Introduction
Although many neurologists contributed to the details of our modern neurological examination, the format of the general neurological examination derives in large part from the organization imposed by John Hughlings Jackson.Reference York and Steinberg 1 At the same time, modern psychiatric mental status examination largely follows the outline promulgated by Karl Jaspers.Reference Jablensky 2 The bedside neuropsychiatric examination builds upon the ideas of these late 19th and early 20th century physicians, but includes a number of specific motor, sensory, and cognitive tasks designed to elicit information useful in neuropsychiatric formulation.
The neuropsychiatric examination is conducted with neuropsychiatric formulation in mind. The contents of the examination follow the traditional model of history, physical examination, mental status and cognitive examination, and review of laboratory and neurodiagnostic findings. One model for neuropsychiatric formulation and treatment planning is shown in Table 1. This article assumes the reader is familiar with the generally accepted outlines of neurological and psychiatric examination in order to focus on aspects of the examination that are particularly important to support neuropsychiatric formulation.
Table 1 Neuropsychiatric formulation and treatment plan

The neuropsychiatric examination is an active and dynamic process requiring the examiner to adapt to the patient and the diagnostic goal. Examples of some different ways the examination might be adapted are listed in Table 2. The examination serves other purposes in addition to supporting the neuropsychiatric formulation. For instance, contrary to the concern that being overly specific in one’s questioning might serve to alienate the patient, detailed inquiry serves to foster a stronger alliance between physician and patient when the examiner makes it clear that the goal is to “see the world through the patient’s eyes.” The examination is adapted in real time to test hypotheses as to the cause or localization of a patient’s complaint. While the physician is conducting the examination, he/she is mentally planning for ancillary testing, treatment, and rehabilitation strategies. The contents of the neuropsychiatric history and review of systems are well covered elsewhere.Reference Benjamin and Lauterbach 3 , Reference Cummings and Trimble 4 It is suggested that the examiner bring standard neurological examination tools and include an optokinetic nystagmus (OKN) cloth or smartphone app, a pulse oximeter, and a clipboard containing blank unlined paper plus any stimuli needed for cognitive assessment.
Table 2 Examples of adapted neuropsychiatric examination for different types of patients or purposes

General Physical Examination
The general physical examination includes careful observation for evidence of dysmorphic features, a particular body habitus, and/or cutaneous findings. In the presence of intellectual disability or autism spectrum disorders, these may indicate a need for specific genetic or microarray testing and increase the likelihood of a syndromal diagnosis. Familiarity with the more common syndromes can be helpful. Ready recognition of Down, fetal alcohol, fragile X, and velocardiofacial syndromes is useful. At least 15 syndromes occurring in at least 1 in 10,000 births have been associated with psychosis in childhood or young adulthood. Clues to these diagnoses come both from recognition of dysmorphic features and from their associated physical and neurologic signs.Reference Benjamin, Lauterbach and Stanislawski 5 Key body areas to observe for dysmorphic features helpful in diagnosis are listed in Table 3.Reference Miles, Takahashi and Hong 6 A suite of phenotyping apps for smartphones or tablets, available from face2gene.com, can be helpful in identifying less common dysmorphic syndromes.
Table 3 Key body areas to survey for dysmorphic features on physical examination

Certain dysmorphic features raise the possibility of abnormal brain development. For example, the presence of midline defects such as hypertelorism, found in several congenital syndromes, may also be a clue to partial agenesis of the corpus callosum. When head circumference is consistent with microcephaly or macrocephaly (greater than 58.4 cm in males or 57.5 cm in females) it is important to determine whether other family members share this trait before assuming it to be indicative of abnormal brain development. Note should also be made of excessive neck circumference, especially with concomitant upper torso enlargement and reduced oropharyngeal opening size combined with snoring, suggesting the possibility of obstructive sleep apnea.
Due to the common embryonic ectodermal origin of the skin and nervous system, dermatologic examination is an important component of neuropsychiatric assessment. Neurocutaneous syndromes may be associated with normal development, especially in the carrier state, or with intellectual disability, seizures, or behavior disorders. Dermatologic findings in the most common of these disorders may be found in Table 4.Reference Chernoff and Schaffer 7 Other findings on general physical examination to watch for include the atrophic glossitis of B12 deficiency, cardiac murmurs that may be associated with congenital abnormalities or chromosome 22 disorders, and joint inflammation that may be a clue to Lyme borreliosis or other rheumatologic disorders.
Table 4 Dermatologic features in common neurocutaneous syndromes

Cranial Nerve Examination
Certain aspects of the standard cranial nerve examination are of added importance in neuropsychiatric disorders. Loss of olfaction in absence of chronic rhinitis, tested at the bedside with scented lip balm or with more specific tests such as “scratch and sniff” multiple choice olfactory testing cards if available,Reference Doty 8 is commonly seen following any level of traumatic brain injury or as an early sign of neurodegenerative disorders such as Parkinson or Alzheimer disease.
In addition to testing ocular pursuits, the oculomotor examination should include screening for supranuclear palsy by asking the patient to look up and down, left and right followed by passive movement of the head to observe for the doll’s eyes phenomenon (vestibular ocular reflex). Supranuclear weakness of vertical gaze with preservation of doll’s eyes may be seen in progressive supranuclear palsy (PSP), typically occurring in middle aged people with a male predominance, as well as in children or young adults with Niemann Pick Type C disease. Saccadic pursuits may also be noted in Parkinson disease and PSP. Optokinetic nystagmus (OKN) is observed when the patient is directed to watch each stripe as the examiner passes a striped cloth or turns an OKN drum in front of the eyes. Frontal pathology can result in failure to direct the eyes to the approaching target while failure to pursue the target is evidence of more posterior pathology. The “OKN Strips” smartphone/tablet app can facilitate OKN testing. The examiner should also routinely check for internuclear ophthalmoplegia (INO), a common finding in demyelinating disease in young adults and an occasional finding in vascular lesions in older adults. INO indicates a lesion of the medial longitudinal fasciculus in which the ipsilateral eye cannot adduct and the contralateral eye develops nystagmus with attempts to abduct, thus resulting in horizontal diplopia when looking away from the side of the lesion. Bilateral INO is commonly associated with demyelinating disease. Unilateral INO may be more common in vascular etiologies. To check for INO, the examiner stands with hands horizontally outstretched and directs the patient to look at one hand, then, when the examiner snaps his/her fingers, to quickly look at the other hand. The quick horizontal movement accentuates the ophthalmoparesis. The examination of oculomotor movements also affords an opportunity to obtain information about prefrontal executive function, specifically the capacity for independent as opposed to stimulus bound behavior, using the anti-saccade task. Following the standard examination of ocular pursuit movements, the patient is asked to direct his or her gaze in the direction opposite to the movement of the examiner’s finger. Inability to overcome the pull to pursuit of the examiner’s finger increases the evidence for stimulus bound behavior. When evaluating possible dementia, the examiner should be alert for prolonged fixation on a stimulus that can be a clue to the “visual grasp” of posterior cortical atrophy and Alzheimer disease.
If temporal pathology is being considered, examination of facial strength should include elicitation of spontaneous smile in addition to smile to command. Asymmetric spontaneous or emotional smile in the presence of symmetrical smile to command has been associated with lateralized limbic, basal ganglia, or supplementary motor area (SMA) pathology.Reference Hopf, Müller-Forell and Hopf 9
A simple addition to the cranial nerve examination to specify the pattern of dysarthria is to have the patient repeat the phonemes, “pa,” “ta,” and “ka” individually and then in succession, “pa-ta-ka.” These phonemes test sounds emphasizing labial, lingual, and guttural vocal muscles respectively. Inability to maintain consistent volume and pitch when asked to utter a prolonged “ahh” indicates scanning speech consistent with cerebellar dysfunction. Examination of the gag reflex is seldom as helpful in the assessment for dysphagia as is observation of the patient swallowing a full tumbler of water without pause. Commonly seen in neuromuscular diseases, dysphagia is also a cause of morbidity in neuropsychiatric patients with movement disorders such as tardive dyskinesias or parkinsonism.
Motor Examination
After examining all 4 limbs for muscle bulk, tone, and strength, and eliciting the deep tendon reflexes, the examiner should test for pathological reflexes seen in upper motor neuron lesions. If the Babinski response is equivocal, the examiner can test for the Gordon (squeeze calf muscle), Chaddock (stroke lateral malleolus with sharp stimulus analogous to Babinski), Gonda (flick another toe downward), or Oppenheim (stroke tibia between 2 knuckles of hand) signs to elicit great toe dorsiflexion as evidence of upper motor neuron abnormality in the lower extremity. Primitive reflexes relevant to brain function include the glabella tap, forced grasping, the palmomental, snout, and suck reflexes. The positive glabella tap (also known as Meyerson’s sign) is the persistence of the eyeblink reflex for 5 or more light finger taps over the glabella and may be seen in Parkinson disease or diffuse frontal dysfunction.Reference Schott and Rossor 10 The grasp or forced grasping response, in which upward stroking across the outstretched palm results in the patient grasping the examiner’s fingers ever more tightly as the examiner attempts to withdraw, has been associated with medial prefrontal and SMA dysfunction, though unilateral damage may produce bilateral grasping.Reference De Renzi and Barbieri 11 A related response in the lower extremity is the forced foot grasp and groping response, elicited by stroking the sole of the seated patient’s foot with the side of the reflex hammer and then placing the hammer in front of the foot. If present, the toes will curl as if to grasp the hammer and the foot will extend toward the object in front of it.Reference Fradis and Botez 12 The palmomental reflex, a less specific release sign that can be seen in normal or abnormal brains, is elicited by stroking the thenar eminence while watching for ipsilateral mentalis muscle contraction.Reference Owen and Mulley 13 Snout and suck reflexes are primitive oral reflexes elicited by tapping the philtrum (snout response) or touching an object to the lips (suck response), respectively. With exception of the grasp and grope responses, which appear to reflect frontal dysfunction, these reflexes are nonspecific indicators of brain dysfunction.
When examining for cerebellar dysfunction, which can be associated with cognitive and mood abnormalities, the examiner should observe for saccadic intrusions and square wave jerks with oculomotor movement, difficulty with the pa-ta-ka test (above), scanning speech, decreased muscle tone, decreased check response during pronator drift and reflex testing, difficulty producing regular rapidly alternating movements, difficulty smoothly following a target with a finger, and dysmetria on reaching toward an object, especially toward the end of the movement.Reference Bodranghien, Bastian and Casali 14
Abnormal involuntary movements and their associated signs are frequently seen in neuropsychiatric disorders. Decreased spontaneous movement is part of the psychomotor slowing of depression and some delirium. Increased overall movement is a component of the psychomotor agitation of manic behavior and ADHD as well as some delirium. The catatonic syndrome includes catalepsy; prolonged posturing such as “schnauzkrampf” and the psychological pillow; waxy flexibility; mitgehen and mitmachen (automatic obedience); stereotypies; echopraxia and echolalia; ambitendency; negativism (gegenhalten); and may include mutism and autonomic instability. Gegenhalten (paratonia) may also be seen in cortical dementias. When a syndrome including parkinsonism is suspected, examination for the triad of akinesia, rigidity, and resting tremor is supplemented with the supranuclear gaze exam (above), activation of the contralateral side to bring out latent rigidity during the examination for tone in the upper extremities, and observation for arm swing and en bloc turning during the gait examination. Axial rigidity and akinesia are typically more prominent than tremor in atypical parkinsonian syndromes such as corticobasal degeneration, PSP, and the frontotemporal dementias. Inability to accurately stop clapping when asked to quickly clap 3 times (the applause sign) has been associated with PSP.Reference Dubois, Slachevsky, Pillon, Beato, Villalponda and Litvan 15 The feeling that one hand is foreign or has a mind of its own, or the inability to recognize one’s own hand, often combined with involuntary movements of the hand, is known as the alien hand sign and can be seen in corticobasal degeneration as well as in disruption of the corpus callosum.Reference Doody and Jankovic 16 The abnormal involuntary hyperkinetic movements of tic, tremor, dystonia, choreoathetosis, and hemiballism may be seen in degenerative extrapyramidal disorders, focal lesions, medication toxicity, and tardive dyskinetic syndromes. Tics also occur in obsessive-compulsive disorder (OCD) and Gilles de la Tourette syndrome. The Abnormal Involuntary Movement Scale (AIMS) examination can be incorporated to quantify choreoathetoid movements.Reference Munetz and Benjamin 17 With the patient seated, observe for adventitious movements, which can be the earliest sign of choreoathetoid movement disorder. A series of distraction maneuvers is used to accentuate movements with arms outstretched (piano-playing fingers), and during fine finger movement, mouth opening, tongue protrusion, standing, and walking (observe face, arm, trunk, legs during each). The examiner should observe for presence of the bon-bon sign (exploratory tongue movement with mouth closed), glottal movement with mouth closed, and sudden inhalation while speaking indicative of diaphragmatic dyskinesia. In the pre-neuroleptic era, abnormal involuntary movements were very common in schizophrenia so their presence may not necessarily indicate tardive dyskinesia.Reference Whitty, Owoeye and Waddington 18
Sensory Examination
The primary sensory examination is supplemented with the assessment of cortical sensation by testing for graphesthesia, stereognosis, 2-point discrimination, and double simultaneous stimulation, indicators of contralateral parietal function. Graphesthesia is assessed by asking the patient to identify a number traced on the fingertip, or palm, using the wooden end of an applicator stick. To test stereognosis, the patient is asked to name a small object placed in his/her hand without looking at it. Inability to name objects placed in the left hand with preserved ability in the right may also be consistent with callosal dysfunction. Two-point discrimination can be tested with a specially designed 2-point discriminator tool that determines the minimum distance between 2 points at which they are perceived as separate. As an alternative the examiner can use a notecard with pinholes at 5, 7, and 10 mm separation. Double simultaneous stimulation may be tested for touch, vision, or hearing as a measure of hemi-neglect. The patient is asked to identify the side being touched when the examiner lightly touches both limbs at once; to identify the finger that is moving when the examiner moves fingers in both hemifields simultaneously; or can be asked to identify the sound when the examiner simultaneously produces different sounds in each ear (eg, crinkling paper vs jingling keys).
Gait Examination
If there is concern for parkinsonism, the patient can be asked to arise from a chair without using his/her hands. In the process of performing the Romberg task, the examiner should note signs of motor impersistence, associated with right frontal dysfunction.Reference Kertesz and Hooper 19 . Asked to stand with feet together, eyes closed, and hands outstretched, the patient with motor impersistence will require reminders to continue all 3 aspects of the command. The examiner can then also perform the pull test by pulling the patient’s shoulders back sharply while standing behind him/her. In the absence of postural instability patients should be able to stabilize themselves without stepping backward. In addition to observing for antalgia and use of gait appliance, the gait is observed for initiation, stride length, speed, step height, circumduction, and adventitious movements. In addition to the observation of heel, toe, and tandem walking, the patient can be asked to walk on the lateral surfaces of the feet to help bring out hemi-dystonic upper extremity posturing.
Neurodevelopmental “Soft” Signs
A number of neurodevelopmental signs, often referred to as neurological soft signs (NSS), may be found during the examination of people with schizophrenia, bipolar disorder, substance use disorders, OCD, antisocial personality disorder, or neurodevelopmental disorders. NSS, which tend to decrease in adolescence and young adulthood, are nondiagnostic of localized lesions and may also be found in children with prematurity, low birth weight, and malnutrition.Reference Whitty, Owoeye and Waddington 18 Their relationship to the pathophysiology of mental illness is yet unclear but they appear to decrease in frequency with improvement in psychiatric symptoms.Reference Mittal, Hasenkamp and Sanfilipo 20 A listing of neurodevelopmental signs may be found in Table 5.
Table 5 Neurodevelopmental (“soft”) signs

Embellishment and Malingering
Neuropsychiatrists frequently examine people with signs of possible symptom embellishment or malingering. A number of bedside techniques may be useful in this situation. When examining a person with complaint of visual field cut or tunnel vision, simply assess visual fields at 30 cm, 1 m, and 5 m. The visual field should expand with distance and not remain restricted like a tunnel. Anesthesia to pinprick and skull sensation to vibration that precisely split the midline are not consistent with neurogenic deficits. A positive Hoover sign, in which the supine patient fails to press down on the examiner’s hand with the heel of the normal leg during attempted straight leg raising of the hemiparetic leg, is also inconsistent with neurological etiology. Feigned hemianesthesia may also be detected by having the patient hold his/her hands out crossed with thumbs downward, then clasp and interdigitate the hands and rotate them upward before assessing primary sensation.
Cognitive Status Examination
There is a widespread tendency for psychiatrists and neurologists to substitute a rating scale screening test, such as the Mini Mental State Examination (MMSE), for bedside cognitive assessment. While rating scales are important to include to allow for reliable comparison of examinations, they are usually not sufficient for understanding the cognitive basis for a patient’s symptoms, nor reaching a precise neuropsychiatric diagnosis. A reliable, freely available, general purpose cognitive screening task is the Montreal Cognitive Assessment (MoCA). There are 3 full versions to avoid rehearsal effect and additional versions for use with illiterate or blind patients, as well as translations into a great number of languages at mocatest.org. The MoCA has been validated for minimal cognitive impairment in addition to more severe dementias. Corrections for age and education are available online. The MoCA can be inserted into the bedside cognitive examination at a convenient point.
When presenting a cognitive task, the examiner must be certain that the patient has established set (understands the task demand) before concluding there is evidence for a specific deficit. Convergent findings from different aspects of the neurological and cognitive examination increase the examiner’s confidence in any suspected findings. During the examination, successful performance on a screening question can allow the examiner to move on to other areas. For example, the ability to execute the command: “Hold up the number of fingers on your left hand equal to the order in the alphabet of the capital of China” involves intact working memory, right/left orientation, auditory comprehension, mental control, general knowledge, and praxis. The ability to solve a verbal shopping problem (Table 6) involves working memory, arithmetic, and executive functions such as cognitive estimation and error checking. It is suggested that unlined paper presented in landscape mode be used for all written tasks and that a clean sheet be presented for each task to minimize errors due to stimulus-bound behavior and perseveration.
Table 6 Bedside cognitive tasks that provide information on prefrontal or executive function (In all tasks observe the process that led to any errors and provide that information in the report.)
Attention
Assessment of cognition begins with arousal and attention. If the patient is unable to attend to the examination, the deficits found may not necessarily reflect neurological dysfunction. Note if the patient is sleepy or sedated, distractible, or suffering from hemispatial inattention, since task performance will be affected. Attention span may be assessed by measuring digit span (normal=7 digits forward), which is more dependent on left hemisphere networks, or pointing span, which is more dependent on right hemisphere networks. To establish pointing span, the examiner places 5 objects on the desk, covers them with a piece of paper, and asks the patient to point to objects in a particular order, then removes the paper. Auditory vigilance, which may be negatively impacted by sleep disorders, substance use, or other causes of attention deficit, is tested by reading a long list of letters and instructing the patient to tap his/her hand when you read the letter A, for example. Errors of omission vs commission are reported. If working memory is in question, several tasks may be of use. Reverse digit span (normal=5) is typically used. Other tasks in approximate order of least to most difficult include counting backward from 20, reciting the days of the week in reverse, the months of the year in reverse, serial 3’s, serial 7’s, alphabetizing the letters in EARTH, and reciting the alphabet in reverse. Alphanumeric sequencing may be used for this purpose, instructing the patient to continue the pattern, 1A-2B-3C ..., for 30 seconds. A slightly more complex task that includes an element of vigilance and error checking is to ask the patient to name the letters of the alphabet that rhyme with “key.” A visual spatial element can be added by asking for the capital block letters that contain curves.
Perseveration is common in prefrontal dysfunction but can be seen with any brain damage. It often accompanies aphasic syndromes and can make language assessment difficult. Perseverance may be tested in a few different ways as well. The “mnmn” and ramparts tasks are reciprocal motor programs that favor language and visual spatial functions respectively (Figure 1). The multiple loops task pulls for both perseveration and stimulus-bound behavior since the patient may be attracted to the similarity of the loops and the number “3.” In each the patient is presented with the target stimulus and asked to copy it underneath and continue repeating the pattern across the page. If stuck-in-set perseveration is present, the patient will be unable to change set to begin the next task and will again start the former task. If there is recurrent perseveration, the patient will begin the new task and then switch back into the previous task after some time. Continuous perseveration is marked by unceasing repetition of the pattern presented.Reference Sandson and Albert 21 Perseveration may be elicited with many other tasks as well. When perseveration complicates cognitive assessment, it is sometimes helpful to “deblock” the patient by changing to a completely different type of task.
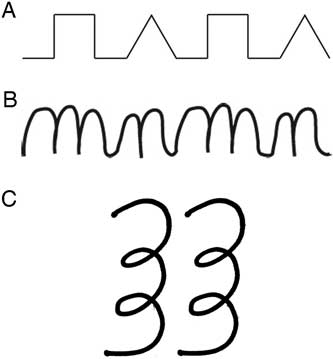
Figure 1 Perseverance tasks.Reference Benjamin and Lauterbach 3 (A) Ramparts, (B) mnmn, (C) multiple loops.
Memory
Complaints of memory loss may be due to attention or memory deficits or to psychological factors. Therefore comprehensive bedside cognitive assessment is indicated in evaluation of memory complaints. Assessment may begin from the moment the examiner enters the room, introducing himself/herself with a cue that can be used later to assess recall and incidental learning. While gathering the history, the examiner may be able to compare information volunteered with that in the record. The examiner can adapt memory tasks to the patient’s estimated cognitive function, choosing to present items for recall with category cues that can be used for later testing. Memory assessment should include both verbal and nonverbal tasks, as well as immediate and delayed recall conditions. Adapting questions for age and culture, an individual’s general fund of knowledge can be tested by asking for facts (eg, how many cards are in a deck? what is the freezing point of water?), general information (what causes rust?), or historical information (what was the Great Depression?). Note is made of intrusions, perseveration, confabulation, or inconsistent performance. Presentation of 4 unrelated words falling into different categories (eg, a color, a flower, an address, and a feeling) can be helpful. Note is made of the number of trials required for the patient to register the words for immediate recall, and then the number recalled spontaneously and at 5 and 15 minutes. If spontaneous recall is incomplete, note is made as to whether performance benefits from category cues or from selecting words from a list. Poor spontaneous recall with accurate selection from a list is consistent with retrieval type memory deficits. Nonverbal recall is tested in a similar fashion but presenting an asymmetric figure for copy, immediate, and delayed recall (Figure 2). The hidden objects task may be used for those unable to complete the above tasks either due to language or other cognitive deficits. The examiner “hides” 3 objects in sight of the patient while saying aloud what he/she is hiding and where it is being placed. Immediate and delayed recall may then be tested spontaneously or with cues. There are many additional bedside memory tasks that can be added for more specific memory assessment. Presentation of a supraspan recall list (eg, 12 words or more) 4 times followed by a spontaneous delayed recall condition can yield information about learning patterns. Similarly, the patient can be presented with a stack of cards containing patterns of lines to assess nonverbal storage vs retrieval deficits. Presentation of pairs of high or low probability associated words (eg, grass-green vs table-elephant) can yield additional information about the interaction of prefrontal function and memory.

Figure 2 Asymmetric figure.Reference Benjamin and Lauterbach 3
Language
Just as in memory assessment, the language examination begins from the moment the examiner encounters the patient. Note is made of melodic line, phrase length, empty vs rich language, paraphasic errors, and other linguistic idiosyncrasies. Aphasia should not be confused with dysarthric articulation disturbances due to motor cranial nerve dysfunction. Apraxia of speech, however, refers to slowed, peculiarly articulated, dysprosodic, or distorted speech related to brain lesion. Script generation is one way to gather data for language assessment. The patient is asked to explain in order the steps in a common task (eg, making pancakes, changing a tire), noting all of the above spontaneous language features as well as serial order errors that may indicate executive dysfunction. Verbal fluency tasks, which yield data on both language and executive function, may also be done at the bedside by asking the patient to list all of the words he/she can in 1 minute beginning with a given letter of the alphabet (phonemic fluency) vs all of the members of a given category (category fluency, eg, animals).
The examination for aphasia includes assessment of auditory comprehension, naming, repetition, reading, and writing. Auditory comprehension is customarily assessed by a combination of gathering the history and giving a 3-step crossed body command, a task that also provides some information about working memory and attention span. The Marie Three Paper Task provides similar information (“Here are 3 pieces of paper. Crumple the large one and toss it on the floor. Give me the medium sized piece and place the small one in your pocket”). Confrontation naming generally includes the naming of body parts, objects and object parts, colors, and actions that occur with high and low frequency in communication. Responsive naming requires the patient to name the object being described by the examiner. Repetition tasks can include sentences of increasing complexity and sentences laden with functor words that express syntactic relationships, connections, or modify nouns or verbs (eg, “no ifs, ands or buts about it”) and are quite difficult for people with expressive aphasia. Oral reading and reading comprehension are assessed by having the patient read a paragraph from a magazine and then explain it. Writing is assessed by having the patient write a sentence. The sentence topic can be varied to obtain more information about the patient’s perception as desired. The writing sample is assessed similarly to spoken language with the addition of looking for spelling errors.
Paralinguistic aspects of communication such as pun, sarcasm, idiom, double-entendre, and emotional prosody rely on right hemisphere as well as left hemisphere networks for comprehension. Assessing these functions requires some nuance. For instance, seeing the humor in a pun produces an almost instant smile, which is different than someone who analyzes the joke in a serial fashion until finally understanding it. The former is assumed to require bilateral networks while the latter process relies more on left hemisphere networks.
Apraxia tends to occur in most aphasias with increased occurrence in Broca and global aphasias. Apraxias have been described as limb kinetic, ideomotor, and ideational.Reference Sandson and Albert 21 Three varieties of praxis are customarily tested: orofacial (“pretend to sniff a flower,” “blow out a match”), limb (how does a police person stop traffic), and transitive (tool use— “show me how you’d brush your teeth” or “pretend to screw in a lightbulb”).
Constructional Ability
The draw-a-clock task (“draw a circle, put in the numbers on a clock, and set the hands to ten past eleven”) can be used as a screen for a host of cognitive deficits, including constructional apraxia, hemi-inattention and neglect, stimulus-bound behavior, and elements of aphasia. As in other screening tasks, abnormalities are followed up with specific tests within the appropriate domains. Construction ability may be further assessed by asking the patient to draw a house showing the front and 1 side, draw a cube, or draw a daisy. With its many small ovoid petals, the daisy drawing can reveal hemi-inattention or hemi-constructional problems. Copying an asymmetric figure can yield information about constructional ability while also probing nonverbal recall, hemi-attention, and learning style. To obtain information that is at least similar to the information derived by neuropsychologists from the Rey-Osterrieth Complex Figure Task, the stimulus should have a discernable external contour, several internal details, and right-left asymmetry. An example is shown in Figure 2. Immediate and delayed recall of the figure can then be used to assess nonverbal recall and learning style.
Executive and Prefrontal Function
Executive function mainly correlates with frontal-subcortical network function, but involves parietal and cerebellar activity as well.Reference Nowrangi, Lyketsos, Rao and Munro 22 Executive function has been shown to correlate with potential for psychosocial and physical rehabilitation.Reference Mak, Wong and Pang 23 , Reference Velligan, Bow-Thomas, Mahurin, Miller and Halgunseth 24 A screening task such as the oral shopping problem above provides a quick estimate of several components of executive function. Observation for motor impersistence and inserting the anti-saccade task into the elemental neurological examination provides additional information. The Luria Three-Step Task, in which the patient is first taught a series of 3 hand positions (fist, side, palm), asked to continue doing the sequence independently, and then transfer it to the other hand, adds information about motor sequencing to the examination.Reference Luria 25 If unable to sequence 3 steps, the patient can be asked to perform a 2-step task (eg, fist-ring task). Verbal and visual sequencing can be tested by asking the patient to unscramble the words in a simple sentence and to put a series of pictures in the correct order to tell a story respectively. The detection of utilization behavior and echopraxia requires creation of space to observe the behaviors. Objects that might have been familiar to the patient in the past are placed within reach of the patient without comment by the examiner. As the examination proceeds the examiner observes any manipulation of these objects by the patient.Reference Lhermitte, Pillon and Serdaru 26 If it appears that the patient may be mimicking the examiner’s movements, observe for echopraxia by first indicating to the patient that he/she should not speak. Then the examiner assumes several poses and observes whether the patient mimics them.
Examples of bedside cognitive tasks that provide information about prefrontal or executive function are listed in Table 6. Observation of the cause of a patient’s errors in other areas of the neuropsychiatric examination yields additional data relevant to prefrontal and executive function.
Closing the Examination
Just as it is helpful to conclude the neuropsychiatric history by summarizing it to the patient to verify that the examiner understands the patient’s complaint, it is also useful to summarize the findings of the neuropsychiatric examination to the patient, explain the most likely causes of any deficits, and clarify the tests or treatment recommendations that will follow.
Conclusion
Conducted in an empathic and careful fashion, the neuropsychiatric examination leads to alliance building, diagnostic hypothesis formation, and the gathering of evidence for neuropsychiatric formulation.










