a total of 426 cases of coronary fistulas reported in children in the English literature, with 106 cases associated with congenital cardiac disease in any age group (Table 2).
Table 2. Congenital cardiac malformations associated with coronary fistulas.

Of the 106, 88 were described in children, this accounting for just over one-fifth of all fistulas reported in this age group.
The most commonly associated anomaly was the spectrum of tetralogy of Fallot, including tetralogy with pulmonary atresia, this accounting for just over two-fifths of the reports.
Where adequate information was available concerning the origin, which was described in 375 cases, and termination, described in 342 cases, we identified 55% of the reported fistulas as originating from the left coronary arterial system, 37% from the right coronary system, and 8% to have multiple origins in the left and right coronary arteries (Table 3).
Table 3. Reported origin and termination of coronary arterial fistulas in children.

The site of termination was most commonly the right heart (65%), followed by pulmonary arteries (23%), left heart (11%), and combined left and right heart (1%). In only one case was simultaneous cardiac and pulmonary termination of the fistula described.1 Multiple fistulas were described in 34 cases.
The most frequently described clinical presentation in childhood is an asymptomatic patient with an audible murmur, which was present in more than half of reported cases. Out of 293 cases reported in children with adequate clinical details, 119 patients (40%) had symptoms that could be related to the presence of the fistula, such as non-specific respiratory symptoms, shortness of breath, or chest-pain.
We identified 23 reported children with spontaneous closure of the fistula. Of these, two had mild, non-specific, associated symptoms.2, 3
Surgical intervention to close the fistula, occasionally as part of corrective surgery for an associated cardiac malformation, was reported in more than 45% of children, 195 cases, whereas to date percutaneous closure of the fistula has been reported in just under one-tenth (39 cases).
We present our experience of treating 17 children with congenital coronary arterial fistulas seen over a period of 32 years. Our experience is in keeping with the reported incidence of one fistula in every 500 patients who undergo cardiac catheterization.4, 5 Rarely, acquired fistulas have been described after cardiac trauma or cardiac surgery,6–9 albeit that no such cases were encountered in our practice.
Among our series of 17 patients, we identified four with tetralogy of Fallot with pulmonary stenosis or atresia, this being the most frequently reported associated group of congenital cardiac anomalies. Although large solitary fistulas are occasionally observed in tetralogy of Fallot, smaller fistulas are more common. Dabizzi et al.10 reported a series of 265 angiographic studies in patients with tetralogy of Fallot, and identified 20 cases with small fistulas between the coronary and pulmonary arteries, and 42 anastomoses between coronary and bronchial arteries or the right atrium. Coronary arterial fistulas in tetralogy of Fallot are a diagnostic challenge, as the characteristic symptoms and signs related to the fistula are usually masked by the underlying cardiac anomaly. Unexpectedly high systemic arterial saturations may suggest an additional source of pulmonary blood supply,11 but diagnosis is usually made during routine angiographic evaluation, as was the case in our patient.
Most reported institutional series of congenital coronary arterial fistulas are small, and therefore vary widely with regards to individual frequency of origin and termination of the fistula. The right coronary artery has been reported to be involved in between one-twelfth and two-thirds of cases, with the pulmonary trunk being the site of insertion in between one-twentieth and three-fifths of cases.2, 8, 9, 12, 13 Our report provides data based on a large number of reported cases, and could serve as a more accurate guide to the individual frequencies of these fistulas.
In our series, all patients with adequate documented information had an audible cardiac murmur. This is in keeping with other institutional series.7–9, 14, 15 Most of the patients in our series were asymptomatic, or had only mild non-specific symptoms. No complication related to the fistula, such as myocardial ischaemia, rupture or thromboembolism, was encountered in any patient, which again is in keeping with other reported series. Liberthson et al.15 reported preoperative symptoms or complications related to the fistula to be present in two-thirds of their patients aged above 20 years, compared to only one-fifth of patients below the age of 20 years.
Prior to the use of high resolution cross-sectional and Doppler echocardiography, the diagnosis was usually confirmed via angiography or as an incidental finding intraoperatively. Echocardiography is now the primary tool for diagnosis of these anomalies,8 and was valuable in suggesting the correct diagnosis in five of our patients. Angiography, nonetheless, is usually undertaken to confirm diagnosis, and nowadays catheterization will allow attempted percutaneous closure of the fistula.
Changes in the electrocardiogram observed in our patients were non-specific. These findings were usually secondary to volume loading of the cardiac chambers serving as the termination of the fistula. Ventricular hypertrophy was present on electrocardiographic recordings in between one-sixth and towthirds of larger series.2, 9, 14 Ischaemic changes are uncommon in children, but become more frequent with increasing age and can, on occasion, be induced with an exercise tolerance test.16
In seven of our patients, chest radiography demonstrated either cardiomegaly or pulmonary plethora. Larger institutional reviews have reported an abnormal film to be present in between one-tenth of silent fistulas, and up to three-quarters of patients who required surgical intervention.2, 9, 14 We identified nine reported cases where an abnormal chest radiograph was the main reason for referral to the cardiologist.
The natural history of the fistulas is variable. In our series, we did not observe spontaneous closure, and all but two of our patients with isolated fistulas underwent surgical or percutaneous closure within a median of 5 months of presentation. Sherwood et al.6 reported their institutional experience of 31 patients with small and clinically silent fistulas, and observed seven cases of spontaneous closure. Once patients develop clinical symptoms secondary to the fistula, the likelihood of spontaneous closure is very much reduced. Of the 23 cases we discovered reported in children where spontaneous closure was observed, only two patients had mild symptoms that might be ascribed to the fistula.
The majority of patients in our series, as well as in the literature, were treated surgically with the use of cardiopulmonary bypass. In selected cases, an approach without the use of cardiopulmonary bypass is feasible. Mavroudis et al.7 reported their surgical experience with 17 cases, and found that in more than half it was possible to ligate the fistula epicardially, without the need for cardiopulmonary bypass. They reserved cardiopulmonary bypass for lesions that were inaccessible, or for patients where a correction of an associated cardiac malformation was required.
The percutaneous approach has been less commonly used to close these fistulas. Nonetheless, when considering reports published after 1995, more than one-third of fistulas have been treated by transcatheter closure, with favourable results. Qureshi et al.17 reported a series of percutaneous closure in 40 patients using coils, detachable balloons, and the Amplatzer duct occluder in selected patients. They achieved a total occlusion rate of 97%. One infant died within with 6 hours of the procedure, and embolization of a coil or balloon occurred in one-sixth. All coils were successfully retrieved.
The availability of a wide range of different transcatheter devices allows a percutaneous approach to a wide variety of fistulas. The Amplatzer plug appears to be especially suitable for closure of larger fistulas, and initial results have been encouraging.17–22 Even closure of very large fistulas in small infants can be successfully achieved using multiple devices.23
In conclusion, our results have demonstrated that, generally, coronary arterial fistulas in childhood are associated with low morbidity and mortality. We propose a conservative approach to the treatment of these anomalies in asymptomatic patients, with careful monitoring, which could allow some fistulas to close spontaneously. If spontaneous closure does not occur, or if patients develop symptoms or complications, then surgical or percutaneous closure should not be delayed. Percutaneous closure should now be the first-line treatment for these children, with surgical procedures reserved for those cases where correction of associated anomalies is required, or where the anatomy of the fistula precludes a successful percutaneous approach.

Table 1.

Table 2.

Table 3.