Introduction
Paramedics are a vital component of the Emergency Medical Services (EMS) workforce in the United States. 1 The paramedic level of certification allows these health professionals to be a key part of the comprehensive prehospital response that serves the public by bringing advanced care, interpretative and diagnostics capabilities, and critical thinking skills that allow complex judgements on critical care and transport decisions. This level of knowledge, skills, and attitudes demands a well-developed education and certification process. This includes training in an academic setting at nationally accredited paramedic programs, completion of a psychomotor competency portfolio, and confirmed competency through completion of the National Registry Cognitive and Psychomotor Examinations.
Providing and maintaining this high-quality paramedic education enriches both the quality of prehospital care provided by graduates and the quantity of candidates that can complete the certification process and ultimately join the workforce. 2,3 The paramedic education pipeline is particularly important in the context of concerns for on-going workforce shortages. Reference Snyder4 Characterizing and tracking paramedic education over time is a foundational step in understanding the current state of the field and ultimately planning for future workforce optimization.
The available data describing the state of paramedic education in the United States are limited. Some research has profiled individual metrics such as simulation availability and use Reference McKenna, Carhart, Bercher, Spain, Todaro and Freel5 and more subjective characteristics of a few high-performing programs. Reference Margolis, Romero, Fernandez and Studnek6 More complete profiles of paramedic education outside of the United States have been published, Reference Hou and Rego7 however, to date, a comprehensive profile of the demographics, characteristics, and resources of paramedic education programs is not available. The primary objective of this study was to form a descriptive profile of the demographic, educational details, and infrastructure for all paramedic programs in the United States in 2018 with self-reported metrics from the 2018 Committee on Accreditation of Educational Programs for the EMS Professions (CoAEMSP; Rowlett, Texas USA) program survey.
Methods
Study Design and Population
A retrospective, cross-sectional analysis was performed of the 2018 CoAEMSP annual survey, completed by all accredited United States paramedic educational programs from January through March of 2020. The inclusion criteria for this study were all Commission on Accreditation of Allied Health Education Programs (CAAHEP; Clearwater, Florida USA)-accredited and CoAEMSP-Letter of Review paramedic programs with enrolled students in 2018. Included in the annual report was the addition of educational program profile questions that characterize paramedic educational programs. This study was determined to be exempt by American Institutes of Research Institutional Review Board (Arlington, Virginia USA; EX00440).
Paramedic Programmatic Accreditation
Since 2013, paramedic education has occurred at nationally accredited educational institutions. Educational program accreditation ensures programmatic standardization and consistent quality across diverse programs. Reference Dickison, Hostler, Platt and Wang8,Reference Rodriguez, Crowe, Cash, Broussard and Panchal9 In the United States, graduation from a nationally accredited paramedic program is a de facto requirement for certification, as it has been a prerequisite for challenging the National Registry of Emergency Medical Technicians (NREMT) paramedic certification exam since 2013. 10 Accreditation for the 677 paramedic programs in the United States is recommended by the CoAEMSP and provided by the CAAHEP. The CAAHEP is the programmatic accreditor of over thirty allied health professions, of which the CoAEMSP is the largest Committee on Accreditation.
CoAEMSP Annual Report
The CoAEMSP Annual report satisfies CAAHEP Standard V.A.4 which states that all programs “must maintain, and make available to the public, current and consistent summary information about student/graduate achievement that includes the results of one or more of the outcomes assessments required in the CAAHEP Standards.” 11 Thus, there is a requirement of a 100% response rate for all paramedic educational programs (CAAHEP-accredited and CoAEMSP-Letter of Review) in the United States.
Data for the annual review are self-reported from each program. The CoAEMSP, as part of their mission, provides training for completion of the annual review including webinars, frequently asked questions, virtual office hours, and email contacts to facilitate accurate reporting of data points. Additionally, annual report completion is enforced by CoAEMSP with possible penalties including fines or probation for failure to complete in a timely manner.
The annual report is collected two years after completion of the educational year to ensure that all candidates have the requisite two-year certification testing period. The 2020 CoAEMSP Annual Review collected data for the paramedic program class of 2018, therefore data evaluated in this study focus on the data collected for the 2018 paramedic cohort.
Measurements
Data were collected on paramedic educational program characteristics including program cohort and class sizes, program training details, and infrastructure details. The number of classes or cohorts graduated by the program during the survey period were reported as continuous variables categorized into meaningful cut points (zero, one, two, three, and greater than four). Similarly, the total number of students enrolled in each program was a continuous variable and also categorized (one, two, three, and greater than four cohorts). The National Association of State EMS Officials (NASEMSO; Falls Church, Virginia USA) region was a categorical variable with each value corresponding to West, Western Plains, South, Great Lakes, and East regions. Program educational details were also evaluated, including total months to program completion and total hours of instruction, which were continuous variables. Specific to the goal of evaluating programs in the future, all questions were collaboratively updated and eight new questions were developed for the educational survey that assessed program budget, full-time faculty, duration in months, total program hours and hours dedicated to clinical, capstone, and field time, and access to simulation. Total hours of instruction was defined as all phases of paramedic educational program hours including didactic, laboratory, clinical, field experience, and capstone field internship. Hours of instruction were evaluated in detail for time (hours) dedicated to clinical (eg, in-hospital, clinics), field experience (not including capstone), and capstone field internship events. Program certification examination pass rates, first attempt pass rate, and cumulative third attempt pass rate were continuous variables.
Program infrastructure details were also evaluated. Total full-time faculty numbers were a continuous variable whereas degree or credential awarded was categorical (certificate, associate degree, bachelor’s degree). Paramedic educational programs were asked to report total annual budget within meaningful pre-defined categories (USD$1-$100,000; USD$100,001-$500,000; USD$500,001-$1,000,000; USD$1,000,001-$1,500,000; USD$1,500,001-$2,000,000; greater than USD$2,000,000; or prefer not to answer). The highest level of available simulation infrastructure was evaluated as a categorical variable: task trainer, simple manikin, intermediate manikin, advanced manikin, and virtual reality.
Additionally, a Resource Assessment Matrix (RAM) 12 was evaluated to measure availability of necessary resources. This measure synthesizes the results of two separate surveys conducted by programs that assess resources available to both students and program representatives. This is scored across ten different parameters, with a corrective plan necessary for any scores that are below the established benchmark. The RAM requirements were dichotomized as meeting the benchmark or not.
Analysis
Inclusion criteria for this evaluation were all programs that started with students enrolled in a program cohort in 2018. As part of preparation of the self-reported data, any text or range responses to questions that asked for numbers (for example, a response of “240-280” or “at least 300” in response to “How many hours of instruction…?”) were removed. If a number was preceded by a qualifier such as a tilde (“∼”) or the word “approximately,” the qualifier was removed and the value converted to a number. If a response was blank or ambiguous, it was excluded from analysis.
Descriptive statistics were calculated (median, interquartile range [IQR], and frequency expressed as a percentage, as appropriate). Statistical analysis was performed with the Stata 15 version statistical package (Stata Corp; College Station, Texas USA).
Results
A total of 677 programs submitted data (100% response rate). Of these, 626 met inclusion criteria by enrolling at least one student during 2018, representing 17,422 students. Table 1 lists paramedic educational program demographics including class size, structure, and geographic region. The majority of programs graduated one cohort per year. While the range of program annual student enrollment varied greatly from zero to 362, the vast majority of programs maintained small sizes (mean 18 students [IQR 12-30]). The greatest number of programs geographically were noted in the South NASEMSO region. The majority of programs did not have satellite campuses, but for those who did, most were located in the South NASEMSO region.
Table 1. Size, Structure, and Distribution Reported to CoAEMSP for Programs Graduating Cohorts in 2018

Abbreviations: CoAEMSP, Committee on Accreditation of Educational Programs for the EMS Professions; NASEMSO, National Association of State EMS Officials.
Paramedic program educational characteristics were also evaluated. Overall program duration and instructional hours showed a relatively narrow distribution. The median program duration was 12 months (IQR 12-16) and with median total hours of instruction being 1,174 (IQR 1069-1304; Table 2). When examined more closely, the total clinical experience time represented 19% of total instruction time, which includes both field experience and capstone field internship experiences. Overall, programs reported a 77% median first pass rate on certification examination and an 89% median cumulative third attempt pass rate.
Table 2. Program Training Details and Associated Testing Outcomes Reported to CoAEMSP for Programs Graduating Cohorts in 2018

Abbreviation: CoAEMSP, Committee on Accreditation of Educational Programs for the EMS Professions.
Finally, the infrastructure that supports program educational curricula, including available resources, were tabulated in Table 3. Programs reported a median of two full-time faculty (IQR 1-3) members responsible for teaching students. Degrees that could be conferred by programs were primarily certificate (90% of total programs) or associate degrees (55% of total programs) with only two percent able to confer bachelor’s degrees at graduation. The majority of programs (80%) had annual operating budgets below USD$500,000. For programs with an annual budget below USD$100,000 (34% of programs), annual enrollment was approximately 14 students (IQR 9-21). Simulation access was also assessed with nearly all (100%) programs reporting simple task trainers and 84% of programs investing in advanced simulation manikins. Of all the paramedic educational programs, 78% reported meeting 80% of RAM requirements.
Table 3. Infrastructure Details Reported to CoAEMSP for Programs Graduating Cohorts in 2018
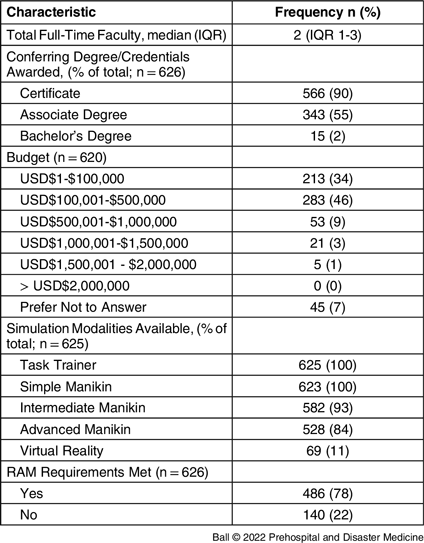
Abbreviations: CoAEMSP, Committee on Accreditation of Educational Programs for the EMS Professions; RAM, Resource Assessment Matrix.
Discussion
Paramedics are a critical component of the prehospital health care system and ensuring quality in their initial education is important to maintain the EMS workforce. In this evaluation, paramedic educational program profile characteristics were presented from the CoAEMSP annual survey with a 100% response rate. This profile defines, for paramedic educational programs, the demographics, training details, and infrastructure supporting the preparation of new paramedic student graduates. These data will allow evaluations of how programs change in the coming years, particularly with the onset of the COVID-19 pandemic that will be represented in the 2020 annual report.
One challenge in benchmarking for paramedic educational programs is that there is a paucity of current data concerning the true demography of these EMS educational programs. Early work completed before mandatory national accreditation focused on innate challenges associated with paramedic program education. Reference Pointer13–Reference Fernandez, Studnek and Cone17 Margolis, et al identified high-performing paramedic programs and described their subjective characteristics, such as maintaining high-level entry requirements and fostering a culture that values continuous review and improvement. Reference Margolis, Romero, Fernandez and Studnek6 This focus was amplified by the community direction toward national accreditation as a first step in improving paramedic education. Reference Dickison, Hostler, Platt and Wang8,Reference Rodriguez, Crowe, Cash, Broussard and Panchal9,18 While previous research has demonstrated that accreditation is an important step in optimizing paramedic education, Reference Dickison, Hostler, Platt and Wang8,Reference Rodriguez, Crowe, Cash, Broussard and Panchal9 further optimization may be necessary. However, educational data post-accreditation are critical to understanding the new barriers faced by paramedic educational programs.
In this study, a thorough evaluation was conducted of the time to course completion and time of focused instruction (Table 2). Paramedic programs completed education in one year with graduates receiving approximately 1,175 hours of training, which agrees with previously available information that suggested an average of 1,000-1,300 total hours. Reference Pollak, Edgerly, McKenna and Vitberg19 Programs reported that 19% of educational hours were in the clinical setting. It is unclear what the impact of increased or decreased clinical experience may be on paramedic student performance. Reference Page, Brazelton, Kokx, Jennings and Williams20 This became a critically important consideration during the SARs-CoV2 pandemic where programs transitioned from clinical settings due to these being unavailable. Reference Amato21 One suggested solution was a transition to increased simulation experience. Reference Mitchell22 As noted in the SUPER study, paramedic educational programs have significant access to simulation in a large range of intricacy. Reference McKenna, Carhart, Bercher, Spain, Todaro and Freel5 Similarly in this evaluation, significant availability of simulation platforms for paramedic students was noted (Table 3). However, it is unclear what the impact on certification success and performance of paramedic graduates may be with either increased online education or simulation-based training. Future research will be necessary to evaluate these paradigms.
One of the more remarkable findings of this analysis was the relatively low rate (78%) of programs being sufficiently resourced to satisfy RAM requirements, meaning that nearly one in four paramedic educational programs in the United States is not appropriately resourced. While the survey RAM includes multiple individual measures of resource availability, this measure provides a holistic view of program resource access. Though it was noted that most paramedic educational programs have small annual enrollments with low numbers of dedicated faculty and low operating budgets (below $500,000), the impact of these considerations on resource availability is unclear. Of note, while other survey data are provided by program administration, the data from which the RAM is calculated are provided by students and educators, a group with the potential to be fewer steps removed from the actual resources.
Limitations
This analysis was conducted retrospectively and based on self-reported survey data. Unlike most surveys, however, completion was mandatory thus the response rate was high and missingness of outcome variables low. One of the issues with the self-reported data was the potential for inappropriate responses, such as reporting data ranges when a number is requested. Further, recall bias is likely present, with programs reporting 2018 data in 2020, and misclassification bias due to the nature of self-reported data. Future evaluations using annual report data should take this into account in survey design.
Conclusion
The CoAEMSP annual survey profile provides a comprehensive description of paramedic educational programs in the United States including demographics, educational details, and infrastructure supporting the preparation of new paramedic student graduates. The majority of paramedic educational programs graduate small class numbers, with programs spanning approximately one year. These programs are supported by relatively low budgets, a low number of dedicated faculty, and excellent access to simulation. Analysis of the RAM score reveals that nearly one in four programs are under-resourced. Future research should focus on developing trends as well as investigating how and why characteristics of paramedic educational programs correlate with different measures of programs success.
Conflicts of interest
The authors declare none.






