Families of children with trisomy 18 and trisomy 13 experience cumulative messaging from foetal through paediatric care that these diagnoses are incompatible with life or universally associated with a poor quality of life.Reference McGraw and Perlman1,Reference Adams and Winslade2 In a survey including 330 parents of children with trisomy 18 and trisomy 13, respondents reported they were told by health care providers: “that the condition of their baby was lethal or incompatible with life (93%), that their child would be a vegetable (55%), that their baby would destroy their family or their marriage (28%), and that if their baby survived, he would live a meaningless life (55%) or a life of suffering (68%).”Reference Guon, Wilfond and Farlow3 Cardiac surgical intervention offerings for children with trisomy 18 and trisomy 13, even those carefully selected based on feasibly correctable cardiac conditions, remain controversial in this decade.Reference Janvier, Okah and Farlow4–Reference Cooper, Riggs and Zafar6 The controversy in offering cardiac surgical interventions for this paediatric population has focused not only on the feasibility of prolonging the child’s quantity of days through surgical interventions but also on the providers’ perspectives on the child’s quality of life in the setting of these genetic diagnosis.Reference Pallotto and Lantos7,Reference Lantos8 Some perceive that cardiac surgical interventions have not improved outcomes in a way warranting the use of critical and costly resources.Reference Graham9 As recent studies have demonstrated that meaningful survival outcomes can be achieved with cardiac surgery for selected children with trisomy 18 and trisomy 13 diagnoses, there is a recognised need to explore the quality of life in these patient cohorts.Reference Muneuchi, Yamamoto and Takahashi10–Reference Maeda, Yamagishi and Furutani13 The concluding research recommendation from a large retrospective review of outcomes after cardiac interventions in infants with trisomy 18 and trisomy 13 was a call to assess quality of life issues for these patients and their families.Reference Peterson, Calamur and Fiore14
Ninety percent of babies with trisomy 18 and eighty percent of patients with trisomy 13 are concurrently diagnosed with CHD,Reference Baty, Blackburn and Carey15 primarily septal defects, patent ductus arteriosus, vulvar dysplasia, and aortic coarctation.Reference Graham, Bradley and Shirali16–Reference Nelson, Rosella and Mahant19 Historically, trisomy 18 and trisomy 13 were labelled as “lethal” genetic diagnoses with death expected within 2 weeks of birth.Reference Nelson, Rosella and Mahant19–Reference Meyer, Liu and Gilboa21 Access to medical interventions, particularly corrective cardiac surgical interventions for a selected cohort, has more recently shifted the prognostic paradigm. Infants with trisomy 18 or trisomy 13 who underwent cardiac surgery between 2004 and 2015 had notably decreased in-hospital mortality reported in the Pediatric Health Information System Database compared to those infants who did not undergo cardiac surgery: 64% lower in trisomy 18 and 45% lower in trisomy 13.Reference Kosiv, Gossett and Bai22 Two decades of data from the Pediatric Cardiac Care Consortium revealed hospital survival rates of 100% for children with trisomy 13 (n = 11) and 86% for children with trisomy 18 (n = 21) who underwent cardiac surgery.Reference Graham, Bradley and Shirali16
The primary objective of this descriptive mixed methods study was to quantify perception of child and parent quality of life and family impact for children with trisomy 18 or trisomy 13 who had undergone definitive cardiac surgery. The study further aimed to explore the child’s functional status as assessed by parents and health care providers and to correlate functional status with family impact. The study described the child’s quality of life from parental qualitative narratives, the family’s experience accessing surgical interventions, parental hopes for their child, and parental advice for medical teams.
Patients and methods
This concurrent mixed methods study was approved by the Institutional Review Board as Protocol 889-18-EP (TraNSLOCATIONS = TRAveling Nationally So Loved One Can Access Trisomy Interventions Operatively in Nebraska). The sample method was a sequential sampling. All parents of children with trisomy 18 or trisomy 13 who had travelled out of state between May, 2017 and March, 2019 to access cardiac surgical interventions denied to them in their local care setting due to genetic diagnoses were invited to participate in the survey after live discharge to home. Study flow diagram is shown in Fig 1.

Figure 1. Concurrent mixed methodology approach for quality of life inquiry.
Patients were retrospectively enrolled from January, 2019 to May, 2019. Study notification occurred through an in-person conversation or telephone call from a study team member providing details on the study aims, methods, and the voluntary nature of participation. In-person or telephone informed consent then occurred. Questionnaire responses were collected using a SurveyMonkey© study database. The 40-item parental questionnaire consisted of a mixture of closed-ended questions with pre-determined categorical responses and open-ended narrative responses. The survey explored how and when parents received the trisomy diagnosis, reason for travel for cardiac surgery, family impact of travel, reflection on the surgical decision, quality of life narrative summary, parental hopes, and advice for medical teams.
Data collection from the medical chart included the child’s current age, genetic diagnosis, cardiac diagnosis, date of cardiac surgery, cardiac surgical procedure, and provider-rated functional status score at time of live discharge to home.
Three validated scales were utilised: PedsQL™ 4.0 Generic Core Parent Report for Toddlers Scales or the PedsQL™ Infant Scale, PedsQL™ 2.0 Family Impact Module, and the Functional Status Scale for Pediatric Hospitalization Outcomes. The 21-item PedsQL™ 4.0 Generic Core Parent Report for Toddlers Scale (age > 24 months) consists of the following dimensions: physical functioning, emotional functioning, social functioning, and school functioning. The 36-item (age <12 months) or 45-item (<24 months) PedsQL™ Infant Scales contain similar dimensions with the addition of physical symptoms and revision of school functioning to cognitive functioning. These scales have a minimum internal consistency reliability standard exceeding 0.70 per dimension.Reference Varni, Limbers and Neighbors23,Reference Desai, Zhou and Stanford24 These paediatric quality of life scales have previously been utilised in infants and children with CHD.Reference Raj, Sudhakar and Roy25–Reference Uzark, Jones and Slusher28 The 36-item PedsQL™ Family Impact Module is a measure of self-reported parental perceptions of physical, emotional, social, and cognitive functioning; communication; and worry. The PedsQL™ Family Impact Module further explores the impact of the child’s diagnosis on family daily activities and family relationships. In initial validation studies, PedsQL™ Family Impact Module scales demonstrated Cronbach’s coefficient alpha scores >0.82.Reference Varni, Sherman and Burwinkle29 The Functional Status Scale measured six domains of child function validated from newborn to adolescents: mental status, sensory functioning, communication, motor functioning, feeding, and respiratory status. Each domain receives a designated score from 1 (normal) to 5 (very severe dysfunction). The Functional Status Scale has been shown to be highly reproducible with the weighted total Functional Status Scale registering an intra-class correlation of 0.94.Reference Pollack, Holubkov and Glass30
Analysis process
Qualitative data were analysed using semantic content analysis,Reference Krippendorff31 including categorical strategies with Atlas.ti data organization. The open-text narrative data were broken down into smaller phrases with those phrases and then reorganised to produce quantifiable categories to facilitate a better understanding of the research question.
Statistical analyses were conducted using scale scores as the main outcome measure. Each PedsQL™ item was reverse-scored and linearly transformed to a scale of 0–100 (higher scores reflected better quality of life or better family function). A final summative score for the parent Functional Status Scale and provider discharge note Functional Status Scale was individually tallied, ranging from 6 to 30 with a higher number representing more severe dysfunction. A Bland–Altman analysis was conducted to assess for agreement in functional status scores between parents and providers using Carkeet’s exact confidence bounds for the upper and lower limits of agreement.Reference Bland and Altman32,Reference Carkeet33 Plots of the quality of life versus the functional status measures were decidedly non-linear; thus, Spearman’s rank correlation was used to capture the association. Group differences were compared using Wilcoxon Signed-Rank or Sum Rank tests as appropriate. Summary statistics reported were the mean, median, and interquartile range.
Results
A total of 10 family units were eligible for participation with offer of either one parent or both co-parents to complete the survey. All 10 family units completed the survey (100% response rate) with 4 families utilising both maternal and paternal survey completion and 6 families utilising only maternal responses. Fourteen surveys were completed for 10 children. Average age of the child was 10.6 months (range from 2 to 32 months). Two children were diagnosed with trisomy 13, one with mosaic trisomy 18, and the remaining 7 with full trisomy 18 as confirmed by karyotype. Cardiac diagnoses included ventricular septal defect (n = 8); atrial septal defect (n = 7); vulvar anomalies to include aortic, tricuspid, and pulmonary valve anomalies (n = 4); aortic coarctation (n = 2); double outlet right ventricle (n = 2); and Tetralogy of Fallot (n = 1), with complete cardiac correction performed in each case. Mean age at time of cardiac surgery was 2.7 months (range from 0.25 to 5.5 months) with average age at time of survey completion 11.3 months (range from 2 to 27 months).
Diagnostic disclosure
The trisomy diagnosis was made known to the parents prenatally in n = 6 and postnatally in n = 4 families, whereas the cardiac condition was known prenatally in n = 8 families. Communication of the trisomy diagnosis occurred in-person n = 6 and by telephone n = 4. Both parents were present to receive the trisomy diagnosis in n = 6 cases. Communication disclosing the diagnosis of trisomy was reported to be “not sensitive” by n = 6, neutral n = 7, and sensitive n = 1.
Access to cardiac surgery
Respondents travelled to access cardiac surgery for their children due to inability to access cardiac surgery in their home state with nine states were represented in the cohort. All respondents shared that they had received a message of their child not being a surgical candidate locally due to underlying genetics. Three of the ten children were reported by their parents to have been scheduled with a cardiac operation date but the scheduled surgery then having been cancelled by the local medical team once genetics were definitively resulted.
Implications of travel for cardiac surgery and decisional reflection
Respondents reported the following family impact due to travel for cardiac surgery: one parent (60%) or both parents (10%) leaving employment, sibling separation during hospitalisation (40%), grandparent distance during hospitalisation (100%), and parental units in separate states during hospitalisation (90%). Economic impact on the family was perceived as low by 3/14 parents (21%), neutral by 6/14 (43%), and high by 5/14 (36%). All parents responded “yes” when asked whether they perceived they made the right decision to travel out of state for their child to undergo cardiac surgery. In open-text responses, parents clarified that they have decisional affirmation due to survival (14/14 patients), growth and developmental progress (9/14 patients), improvement in heart failure symptoms such as feeding capacity or respiratory status (6/14 patients), child intrinsic worth (6/14 patients), and the child’s contribution as a family member (3/14 patients).
Quality of life
All parents selected “high” when given the option of rating their child’s quality of life as low, medium, or high. When asked to quantify the child’s quality of life using a visual analogue scale from 0 to 100 with 100 being the highest quality of life, the mean response was 92.7 with median 90 (range from 80 to 100).
Results from the PedsQL™ and Family Impact Module measures are available as Table 1. Fathers tended to give higher scores to their children than mothers for both quality of life and family wellness domains but without a statistically significant difference in parental ratings.
Table 1. Quality of life and family impact scale dimension results

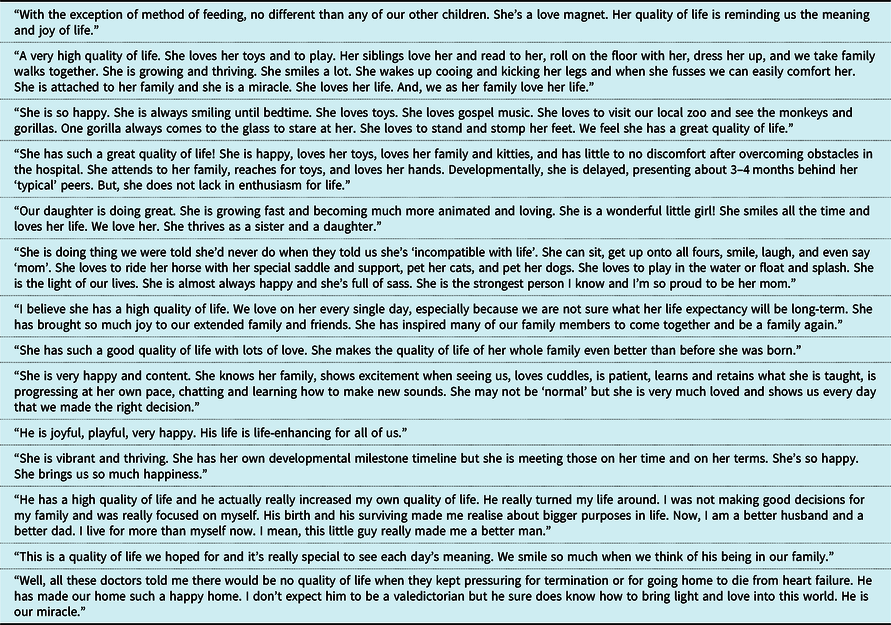
The meaning of quality of life was constructed in narrative free-text by parents as depicted in exemplary quotes in Table 2.
Table 2. Exemplary parental quotes depicting child’s quality of life
Functional status
A total of six children were on room air only, two used intermittent nasal cannula support, one had tracheostomy to room air, and one used tracheostomy and mechanical ventilation. All ten children had a gastrostomy tube for feeding support with eight children reported to be taking some food by mouth. Eight children were reported to have normal sleep–wake cycles. Five had suspected hearing loss. All communicated with vocalisations, expression, and gestures.
The Functional Status Scale instrument range is from 6 to 30, with a higher score associated with a worse functional status. In this cohort, mean Functional Status Scale ranking by parents was 11 (range from 9 to 14) and by paediatrician documentation day prior to discharge in medical record was 11.6 (range from 9 to 14). Correlation between parent and provider perspective on the child’s functional status was notably in agreement at 0.89 between parent and provider ranking of functional status. Five providers ranked the child’s Functional Status Scale higher than the parent. All four fathers rated their child’s functional status the exact same number as the provider Functional Status Scale ranking (100% agreement in paternal and provider Functional Status Scale rankings). A Bland–Altman plot depicting provider versus parent functional status agreement is provided as Fig 2.

Figure 2. Provider versus parent functional status agreement plot.
Correlation between the child’s functional status and family functioning was −0.26. Correlation between the child’s functional status and the parent’s self-reported quality of life was −0.62. A decrease in the child’s functional status correlated with a small but notable inverse impact to family function and negative impact to the parental caregiver’s quality of life. Summary of correlations is provided as Table 3.
Table 3. Correlations between functional status and outcome measures

Parental hopes and shared insight
In response to free-text inquiry on hopes for their child, parents depicted their hopes for their child in terms of allowing the child to reach his or her unique potential (n = 9 (65%)), experiencing joy and happiness (n = 7 (50%)), knowing love (n = 6 (43%)), inspiring others (n = 6 (43%)), having access to medical care in the future (n = 5 (36%)), and finding comfort in the family’s spiritual framework (n = 3 (22%)). Parents offered their insight and wisdom for medical teams in the context of these stated hopes as shown in Table 4.
Table 4. Parental advice for medical teams

Discussion
This concurrent mixed methodology study generated a descriptive summary of parental perspectives on quality of life, family impact, functional status, and hopes for children with trisomy 18 and trisomy 13 who have undergone heart surgery. Of interest, the scores assigned to children in this cohort were parallel to the proxy-ranked scores using the same scales when applied to children with CHD without genetic diagnoses after cardiac surgery.Reference Raj, Sudhakar and Roy25,Reference Berkes, Pataki and Kiss27,Reference Uzark, Jones and Slusher28 Quality of life is highly subjective, as is the impact of a child’s diagnosis or prognosis on a family’s function and well-being. The children in this study were perceived by their families to have high quality of life and valued life roles. This study included only a small, selected group of persistent parents who pursued and accessed cardiac surgery at another care centre after being refused cardiac surgery at their home centre, which does mean a real risk of a response bias.
The functional status of the children was noted to be congruent between parent and provider perspectives. Functional status had minimal impact on the parental perception of the child’s quality of life or parental perception of overall family wellness. In a prior study of 12 Pennsylvanian parents whose children with trisomy 18 had undergone congenital heart surgery, survey respondents both bereaved and actively parenting unanimously stated “that their child’s quality of life was improved by their specific treatment strategy, that the experience of the parents was enhanced, and that they would choose the same treatment course again.”Reference Davisson, Clark and Chin34 The majority of German mothers of children with trisomy 18 and trisomy 13 who survived longer than 3 months depicted their children as “friendly, happy, and peaceful” and were in favour of access to medical interventions for their children.Reference Kusztrich, Huseman and Garten35
This study was motivated by the study team’s own curiosity about the rising recent phenomenon of families reaching out for cardiac surgical interventions for their children and to try to understand the complex and even controversial phenomenon of offering care for these children. In sharing the findings from this study, our goal is that families with children with trisomy 18 and trisomy 13 diagnoses may share their perspectives on their child’s quality of life. Respondents in this study understood their children’s diagnosis and the prognostic implications of the trisomy 18 and trisomy 13 diagnoses but wanted their children to be offered “a chance” to “reach his or her potential.”
The average age at the time of corrective surgical intervention (<3 months) was notably young in our study. Our care centre has observed elevated pulmonary vascular resistance in this population younger, and more often, than children without these trisomy diagnoses. This pulmonary vascular resistance elevation has proven to have become irreversible in situations and at times where it would not have been expected to be so in other patients without these genetic aneuploidies. Due to this observation, we have opted for consideration of earlier surgical intervention. The trisomy 13 and trisomy 18 population’s cardiac needs are difficult to predict and only recently with a growing literature base of trends and patterns. The threshold consideration of earlier age for corrective surgical intervention has been part of our care model and family decision-making regarding potential timing of cardiac surgical intervention.
Limitations of this study include the lack of child reported outcomes, as our cohort was not of age or developmental ability to self-report. An additional limitation includes small sample size from a single-centre site, although the patients represent wide geographies. A “choice-supportive bias” exists as these selected patients may retrospectively ascribe positive attributes to the cardiac surgical pursuit and may demote the forgone options of not pursuing cardiac surgery. Additionally, providers working at an institution where the practice is to consider cardiac surgical intervention in review of each child’s unique comorbidities will be potentially biased towards the institution’s practice as compared to those providers working at centres with universal rules against cardiac interventions for children with these genetic conditions.
Strengths of the study include parallel mixed methods design which combined elements of qualitative and quantitative research approaches for the purpose of breadth of understanding and corroboration on parental perspective on a child’s quality of life, family impact, and parental hopes. Simultaneous integration of validated surveys and questionnaires with narrative inquiry fostered methodological triangulation. Use of both parental report and provider report for functional status offered a comparison summary in addition to the subjective quality of life metrics.
Conclusion
Cardiac surgical interventions for children with trisomy 21 were highly controversial until the late 1970s,Reference Champagne, Lewis and Gilchrist36 with a collaboration of both physiological outcomes-based data and family advocacy compelling a shift in care paradigms for children with Down syndrome. This paper adds to the growing body of literature on similar cardiac surgical considerations now for a carefully selected cohort of children with trisomy 18 and trisomy 13 with correctable cardiac lesions. Further research is warranted to investigate how the findings from this study may differ or concur with the same questionnaire for a local cohort, and whether the nature of persevering to pursue cardiac surgery even after being denied access in a home state setting impacts quality of life reporting. Future research warrants inclusion of bereaved family perspectives. Future studies would also include health care provider perspectives on reasons for providing or not providing cardiac surgical care options.
Cardiac surgical offerings may be considered in the context of an interdisciplinary care team’s shared exploration of the child’s comorbidities and the family’s understanding of overall prognosis, values, and decisional context.Reference Haug, Goldstein and Cummins37 Mixed methods research is recognised as transformative in capturing differing value commitments which can lead to dialogue across professional, personal, and ideological perspectives. This study adds to the recent dialogue by describing parental hopes and goals in pursuing cardiac surgical interventions. Clinical consideration of parental quality of life perceptions for children with trisomy 18 and trisomy 13 enables focus to expand beyond mere judgement of survival into enhanced child-centric, family-partnered care models.38
Financial Support
The authors have no financial relationships relevant to this article to disclose.
Conflicts of Interest
The authors have no conflicts of interest relevant to this article to disclose.
Ethical Standards
Ethical research standards were followed.
Table of Contents Summary
This concurrent mixed methodology study explores quality of life and family impact for children with trisomy 18 and trisomy 13 after travelling to access cardiac surgery.
What’s Known on This Subject
Over 80% of patients with trisomy 18 or trisomy 13 have congenital heart conditions. Despite growing evidence that definitive cardiac repair prolongs survival, surgical interventions remain controversial in the background of provider perspectives on survival and presumed quality of life.
What This Study Adds
This concurrent mixed methodology study describes the experiences of families who travelled to access cardiac surgery for a child with trisomy 18 or trisomy 13. Parental perceptions of quality of life, functional status, and family impact may inform cardiac care models.
Contributors’ Statement
Dr M.S.W. designed the study, supervised data collection, drafted the initial manuscript, and revised the manuscript. Mr J.R. designed the data collection instruments and collected data. Dr N.B. helped design and critically review the data collection instruments and assisted in data analyses. Dr C.W. and Dr H.H. carried out the initial data extraction or data analyses. Dr J.H. conceptualised the study and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.








