Introduction
Children are often thought to be more prone to tympanic membrane graft failure than adults. The reported success rate of tympanoplasty in children ranges from 35 to 94 per cent.Reference Caylon, Titiz and Falcioni1, Reference Uyar, Keles, Koc, Oztruk and Arbag2 Factors contributing to failure include young age, high frequency of otitis media and upper respiratory tract infections, immature immune system, unpredictable eustachian tube function, status of the contralateral ear, size and condition of the perforation (i.e. dry or draining), surgical technique, and graft type.Reference Bluestone, Cantekin and Douglas3–Reference Vrabec, Deskin and Grady6
Some otological surgeons advocate early surgery (on children older than four years) to correct anatomical defects and improve hearing.Reference Glasscock7 Others advise delaying surgery until puberty.Reference Goodman and Wallace8, Reference Ophir, Porat and Marshak9 Proponents of early intervention frequently cite the adverse effects of hearing loss on speech and language development.Reference Rizer10 Delay may also increase the potential risk of cholesteatoma formation and ossicular chain erosion.Reference Rizer11
The principal aims of tympanoplasty are to create an intact tympanic membrane and to restore functional hearing.Reference Rizer10 The choice of operative technique and material for paediatric myringoplasty and tympanoplasty remains controversial.Reference Gross, Bassila, Lazar, Long and Stagner4 A variety of techniques have been described and are currently used, including overlay, underlay, sandwich, pegging, rosette and plugging.Reference Gibb and Chang12–Reference Pfattz and Griesemer14 In addition, a wide variety of grafting materials have been used, in various autografts, homografts and allografts.Reference Rizer10, Reference Rizer11 At the present time, autografts of temporalis fascia, veins, areolar tissue, periosteum and perichondrium, and involving either the overlay or underlay technique, appear to be most widely used.Reference Ozbek, Ciftci, Tuna, Yazkan and Ozdem15–Reference Page, Charlet and Strunski17
Temporalis fascia's superior qualities, ready availability in the operative field and ideal handling have made it the standard for tympanic membrane grafting since its introduction in the 1960s.Reference Rizer10 GoodhillReference Goodhill18 used tragal perichondrium and cartilage for grafting in 1967, with similar results to others using fascia. However, although acceptable, this material has not been widely used.Reference Milewski, Giannakopoulos, Muller and Schon19
Each graft has its own, well known advantages and disadvantages. Some authors have suggested that soft tissue is an uncertain material with which to repair total perforations, especially those close to the annular region, and that more rigid transplant materials are needed.Reference Milewski, Giannakopoulos, Muller and Schon19
A ‘ring’ graft is a modified cartilage–perichondrium composite graft consisting of a peripheral, ring-shaped piece of cartilage attached to a sheet of perichondrium. This graft type has the advantages of cartilage–perichondrium composite grafts, perichondrial grafts and temporalis fascia grafts, but without their disadvantages.Reference Mansour, Askar and Albirmawy20
This study aimed to evaluate both the anatomical and functional results of primary type one tympanoplasty with cartilage–perichondrium composite ring graft technique in paediatric patients, and to compare the results with those of primary type one tympanoplasty using temporalis muscle fascia in children with similar middle-ear pathology and pre-operative hearing levels.
Patients and methods
Patient population and evaluation
A retrospective chart review was performed to identify all children who had undergone type one tympanoplasties using either a cartilage–perichondrium composite ring graft or temporalis muscle fascia, performed by the same surgeon (OAA) in the otolaryngology department, Tanta University Hospital, from January 2004 to October 2008. Data were obtained from out-patient appointment medical records and surgical reports.
Inclusion criteria were: (1) a dry, central, subtotal or total perforation (any size); and (2) conductive deafness with an air–bone gap not exceeding a mean of 25 dB. All cases were secondary to otitis media, tympanostomy tube placement or trauma. Any source of recurrent upper respiratory tract infection (e.g. sinusitis, allergic rhinitis or adenotonsillitis) was managed medically and/or surgically at least one month before surgery.
Cases with conductive hearing loss of more than 25 dB, or mixed hearing loss, were excluded. Patients with concomitant mastoidectomy, ossiculoplasty, atelectasis or any history of previous ear surgery (except for tympanostomy tubes) were also excluded. Patients older than 15 years and younger than five years at the time of surgery were likewise excluded, in order to obtain two cohort groups of similar age distribution.
All children received at least one year's follow up after surgery.
During the first years of the study period, myringoplasty with temporalis fascia was performed more frequently, whereas the ring graft was used more frequently during the later years. The ring graft group included 46 children and the temporalis fascia group 49. Six patient in the ring graft group and seven in the fascia group did not have adequate follow-up data and were thus eliminated from analysis, leaving 40 patients in the ring graft group and 42 in the fascia group.
Because the study aimed to evaluate the anatomical and audiological outcomes for the two graft materials, the author tried to eliminate any factor that might affect the surgical outcome (e.g. ossiculoplasty, cholesteatoma or neural deafness), in order to decrease bias.
The children's pre- and post-operative audiometric results were analysed according to the 1995 American Academy of Otolaryngology–Head and Neck Surgery guidelines.21 Surgical results were evaluated by comparing patients' pre- and post-operative pure tone average (PTA) air–bone gaps (ABGs) (at 0.5, 1, 2 and 3 kHz) and speech reception thresholds, and their post-operative tympanic membrane findings. Patients with one or more years of follow up, who had undergone audiometric testing in the first post-operative year, were included in the study.
Informed consent for surgery was obtained from all the patients' parents.
Surgical technique
All patients were operated upon under general anaesthesia by the same surgeon (OAA). The post-auricular approach was used in all cases.
In the ring graft group, harvesting and modification of the tragal cartilage and perichondrial material was performed as previously described by the author and colleagues.Reference Mansour, Askar and Albirmawy20 The perichondrium was left attached to the concave posterior side of the cartilage, leaving the anterior perichondrium and the free edge of the tragal cartilage intact, to avoid tragal deformity. The graft was approximately 12–15 mm in diameter. A circular piece of cartilage was cut from the centre of the graft using a number 15 scalpel blade or the sharp edge of an ear speculum (Figure 1a). The cut, circular piece of cartilage was removed with gentle dissection. Care was taken to avoid laceration of the attached perichondrial sheet. In this way, it was possible to obtain a perichondrial sheet with attached cartilage ring frame. The cartilage ring was trimmed according to the periphery needed, taking care to preserve a good rim of firm, elastic, intact cartilage (2–3 mm), so that the size of the graft would be a little larger than the size of the membrane tensa (Figure 1b).
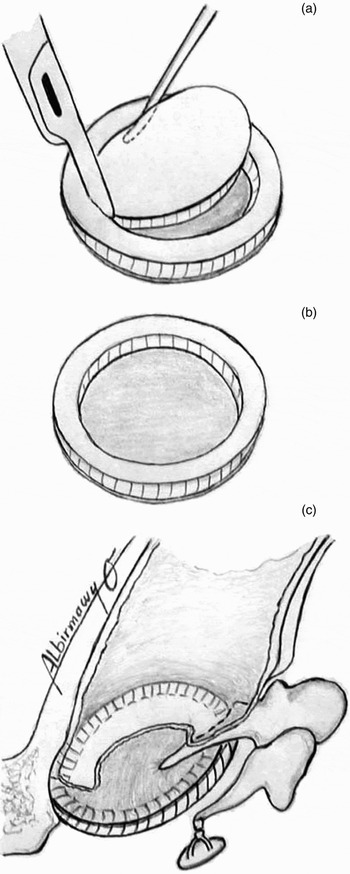
Fig. 1 (a) Cutting and dissecting the central cartilaginous disc from the harvested cartilage–perichondrium composite tragal graft. (b) The ‘ring’ graft before implantation, with its peripheral cartilaginous rim and attached perichondrial sheet. (c) The implanted underlay ring graft, with the cartilaginous ring facing medially and the perichondrium facing laterally.
After preparation of the middle ear and tympanic membrane, the myringoplasty and tympanoplasty proceeded as follows. The ring graft was used as an underlay with its cartilage facing medially and perichondrium facing laterally, covered by the handle of the malleus, the tympanic membrane remnant and the posterior tympanomeatal flap. Care was taken to place the cartilaginous ring of the graft well under the annulus, or in the bony annulus if the fibrous annulus was absent or removed. In this way, the graft maintained its exact site without the need to fill the middle-ear cavity with Gelfoam®, and with the transparent perichondrium in a central position (Figure 1c).
In the temporalis fascia group, the graft was harvested from the ipsilateral deep temporalis muscle fascia, and dehydrated. After filling the middle-ear cavity with supporting Gelfoam, the graft was placed medial to the handle of the malleus, the tympanic membrane remnant, the anteroinferior annulus and the posterior tympanomeatal flap.
In both groups, Gelfoam was used to pack the external ear canal lateral to the reconstructed tympanic membrane.
Post-operative care and outcome measures
The children were discharged the next morning on a 10-day course of oral amoxicillin-clavulanic acid.
At the end of the 10th post-operative day, the Gelfoam was sucked from the external ear canal to avoid a granulomatous reaction. Three weeks later, the children were encouraged to start doing gentle Valsalva manoeuvres. After the end of the eighth week, if hearing results were available and the tympanic membrane looked clear, the patient was followed up every three months for at least one year.
The main outcome measures used were graft success rate and hearing improvement level.
Successful graft acceptance was defined as full, intact healing of the tympanic membrane without perforation, retraction, lateralisation or anterior blunting, for at least 12 months post-operatively.
Assessment of hearing improvement was based on the most recent audiogram available. Results were analysed by comparing pre- and post-operative PTA ABGs at 0.5, 1, 2 and 3 kHz. If the threshold at 3 kHz was not available in the audiogram, the mean of the 2 and 4 kHz results was used as an estimated 3 kHz threshold. The ABG change was defined as the difference between the pre- and post-operative ABGs. An ABG closure to within 20 dB was considered successful. Pre- and post-operative speech reception thresholds were also recorded and analysed.
Statistical analysis
Data were collected, coded and analysed using the Statistical Package for the Social Sciences version 12 and Windows XP software.
Means and standard deviations were obtained from the measured data. An analytical and statistical comparison of recorded data was performed using the independent group t-test for the matching variables. A paired-sample t-test was used to compare the difference in means. The α level was set at 0.05. A one-tailed test for significance was used; p < 0.05 was considered statistically significant and p < 0.001 highly statistically significant.
Results
A total of 82 children younger than 16 years and older than four years was included in this study. The ring graft group comprised 40 children and the temporalis fascia group 42. The children's ages ranged from five to 15 years, with a mean age of 12.70 ± 2.30 years in the ring graft group and 11.40 ± 2.91 years in the fascia group. There were 27 (67.5 per cent) boys and 13 (32.5 per cent) girls in the ring graft group, and 26 (61.9 per cent) boys and 16 (38.1 per cent) girls in the fascia group.
The follow-up period ranged from 12 to 39 months, with a mean of 16.54 ± 8.61 months for the ring graft group (range 12–36 months) and a mean of 18.22 ± 7.94 months for the fascia group (Table I).
Table I Patient characteristics and follow up

* n = 40; †n = 42. SD = standard deviation; y = years; FU = follow up; mths = months
The indication for surgery in all cases was dry perforation. Patients' perforation sizes were as follows: less than 50 per cent in 19 (47.5 per cent) cases in the ring graft group and 22 (52.38 per cent) in the fascia group; 50–75 per cent in nine (22.5 per cent) in the ring graft group and 11 (26.19 per cent) in the fascia group; subtotal in seven (17.5 per cent) in the ring graft group and five (11.90 per cent) in the fascia group; and total in five (12.50 per cent) in the ring graft group and four (9.52 per cent) in the fascia group. The difference in perforation size between the two groups was not statistically significant (p > 0.05; Table II).
Table II Pre-operative tympanic membrane perforation size

Grp = group
The graft success rate in ring graft patients was 95 per cent. Only two cases developed post-operative perforation. One of these perforations was accepted as a primary failure of grafting, occurring within six months of surgery, while the other child had a delayed perforation secondary to acute otitis media. Both these perforations were located posterosuperiorly. The first perforation was less than 50 per cent of the tympanic membrane size, and the second one was completely healed by conservative treatment. There was no graft retraction, lateralisation or anterior blunting in the ring graft group.
The graft success rate in the fascia group was only 76.2 per cent. Early post-operative perforations were detected in three cases, and delayed perforations in another three cases during the follow-up period. Most of these perforations were located anteriorly and were less than 50 per cent of the tympanic membrane size, except in one case. None of these perforations responded to conservative treatment. Two fascia group cases developed extensive retraction, while another graft was lateralised and a further one showed anterior blunting.
The difference in graft acceptance rates between the two groups was statistically significant (p = 0.006; Table III).
Table III Post-operative graft success rate

The p value is related to the comparison of the graft success rate between the ring group and fascia group. Grp = group
All 40 patients in the ring group had successful hearing results, with an ABG within 20 dB; 16 had an ABG within 10 dB. In contrast, in the fascia group, only 30 patients had successful hearing results, with an ABG within 20 dB; 9 had an ABG within 10 dB.
Changes in ABG and speech reception threshold were noted for all children.
In the ring graft group, the mean pre-operative ABG was 26.62 ± 1.73 dB and the mean post-operative ABG 10.95 ± 2.12 dB; this difference was highly statistically significant (p < 0.001). The mean pre- and post-operative speech reception threshold scores were respectively 34.73 ± 3.31 and 12.39 ± 3.11 dB (Table IV), also a highly statistically significant difference (p < 0.001). Thus, in this group the mean ABG decreased by 14.67 ± 2.10 dB and the mean speech reception threshold score improved by 22.34 ± 3.58 dB.
Table IV Pre- and post-operative PTA-ABG and speech reception threshold: ring group

PTA-ABG = pure tone average air–bone gap; SD = standard deviation; pre-op = pre-operative; post-op = post-operative
In the fascia group, the mean pre-operative ABG was 25.98 ± 2.21 dB and the mean post-operative ABG 12.73 ± 8.97 dB, a highly statistically significant difference (p < 0.001). The mean pre- and post-operative speech reception threshold scores were respectively 32.33 ± 2.74 and 14.54 ± 9.65 dB (Table V), also a highly statistically significant difference (p < 0.001). Therefore, in this group the mean ABG decreased by 13.25 ± 9.57 dB and the mean speech reception threshold score improved by 17.79 ± 9.98.
Table V Pre- and post-operative PTA-ABG and speech reception threshold: fascia group

PTA-ABG = pure tone average air–bone gap; SD = standard deviation; pre-op = pre-operative; post-op = post-operative
Comparison of the two groups' audiological results did not reveal any statistically significant difference (p > 0.05). These results are presented in Table VI.
Table VI Audiological outcomes: comparison between groups

SD = standard deviation; pre-op = pre-operative; post-op = post-operative; PTA-ABG = pure tone average air–bone gap; SRT = speech reception threshold
Discussion
The goal of tympanoplasty is to reconstruct the tympanic membrane and the sound-conducting mechanism in a long-lasting way. Since the introduction of this procedure in the 1950s by ZoellnerReference Zoellner22 and Wullstein,Reference Wullstein23 numerous graft materials and placement techniques have been described to reconstruct the tympanic membrane.Reference Rizer10 Temporalis muscle fascia and perichondrium remain the most frequently used materials, with a primary tympanoplasty closure rate of approximately 90 per cent.Reference Dornhoffer24, Reference Gerber, Mason and Lambert25 However, in paediatric populations (which have a high frequency of upper respiratory tract infection, eustachian tube dysfunction and immune system immaturity, together with a greater incidence of advanced middle-ear pathology, retraction pockets, atelectasis and revision tympanoplasty), fascial and perichondrial grafts have been observed to undergo atrophy and subsequent failure in the post-operative period, regardless of placement technique.Reference Buckingham26–Reference Gamra, Mbarek, Khammassi, Methlouthi, Quini and Hariga28 These results have encouraged otologists to use harder and more compatible graft materials.Reference Kerr, Byrene and Smyth29, Reference Mills, Booth and Kerr30
Graft cartilage harvested from the concha or tragus is easy to obtain, thick, hard, resistant to resorption and retraction, and convenient for shaping according to the size of the perforation and the nature of the middle-ear pathology.Reference Dornhoffer and Cartilage31 However, the risk of significant conductive hearing loss following cartilage tympanoplasty has always hampered routine acceptance of cartilage as a graft material.Reference Dornhoffer32
In an attempt to increase the advantages of the cartilage–perichondrium composite graft while avoiding its disadvantages, Mansour et al. Reference Mansour, Askar and Albirmawy20 modified this graft to what is now termed a cartilage–perichondrium composite ring graft. This was done by cutting and dissecting most of the central cartilaginous disc, leaving the graft with a peripheral cartilaginous ring (2–3 mm) attached to a unilateral firm, elastic, transparent sheet of perichondrium. In these authors' series, tympanic membrane perforations were completely healed using cartilage–perichondrium composite ring grafting, in 18 cases of non-cholesteatomatous, chronic, suppurative otitis media with different perforation sizes.
From 2004 onward, the current author has used ring grafts for all types of tympanoplasty, including high risk cases such as paediatric tympanoplasty, revision procedures, tympanosclerosis, atelectasis, large perforations and ossiculoplasty. Although the ring graft had generally been suggested for more difficult cases, there were no clinical studies comparing its results with those of temporalis fascia grafting, for childhood tympanoplasty. Hence, the current study aimed to evaluate and compare the anatomical and audiological outcomes of paediatric type one tympanoplasty, using ring grafting as a new technique and temporalis fascia grafting as the standard procedure. An attempt was made to eliminate any other factor that may affect outcomes (e.g. ossiculoplasty, cholesteatoma, discharging ears or neural deafness), in order to decrease bias.
Based on the hypothesis that a thick, rigid cartilage disc can be associated with considerable conductive hearing loss due to reduced compliance, it could be postulated that modifying the cartilage may lead to better anatomical and audiological outcomes. A number of cartilage techniques and modifications have been described: the cartilage palisade tympanoplasty and Heermann techniques,Reference Amedee, Mann and Riechelman33–Reference Heermann35 composite autograft shield,Reference Milewski27, Reference Duckert, Müller, Mkielski and Helms36, Reference Cavaliere, Mottola, Rondinelli and Iemma37 perichondrium island flap,Reference Dornhoffer24, Reference Gerber, Mason and Lambert25, Reference Adkins38 cartilage butterfly inlay graft,Reference Eavey39, Reference Mauri40 ‘crown cork’ technique,Reference Hartwein, Leuwer and Kehrl41 cartilage mosaic tympanoplasty,Reference Abou Mayaleh, Heshiki, Portmann and Negrevergne42 cartilage wheel,Reference Shin, Lee, Kim and Lee43 cartilage slicing,Reference Atef, Talaat, Moseleh and Safwat16, Reference Zahnert, Huttenbrink, Murbe and Bornitz44 and cartilage reinforcement.Reference Uslu, Tek, Tatlipinar, Kilicarslan, Durmus and Ay Ogredik45 Either tragal or conchal cartilage can be used – the choice depends on the surgeon's preference.Reference Gerard, Decat and Gersdorff46, Reference Puls47
These articles have described cartilage grafting, and/or its modification, alone or in comparison with traditional grafting materials, especially temporalis fascia, and have reported high tympanic membrane closure rates of 91.5,Reference Milewski27 92,Reference Duckert, Müller, Mkielski and Helms36 9638 and 100 per cent.Reference Dornhoffer24, Reference Gerber, Mason and Lambert25, Reference Uzun, Caye-Thomasen, Anderson and Tos48, Reference Anderson, Caye-Thomasen and Tos49
This current study further elaborates on the above results, by demonstrating that overall graft acceptance and hearing improvement after ring graft myringoplasty were comparable to those for fascia grafting. However, it should be noted that most of the previous studies were performed on cholesteatomatous ears, with or without ossiculoplasty. Anatomical and functional results can be affected not only by the graft material but also by middle-ear pathology and ossicular chain reconstruction. The current study included only children with dry, non-cholesteatomatous ears and an intact ossicular chain. Children in both graft groups were age-matched and had similar perforation sizes and middle-ear pathology; they therefore represented a defined and homologous patient population. Thus, their hearing loss was most probably due to tympanic membrane perforation, and this enabled the surgeon to make precise conclusions with respect to the operative technique. The graft success rate after at least one year of follow up was 95 per cent for the ring graft group and 76.2 per cent for the fascia group; this difference was statistically significant. Moreover, the delayed post-operative perforation encountered in the ring graft group healed with conservative treatment, while this approach failed in cases of post-operative perforation in the fascia group. These graft success rates thus favour the use of ring grafts in children. The adequate mean follow-up time in both groups allowed the author to evaluate the stability of both grafting materials.
In some reported series,Reference Koch, Friedman, McGill and Healy5, Reference Vrabec, Deskin and Grady6 success was defined as finding an intact graft in the proper location at the annulus ‘in addition to being intact’ at the last examination. From an acoustic point of view, graft lateralisation, retraction, and/or blunting have the same effect as perforation. Graft lateralisation or blunting could be caused by:Reference Perkins and Bui50 (1) bleeding in the middle ear, displacing the graft laterally; (2) incorrect positioning of the graft onto the malleus and bony sulcus; (3) post-operative graft slippage from the umbo, during Gelfoam removal or Valsalva manoeuvre; (4) the patient's inherent healing process, with canal skin contraction resulting in lateral pulling of the graft.
In this study, no post-operative retraction, lateralisation or blunting was observed in the ring graft group. However, in the fascia group the tympanic membrane was retracted in two cases, lateralised in one case and blunted anteriorly in another case. The substance and design of the ring graft enabled it to be stable, firm yet malleable, and transparent. The handle of the malleus supported the graft perichondrium by resting over it at the umbo, while the tympanic and bony annulus fit the peripheral cartilaginous ring circumferentially, acting like a natural drum. This eliminated the necessity of placing Gelfoam in the middle ear to support the ring graft position, as required with other methods (including temporalis fascia grafting). The absence of amino acid chains from disintegrating middle-ear Gelfoam would be expected to reduce the risk of middle-ear infection in the early post-operative period, and to promote earlier aeration of the middle-ear space. This, in combination with the early removal of the external canal Gelfoam, maximised the restoration of normal middle-ear and auditory canal physiology, and probably enhanced the ultimate anatomical and functional results.
In 2000, Zahnert et al. Reference Zahnert, Huttenbrink, Murbe and Bornitz44 used laser Doppler interferometry to study cadaver cartilage, and concluded that the ideal thickness of graft cartilage, from an acoustic point of view, was 0.5 mm, compared with the 0.7–1 mm thickness obtained at harvest. Atef et al. Reference Atef, Talaat, Moseleh and Safwat16 analysed the effect of cartilage disc thickness on hearing results after perichondrium–cartilage island flap tympanoplasty, and concluded that slicing the cartilage to half its normal thickness added to the technical difficulties of the procedure without making a significant difference to the hearing gain. In the current study, the use of a ring graft solved this problem, by removing most of the central cartilaginous disc while keeping a narrow (2–3 mm) peripheral rim with its normal harvest thickness. This enabled rapid healing and no delay in hearing improvement. After healing, the ring graft was similar to a normal tympanic membrane in its conical shape and transparency, facilitating the diagnosis of any developing middle-ear pathology such as a middle-ear effusion or cholesteatoma.
Although one might anticipate a significant conductive hearing loss with a rigid, thick, healed tympanic membrane created using cartilage in a tympanoplasty, surprisingly, there is no great evidence in the literature to support this notion.Reference Dornhoffer and Cartilage31, Reference Dornhoffer32 Gerber et al. Reference Gerber, Mason and Lambert25 compared cartilage with fascia for tympanoplasty, and found no significant difference in hearing between the two groups. DornhofferReference Dornhoffer24 obtained the same results after comparing cartilage with perichondrium. MilewskiReference Milewski27 reported a post-operative average ABG of <30 dB in 92.4 per cent and <10 dB in 43.6 per cent of 197 patients undergoing tympanoplasty using cartilage. Duckert et al. Reference Duckert, Müller, Mkielski and Helms36 reported excellent hearing results with cartilage: closure of the ABG to within 10 dB was achieved in 87, 73 and 70 per cent of type I, II and III tympanoplasties, respectively. Gamra et al. Reference Gamra, Mbarek, Khammassi, Methlouthi, Quini and Hariga28 confirmed audiometric hearing improvement in their series: good functional results (ABG ≤ 20 dB) were observed in 89 and 82.8 per cent of the cartilage and fascia groups, respectively, without a statistically significant difference. Thomasen et al. Reference Thomasen, Anderson, Uzun, Hansen and Tos51 compared cartilage palisades with fascia for tympanic membrane reconstruction after surgery for sinus or tensa retraction cholesteatoma in children, and reported that the former grafting technique appeared superior with respect to prevention of long-term tympanic membrane retraction and excellent long-term hearing results. Ozbek et al. Reference Ozbek, Ciftci, Tuna, Yazkan and Ozdem15 used the same technique in type one tympanoplasty in children, and concluded that palisade modification yielded good anatomical and functional results, with a 100 per cent acceptance rate, compared with fascia (70.2 per cent acceptance), and almost the same audiological results. Uslu et al. Reference Uslu, Tek, Tatlipinar, Kilicarslan, Durmus and Ay Ogredik45 inserted a piece of cartilage as a reinforcement under the anterior border of a temporalis fascia graft in cases of high risk perforation, and found that this technique greatly increased the rate of tympanic membrane closure, without affecting audiometric results. Shin et al. Reference Shin, Lee, Kim and Lee43 introduced a wheel cartilage–perichondrium composite graft with one stage ossiculoplasty; their patients' mean ABG decreased from 30.0 dB pre-operatively to 24.0 dB post-operatively, and the mean air conduction threshold from 47.3 dB pre-operatively to 35.7 dB post-operatively. Cavaliere et al. Reference Cavaliere, Mottola, Rondinelli and Iemma37 reported their experience with tragal cartilage fashioned as a shield with a V-shaped notch to accommodate the malleus handle, in tympanoplasties in 306 adult patients, and recommended its use in less severe middle-ear disorders, in which the functional outcome was more essential.
In this study, the difference between pre- and post-operative audiometric parameters (i.e. PTA-ABG and ABG change, at 0.5, 1, 2 and 3 kHz) and speech reception thresholds in the children of each group was highly statistically significant. However, children in the ring graft group exhibited good post-operative hearing results that were comparable to those in the fascia group, and in this respect there was no statistically significant difference. These results are similar to those reported elsewhere.Reference Ozbek, Ciftci, Tuna, Yazkan and Ozdem15, Reference Dornhoffer24, Reference Gerber, Mason and Lambert25, Reference Milewski27, Reference Gamra, Mbarek, Khammassi, Methlouthi, Quini and Hariga28, Reference Dornhoffer and Cartilage31, Reference Dornhoffer32
A literature review revealed that sensorineural hearing impairment may occur in anywhere from 0.7 to 5 per cent of tympanoplasties.Reference Sheehy and Anderson52 However, such hearing impairment is usually associated with ossicular work or drilling. In the current series, no post-operative sensorineural hearing impairment or profound hearing loss was encountered.
Early post-operative neodrum granuloma was detected in two cases in each group. These granulomata resolved within a week of antibiotic steroid ear drops treatment. Otitis externa was noted in one ring graft child and two fascia graft children, and also resolved promptly with the correct antibiotic. Postauricular haematoma and infection were encountered in two cases in the fascia group; the haematoma was drained and the infection was managed with antibiotics. Tragal haematoma and infection were also encountered in two cases in the ring graft group, and were managed in the same way.
• The paediatric population is often thought to be more prone to tympanic membrane graft failure than adults
• This study aimed to evaluate the anatomical and audiological outcomes of primary type one tympanoplasty performed with a modified cartilage–perichondrium composite ‘ring’ graft
• Type one tympanoplasty with a ring graft resulted in graft acceptance of 95 per cent
• The ring graft appears be effective for both perforation closure and rapid hearing improvement in the paediatric population
Immediate post-operative facial nerve palsy was observed in one ring graft child. This was partial and resolved completely within four hours, and was thus considered a temporary complication of postauricular local anaesthesia infiltration, due to the superficial facial nerve pathway in children and possible facial canal dehiscence.
The difference in post-operative complications encountered in the two groups was not statistically significant.
Conclusion
The ring graft is a modified cartilage–perichondrium composite graft comprising a peripheral, ring-shaped piece of cartilage attached to a transparent perichondrial sheet. It has the same advantages as cartilage–perichondrium composite grafts, perichondrial grafts and temporalis fascia grafts, but without their disadvantages. The presence of a firm yet malleable peripheral cartilaginous ring fits and stabilises the graft within the bony annulus and under the tympanic membrane fibrous annulus; this makes the graft resistant to retraction, lateralisation and blunting.
The absence of a large, central cartilaginous disc enables the stretched perichondrium to be freely mobile and transparent and to not fill the middle-ear space or rest over the bulge of the promontory, while at the same time accommodating the handle of the malleus. This gives it a conical appearance and position, similar to the natural tympanic membrane, and allows rapid post-operative healing without any delay in hearing improvement.
The use of a ring graft to reconstruct the tympanic membrane during paediatric myringoplasty achieved good audiometric outcomes that were similar to, if not better than, those for temporalis fascia grafting. Furthermore, ring graft myringoplasty had an excellent tympanic membrane closure rate, creating a tympanic membrane resistant to frequent upper respiratory tract infections and possible perforation. Therefore, the ring graft technique could be used effectively in paediatric myringoplasties, with few graft failures and audiological outcomes comparable to fascia grafting. This could allow most children to resume a normal lifestyle, and would facilitate the early detection of any developing post-operative middle-ear effusion or cholesteatoma behind the newly formed, transparent tympanic membrane.









