Introduction
Suicide among adolescents and young people is a major global public health concern and continues to be an important cause of preventable mortality worldwide (Naghavi, Reference Naghavi2019). Globally, suicide is the leading cause of age-standardised years of life lost in many high-income countries in the Asia Pacific region. Moreover, suicide is ranked fourth by age-standardised mortality rate in Eastern Europe, sixth in industrialised countries in the Asia Pacific region, seventh in Australasia, and tenth in Central Europe and industrialised countries of North America (Naghavi, Reference Naghavi2019; World Health Organization, 2018). Deaths from suicide increased by 6.7% between 1990 and 2016, with suicide accounting for 817 000 deaths in 2016 (Naghavi, Reference Naghavi2019). Although the proportion of deaths due to suicide varies by age, suicide accounts for 1.49% of all deaths globally (Naghavi, Reference Naghavi2019) and a staggering 8.5% among young people aged 15–29. The numbers differ between countries but low- and middle-income countries (LMICs) bear most of the global suicide burden, accounting for 75% of all suicides occurring in these countries (WHO, 2014).
Suicidal behaviours entail the spectrum of thoughts that include suicidal ideation (SI), suicidal planning (SP), and suicidal attempts (SA) and are a common phenomenon during adolescence (10–19 years) and among young people (15–24 years) (Hawton, Saunders, & O'Connor, Reference Hawton, Saunders and O'Connor2012), with fatal completion of suicide leading to premature death (Cash & Bridge, Reference Cash and Bridge2009; Seidu et al., Reference Seidu, Amu, Dadzie, Amoah, Ahinkorah, Ameyaw and Kissah-Korsah2020). Childhood and adolescence have been found as a key suicide ‘prevention window’ yet only about 50% of emotional and behavioural disorders seen in these age groups have been clearly defined in terms of the role in suicidal behaviour (Wyman, Reference Wyman2015). Evidence suggests that childhood suicidal behaviours are significantly associated with suicide later in adulthood (WHO, 2014). However, a meta-analysis based on longitudinal studies conducted in 2016 found these associations not to be statistically significant for the longer period (Ribeiro et al., Reference Ribeiro, Franklin, Fox, Bentley, Kleiman and Nock2016). Other studies suggest that suicidal behaviours (i.e. SI, SP and SA) not only lead to life-threatening events (e.g. physical injury) for adolescents but also result in trauma and other psychological issues (Centers for Disease Control and Prevention, 2018). Seventy-five percent of global deaths due to suicide occur in LMICs, which have restricted resources to abate the burden of mental health conditions (WHO, 2014), including suicidal behaviours to prevent disability and deaths (Wyman, Reference Wyman2015). Adolescent suicidal behaviours are likely to be an under-reported burden in LMICs due to religious or cultural norms, social stigma and taboos, and poor reporting systems (Wyman, Reference Wyman2015).
Emerging evidence suggests that food insecurity (i.e. decreased food intake and disrupted eating patterns due to inadequate resources for food) (Nord, Andrews, & Carlson, Reference Nord, Andrews and Carlson2006) and hunger or chronic undernourishment (i.e. as consuming <2100 kilocalories per day for extended lengths of time) may be associated with increased risk of mental illness (Martin, Maddocks, Chen, Gilman, & Colman, Reference Martin, Maddocks, Chen, Gilman and Colman2016). While significant progress has been made in reducing hunger or undernourishment worldwide, current levels remain an issue of major public health significance. For example, although the prevalence of hunger has fallen from 12.6% in 2000 (i.e. 825.6 million people) to 8.9% in 2019 (i.e. 687.8 million people), approximately 750 million people were exposed to severe levels of food insecurity in 2019 (IFAD; UNICEF; WFP; WHO, 2020). LMICs in Africa (36.4% or 250.3 million people) and Asia (55.4% or 381.1 million people) account for 90% of the 687.8 million undernourished people in 2019. Food insecurity and associated hunger are economic stressors, with increasing food insecurity strongly associated with increasing economic hardships, which can be compounded by stressful or adverse life events such as increments in civil strife or armed conflicts, climate-related shocks and economic slowdowns (Floden & Combs, Reference Floden and Combs2013; IFAD; UNICEF; WFP; WHO, 2020; Whitaker, Phillips, & Orzol, Reference Whitaker, Phillips and Orzol2006). Also, people who experience food insecurity tend to report isolation characterised by limited participation in social and community events in their catchments, fuelled by guilt and worry about relying on others in the community for survival. Therefore, the relationship between food insecurity and poor mental health status can be compounded by stressful life events and social isolation. Similarly, food insecurity brings with it shame among parents and their perceived inability to care for their children leads to parental distress (Runnels, Kristjansson, & Calhoun, Reference Runnels, Kristjansson and Calhoun2011). Indeed, the relationship between parental distress and their children's mental health problems is well established (Hattangadi et al., Reference Hattangadi, Cost, Birken, Borkhoff, Maguire and Charach2020; Nilsson, Laursen, Hjorthøj, Thorup, & Nordentoft, Reference Nilsson, Laursen, Hjorthøj, Thorup and Nordentoft2017; Pierce et al., Reference Pierce, Abel, Muwonge, Wicks, Nevriana and Kosidou2020; Renzaho, Mellor, Mccabe, & Powell, Reference Renzaho, Mellor, Mccabe and Powell2013; Van Loon, Van de Ven, Van Doesum, Witteman, & Hosman, Reference Van Loon, Van de Ven, Van Doesum, Witteman and Hosman2014).
Notably, there are several studies on food insecurity and SI and SA (Koyanagi et al., Reference Koyanagi, Stubbs, Oh, Veronese, Smith, Haro and Vancampfort2019; McIntyre, Williams, Lavorato, & Patten, Reference McIntyre, Williams, Lavorato and Patten2013; Romo, Abril-Ulloa, & Kelvin, Reference Romo, Abril-Ulloa and Kelvin2016), limited evidence exist on SA among adolescents (Alaimo, Olson, & Frongillo, Reference Alaimo, Olson and Frongillo2002; Koyanagi et al., Reference Koyanagi, Stubbs, Oh, Veronese, Smith, Haro and Vancampfort2019). Some studies have found a relationship between food insecurity and suicidal behaviours (Shayo & Lawala, Reference Shayo and Lawala2019; Stuff et al., Reference Stuff, Casey, Szeto, Gossett, Robbins and Bogle2004) in the general adult population and adolescents. Others have reported a correlation between poor mental health status and food insecurity among school-going adolescents in high-income countries. Further, food-insecure adolescents have been reported to be significantly more likely to experience suicide behaviour and depressive disorders in Canada and the United States (Alaimo et al., Reference Alaimo, Olson and Frongillo2002; Faught, Williams, Willows, Asbridge, & Veugelers, Reference Faught, Williams, Willows, Asbridge and Veugelers2017) and SI and SA in Southeast Asia (Peltzer & Pengpid, Reference Peltzer and Pengpid2012).
Several common explored risk factors for adolescent suicidal behaviours include demographic factors, victimisation and violence, use of alcohol and drugs, mental health issues, and limited family and peer relationships (Hawton et al., Reference Hawton, Saunders and O'Connor2012; Kokkevi, Rotsika, Arapaki, & Richardson, Reference Kokkevi, Rotsika, Arapaki and Richardson2012; Swahn & Bossarte, Reference Swahn and Bossarte2007). Other factors associated with adolescent suicidal behaviours in LMICs overlap with well-known risk factors in high-income countries, including physical and sexual abuse, bullying victimisation, mental health problems and depressive symptoms (Mahfoud, Rema, Haddad, & Dejong, Reference Mahfoud, Rema, Haddad and Dejong2011), and low-income family and social relationships (Randall, Doku, Wilson, & Peltzer, Reference Randall, Doku, Wilson and Peltzer2014). Existing studies in LMICs using data from the Global School-based Student Health Survey (GSHS) have focused on global variations in the unequal distribution and associated predictors of adolescent suicidal behaviour (Biswas et al., Reference Biswas, Scott, Munir, Renzaho, Rawal and Mamun2020; McKinnon, Gariépy, Sentenac, & Elgar, Reference McKinnon, Gariépy, Sentenac and Elgar2016; Tang et al., Reference Tang, Yu, Wilcox, Kang, Wang and Chen2020; Uddin, Burton, Maple, Khan, & Khan, Reference Uddin, Burton, Maple, Khan and Khan2019). However, previous studies did not examine food security and psychological, protective and lifestyle-related factors associated with suicidal indicators (Biswas et al., Reference Biswas, Scott, Munir, Renzaho, Rawal and Mamun2020; McKinnon et al., Reference McKinnon, Gariépy, Sentenac and Elgar2016; Tang et al., Reference Tang, Yu, Wilcox, Kang, Wang and Chen2020; Uddin et al., Reference Uddin, Burton, Maple, Khan and Khan2019).
Indeed, the 17 Sustainable Development Goals (SDG), adopted by all United Nations Member States in 2015, pledge to ‘leave no one behind’. Target 3.4 emphasises the need to reduce premature mortality from non-communicable diseases by one-third by 2030 through disease prevention and treatment and promoting mental health and wellbeing. However, while the SDGs Indicator 3.4.2 emphasises the importance of reducing the suicide mortality rate, it fails to include defined targets (Uniten Nation, 2020). Clarifying the emotional and behavioural factors for suicide among adolescents and young people is critical to planning and implementing preventive approaches and measuring and evaluating their progress. Meeting the SDGs-target to reduce mental health illness and promote mental health and wellbeing will require a comprehensive multi-sectoral approach that addresses a range of risk factors, including lifestyle behaviours, and considers the local contexts. Therefore, this study aimed to assess the burden of adolescents' suicidal behaviours and its association with violence and unintentional injury and psychosocial, protective and lifestyle factors amongst school-based adolescents across 77 countries with six WHO regions, including 12 low, 29 lower-middle, 25 upper-middle and 11 high-income countries.
Methods
Study design and data source
The present study was a cross-sectional design to investigate the factors associated with adolescent suicidal behaviours (i.e. SI, SP and SA) globally, in regional and country income groups. Data for this study were generated from the most recent GSHS [World Health Organization (WHO), 2020]. This survey is a collaborative surveillance project designed to help countries measure and assess the behavioural risk and protective factors among school-based adolescents aged 11–17. The GSHS project was developed by the WHO in collaboration with the United Nations, the United Nations International Children's Fund, the United Nations Educational, Scientific and Cultural Organisation, and the Joint United Nations Programme on HIV/AIDS with technical assistance from the United States Centers for Disease Control and Prevention. The GSHS is a low-cost school-based survey that collects on health behaviours and protective factors associated with the leading causes of morbidity and mortality among children and adults worldwide. The questions in each GSHS are tailored to each country's context, but the study design and participant selection procedure are similar across the 101 GSHS countries. In this study, data were used from 77 countries (with data on suicidal behaviours in the six WHO regions) among school-based adolescents aged 11–17. The World Health Organisation defines adolescence as the transition phase that children go through between 10 and 19 years, which falls within the WHO's conceptual definition of young people (10–24 years) (World Health Organisation, 2020). For this study, the word ‘school-based adolescents’ has been adopted and used consistently throughout the manuscript.
Sampling procedure
A two-stage cluster sampling technique was used for the GSHS to obtain a representative sample of school-based adolescents globally. During the first stage, the schools representing geographic regions of a specific country were selected. During the second stage, schools were chosen with a probability proportional to enrolment size, after which classes within these schools were selected randomly, such that all students in a selected class and school had an equal probability of participation. All students in these selected classes were eligible to participate in the survey. A standardised scientific survey procedure was performed consisting of a common school-based methodology, including core questionnaire modules, core-expanded questions and country-specific questions that were combined to form a self-administered questionnaire that could be administered during one regular class period [World Health Organization (WHO), 2020]. Detailed information regarding survey sampling, quality control, management and survey instruments has been reported elsewhere [World Health Organization (WHO), 2020]. A total of 251 763 samples (i.e. school-based adolescents) were drawn from 77 countries, including 12 low-income, 29 lower-middle-income, 25 upper-middle-income and 11 high-income countries, based on the World Bank classification (World Bank, 2021) at the time of the survey. The study participants were distributed across the six WHO international geographical regions (online Supplementary Appendix Fig. A1). A high proportion of school-based adolescents participated from the Americas (32.85%), followed by Western Pacific (17.76%), African (16.66%) and South-East Asian (17.04%) regions.
Measures
Outcome measures
School-based adolescent's suicidal behaviours included SI, SP and SA and the magnitude of suicidal behaviours as the outcome variables. In this study, each of these outcome variables was measured with a single self-reported item or question. SI and SP were assessed using two items with a response option of ‘yes’ or ‘no’: ‘During the past 12 months, did you ever seriously consider attempting suicide?’ and ‘During the past 12 months, did you make a plan about how you would attempt suicide?’ SA was measured based on the question ‘During the past 12 months, how many times did you actually attempt suicide?’ Each response was dichotomised (1 = ‘yes’ if the participants reported suicide behaviour during the past 12 months or 0 = ‘no’ otherwise). By extending the analytical explorations, the number of reported suicidal behaviours among the young school-based adolescents were also considered an outcome variable. Responses were categorised as ‘none’ if the participants reported that they had not experienced any form of suicidal behaviours or as ‘one suicidal behaviour’ if they reported having experienced one suicidal behaviour; ‘two suicidal behaviours’ if they reported having experienced two suicidal behaviours; or ‘three suicidal behaviours’ if they reported that they had experienced three suicidal behaviours.
Explanatory variables
Violence and unintentional injury-related factors: Violence and unintentional injury were assessed by asking adolescents how often they had been physically attacked or participated in a physical fight and the frequency they experienced serious injuries or bullying victimisation. Physical violence by peers was assessed with the questions: ‘During the past 12 months, how many times you were physically attacked?’ and ‘During the past 12 months, how many times were you in a physical fight?’ Participant responses for being physically attacked and fighting one or more times were recoded as ‘yes’ or ‘no’ otherwise. If they reported being seriously injured one or more times according to the question ‘During the past 12 months, how many times were you seriously injured?’, their response was coded ‘yes’, otherwise, it was coded ‘no’. Participants' bullying victimisation was defined as dichotomised (1 = ‘yes’ if the participant reported bullying experiences on one or more days, or 0 = ‘no’ otherwise).
Psychological factors: Two psychological factors included in this study were anxiety and feeling of loneliness. Participant's level of anxiety was assessed using the following question: ‘During the past 12 months, how often have you been so worried about something that you could not sleep at night?’ This item indicated loss of sleep due to worry and was used as a proxy for anxiety (Biswas et al., Reference Biswas, Scott, Munir, Renzaho, Rawal and Mamun2020). Feeling loneliness was assessed using the question ‘During the past 12 months, how often have you felt lonely?’ These responses were coded as ‘never’, ‘rarely or sometimes’, ‘most of the time or always’.
Protective factors: Protective factors measured peers social support at school and parental regulation and monitoring. Peer support was assessed using a proxy variable based on the question ‘During the past 30 days, how often were most of the students in your school kind and helpful?’ to which students could respond ‘never’, ‘rarely’, ‘sometimes’, ‘most of the time’ or ‘always’. Responses were recorded as 0 = ‘never’, 1 = ‘rarely or sometimes’ or 2 = ‘most of the time and always’. The number of close friends was recorded as 0 = ‘none’, 1 = ‘1–2 friends’ or 2 = ⩾3 friends based on the survey question ‘How many close friends do you have?’ Parental regulation and monitoring were assessed as the role of parental supports using three variables: parents checking homework (i.e. ‘During the past 30 days, how often did your parents or guardians check to see if your homework was done?’), parents understanding the problem (i.e. ‘During the past 30 days, how often did your parents or guardians understand your problems and worries?’) and parental monitoring (i.e. ‘During the past 30 days, how often did your parents or guardians really know what you were doing with your free time?’). Responses were recorded as ‘never’, ‘rarely or sometimes’, ‘most of the time or always’.
Lifestyle factors: Lifestyle factors included questions on food insecurity, sedentary behaviours and obesity. Participant food insecurity (hunger) was assessed according to the following survey question: ‘During the past 30 days, how often did you go hungry because there was not enough food in your home?’ Responses of ‘most of the time’ or ‘always’ were recoded as ‘severe food insecurity (Q1)’, ‘rarely’ or ‘sometimes’ as ‘moderate food insecurity (Q2)’, and ‘never’ as ‘food secure (Q3)’ (McKinnon et al., Reference McKinnon, Gariépy, Sentenac and Elgar2016). This study used these categories since moderate food insecurity is often considered to be an indication that the quality/quantity of food consumed has been compromised, whereas severe food insecurity refers to reduced food intake and disrupted eating patterns (McIntyre et al., Reference McIntyre, Williams, Lavorato and Patten2013). Some questions asked participants about time spent engaged in sitting activities and watching television and their weight and height. For instance, participants were asked, ‘How much time do you spend during a typical or usual day sitting and watching television, playing computer games, talking with friends, or doing other sitting activities?’ Students' daily sitting activities were categorised as follows: ‘none’, ‘<1 h’, ‘1–2 h’, ‘3–4h’ and ‘⩾5 h’.
Socio-demographic factors: Most studies have shown that the risk of suicide increases with age and rates are higher among males than females (Biswas et al., Reference Biswas, Scott, Munir, Renzaho, Rawal and Mamun2020; Ruch et al., Reference Ruch, Sheftall, Schlagbaum, Rausch, Campo and Bridge2019; Tang et al., Reference Tang, Yu, Wilcox, Kang, Wang and Chen2020). Therefore, these two demographic factors were included as explanatory variables. Age was grouped as follows: ‘11–12’, ‘13’, ‘14’, ‘15’, ‘16’ and ‘17 years’. The gender of the participants was coded as ‘male’ or ‘female’.
Statistical analysis
Due to the complex nature of the data, a composite samples option was applied in the analytical exploration, accounting for country-specific primary sampling unit, stratum and sample weight to ensure samples were nationally representative in respect to the study population. All analyses were weighted using a sampling unit, which is derived from the probability of a school being selected, a classroom being selected, school- and student-level non-response, and gender. This included using strata and primary sampling units at the country-specific data. The prevalence of suicidal ideation, suicidal planning and suicidal attempts was weighted and estimated with corresponding 95% confidence intervals (CIs) for the national and regional perspectives. A random-effects meta-analysis was used to generate national and overall pooled estimates of suicidal behaviours using the Laird inverse variance method. Forest plots exhibit the prevalence of SI, SP and SA by country and its corresponding weight and the pooled prevalence with 95% CIs. Heterogeneity was investigated using the I 2 statistic and a high level of inconsistency (I 2 > 50%) was used to justify random-effect modelling. In the analytical exploration, binary logistic regression (outcome variables: adolescents' suicidal behaviours as dichotomised) and multinomial logistic regression (outcome variable: the magnitude of adolescents' suicidal behaviours with four category levels: ‘none’, ‘one suicidal behaviour’, ‘two suicidal behaviours’, ‘three suicidal behaviours’) were employed to examine the association between participants' suicidal behaviours (SI, SP and SA) and a set of explanatory factors (e.g. socio-demographic, violence and unintentional injury, psychological, non-communicable disease risk and protective factors). Regarding the explanatory variables, the category levels found to reflect a lower risk of suicidal behaviours (or magnitude of suicidal behaviours) were considered the reference for constructing odds ratios using binary logistic regression or relative risk ratios using multinomial logistic regression, with a 95% CI. The study also looked at interaction effects in the regression models. Statistical significance was considered at the 5% risk level. All analyses were performed using the statistical software Stata/SE 15 (StataCorp, College Station, Texas, USA).
Results
Participants' characteristics
The sample consisted of 251 769 school-based adolescents (51.9% female) (Table 1). The majority of participants (~ 92%) were adolescents aged 13–17 years. Seven percent of participants experienced severe food insecurity, and 39.6% experienced moderate food insecurity. Almost one-third (30.7%) of participants reported having been bullied on one or more occasions in school, and 8.7% reported a feeling of anxiety most of the time or always during the past 12 months preceding the survey. Almost one in eight (11.6%) participants reported feelings of loneliness. Regarding physical violence by peers, approximately 33% of adolescents reported having been physically attacked and participating in physical fighting, and 39% of adolescents had been seriously injured by their peers. Approximately 61% of students had at least three close friends, and 40% reported experiencing positive peer support most of the time or always. In terms of the role of parental control, 39% indicated that their parents checked their homework, while 39.3% and 44.7% reported that their parents had attended to their problems and engaged in monitoring their leisure activities at least regularly, respectively. Approximately 35% of participants were engaged in less than 1 h of sitting per day; however, 33% of school-based adolescents reported 3 h or more of sitting per day for the past 30 days. Approximately 6% of adolescents were obese, and 9.8% of adolescents were overweight.
Table 1. Participant's background characteristics

CI, confidence interval; Q1, severe food insecurity; Q2, moderate food insecurity; Q3, food security.
Unequal distribution of school-based adolescents' suicidal behaviours during the past 12 months
The population-weighted 12-month pooled prevalence of SI, SP and SA amongst school-based adolescents aged 11–17 years was 18% (95% CI 16–19%), 18% (95% CI 15–21%) and 16% (95% CI 14–18%), respectively, which varied between countries and regions (online Supplementary Appendix Table A1). Country-wise prevalence ranged from 1.1% in Myanmar to 35% in Kiribati. Regarding SP, the overall weighted pooled prevalence was 18%, and the prevalence ranged from 0.2% in Myanmar to 41% in Zambia (online Supplementary Appendix Table A1). Globally, 16% of adolescents reported they had attempted suicide at least once during the past 12 months. Across countries, the prevalence of SA was highest in Samoa (62%), followed by the Solomon Islands (38%), Kiribati (31%) and Tokelau (29%). The lowest prevalence was found in Indonesia (4%), Bangladesh (5%), Lao People's Democratic Republic (5%), Brunei Darussalam (6%) and Cambodia (7%). Also, the pooled prevalence of school-based adolescent suicidal behaviours (i.e. SI, SP and SA) were unequally distributed and two times higher among adolescents with severe insecurity compared with their food-secure counterparts for all geographical regions (Fig. 1).
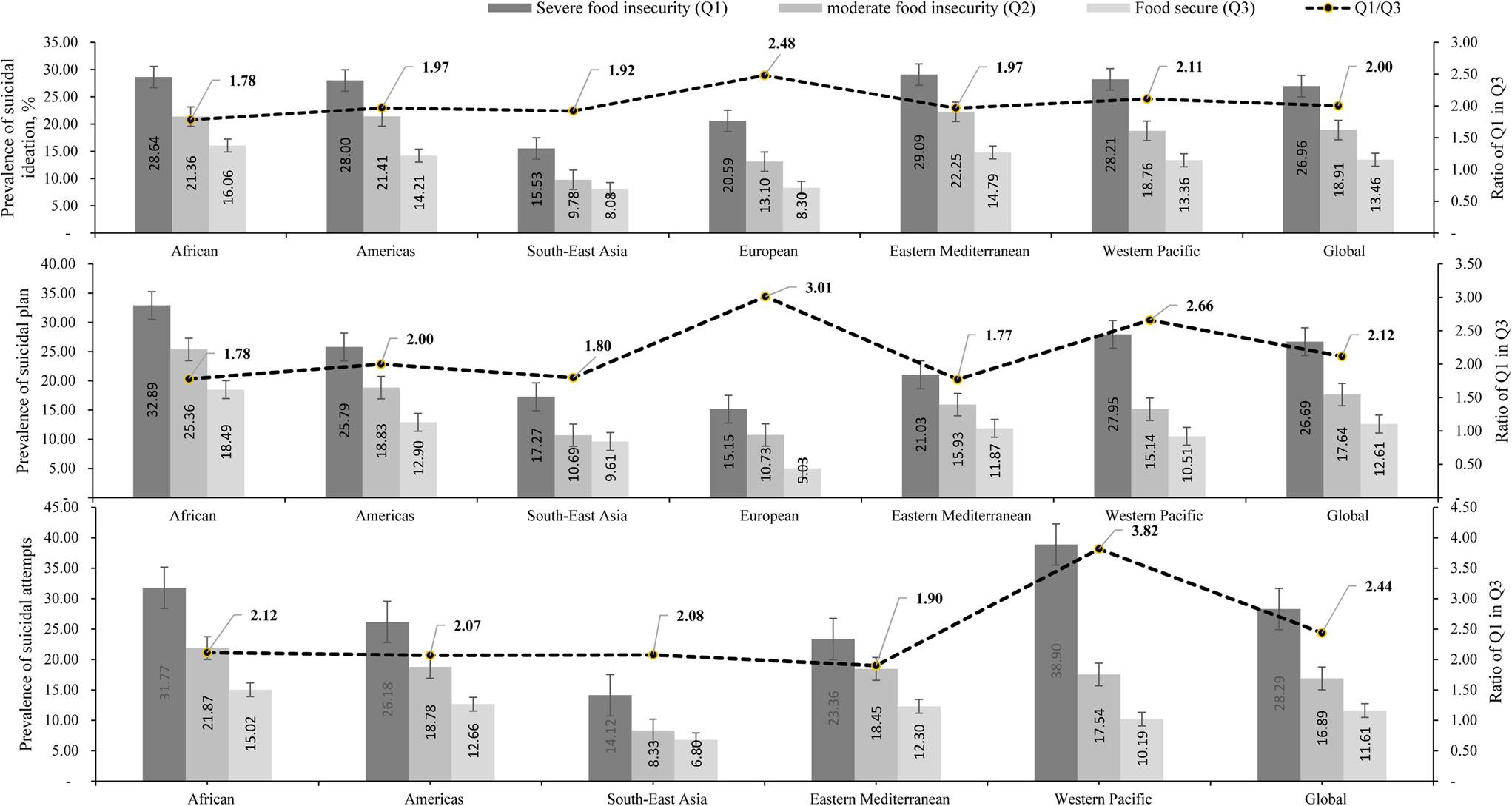
Fig. 1. Unequal distribution of food security among adolescents' suicidal burden.
Association of school-based adolescents' suicidal ideation, planning and attempts
Table 2 presents the regression outputs by food security levels. After controlling for factors in the table, adolescents who reported experiencing violence and unintentional injury (e.g. being physically attacked, participating in physical fighting, being seriously injured and being bullied) were at a higher risk of suicidal behaviours. For example, school-based adolescents who reported being physically attacked, participating in physical fights, and being seriously injured and being bullied (i.e. victimisation by peers) were respectively at higher risk of SI (OR 1.28, 95% CI 1.23–1.33; OR 1.32, 1.27–1.38; OR 1.42, 1.37–1.48; OR 1.56, 1.50–1.62), SP (OR 1.29, 1.23–1.34; OR 1.34, 1.29–1.39; OR 1.47, 1.42–1.53; OR 1.54, 1.48–1.60) and SA (OR 1.45, 1.38–1.51; OR 1.54, 1.48–1.62; OR 1.67, 1.60–1.75; OR 1.87, 1.79–1.96) than those who did not experience any physical violence and unintentional injury. The magnitude of suicidal behaviours was comparatively more pronounced among school-based adolescents who experienced moderate to severe food insecurity than those who reported food security (Table 2).
Table 2. Association of adolescent's suicidal behaviours and associated factors across food insecurity for the global perspective

CI, confidence interval; AOR, adjusted odds ratio; CI, confidence interval; ref, reference category.
Similarly, psychological factors were associated with school-based adolescents' suicidal behaviours. For example, adolescents who reported anxiety had higher odds of having SI (OR 2.64; 95% CI 2.36–2.96), SP (OR 2.51; 95% CI 2.23–2.82) and SA (OR 2.55; 95% CI 2.25–2.90) than those who reported not experiencing anxiety. Similarly, adolescents who felt lonely had significantly higher odds of having SI (OR 2.90; 95% CI 2.74–3.07), making a plan to commit suicide (OR 2.19; 2.07–2.32) or attempting suicide (OR 2.57; 2.40–2.75) when compared to adolescents who did not experience loneliness. Adolescents who reported a lack of parental and poor peer support were at significantly higher risk of SI, SP and SA than those who had supportive parental and peer environments. Adolescents who reported more than 4 h of sitting per day were at significantly higher risk of SI (OR 1.54; 95% CI 1.46–1.62), SP (OR 1.42; 95% CI 1.35–1.49) and SA (OR 1.19; 95% CI 1.12–1.26) when compared to adolescents who engaged in sitting for less than 1 h. To explore the interaction effects, adolescents reporting a lack of parental support and a high level of anxiety were at a higher risk of having SI (OR 1.23; 95% CI 1.06–1.43), SP (OR 1.16; 95% CI 1.01–1.35) and SA (OR 1.26; 95% CI 1.06–1.50). A similar association was observed among school-based adolescents across country income categories [i.e. low, lower-middle, upper-middle and high incomes (online Supplementary Appendix Table A2)] and all geographical regions in terms of SI, SP and SA, except in the European region where there was a paucity of data related to suicide attempts (online Supplementary Appendix Table A3). Concerning the magnitude of suicidal behaviours (Table 3), adolescents who reported being physically attacked, participating in physical fights, being seriously injured and being bullied (i.e. victimisation by peers) were at higher risk of one (relative risk ratios, RRR = 1.17, 95% CI 1.12–1.23; RRR = 1.34, 1.28–1.40; RRR = 1.34, 1.29–1.40; RRR = 1.57, 1.50–1.64), two (RRR = 1.41, 1.33–1.48; RRR = 1.39, 1.32–1.47; RRR = 1.58, 1.50–1.66; RRR = 1.77, 1.68–1.87) and three suicidal behaviours (RRR = 1.31, 1.22–1.39; RRR = 1.49, 1.40–1.59; RRR = 1.84, 1.72–1.96; RRR = 1.85, 1.74–1.97), respectively, than those who did not experience any physical violence and unintentional injury. These associations were also extended with adolescents' characteristics associated with loneliness and anxiety, a lack of parental support and >4 h of sitting per day.
Table 3. Association between number of adolescent's suicidal behaviours and associated factors across food insecurity for the global perspective

CI, confidence interval; Adj. RRR, adjusted relative risk ratio; CI, confidence interval; ref, reference category.
Discussion
This study utilised data from 251 769 school-based adolescents from the latest GSHS survey across 77 LMICs in six WHO regions. Results indicate that adolescents who reported physical violence and unintentional injury-related factors (e.g. being physically attacked, participating in physical fights, being seriously injured and being bullied) were at higher risk of SI, SP and SA than those who did not experience physical violence and unintentional injury across food security categories. This points to the predominant role of violence and unintentional injury in adversely affecting adolescents' mental health (Jensen, Reference Jensen2013; Koyanagi et al., Reference Koyanagi, Stubbs, Oh, Veronese, Smith, Haro and Vancampfort2019; McLaughlin et al., Reference McLaughlin, Green, Alegría, Jane Costello, Gruber and Kessler2012; Seidu et al., Reference Seidu, Amu, Dadzie, Amoah, Ahinkorah, Ameyaw and Kissah-Korsah2020; Yoshikawa, Aber, & Beardslee, Reference Yoshikawa, Aber and Beardslee2012). These associations have been confirmed in other studies, which posited that suicidal behaviours were prevalent among adolescents who had a history of physical abuse (Andover, Morris, Wren, & Bruzzese, Reference Andover, Morris, Wren and Bruzzese2012; Asante, Kugbey, Osafo, Quarshie, & Sarfo, Reference Asante, Kugbey, Osafo, Quarshie and Sarfo2017; Baetens, Claes, Muehlenkamp, Grietens, & Onghena, Reference Baetens, Claes, Muehlenkamp, Grietens and Onghena2011; Seidu et al., Reference Seidu, Amu, Dadzie, Amoah, Ahinkorah, Ameyaw and Kissah-Korsah2020). Adolescents might have engaged in SI, SP and SA after experiencing physical violence and unintentional injuries due to trauma, cognitive distortions and humiliation (Weismoore & Esposito-Smythers, Reference Weismoore and Esposito-Smythers2010). These experiences are associated with long-term adverse effects on self-esteem, self-efficacy, peer and parental relations and high mortality burden (De Beurs, ten Have, Cuijpers, & De Graaf Reference De Beurs, ten Have, Cuijpers and De Graaf2019; McKinnon et al., Reference McKinnon, Gariépy, Sentenac and Elgar2016; Qualter, Brown, Munn, & Rotenberg, Reference Qualter, Brown, Munn and Rotenberg2010; Ribeiro et al., Reference Ribeiro, Franklin, Fox, Bentley, Kleiman and Nock2016; Schinka, VanDulmen, Bossarte, & Swahn, Reference Schinka, VanDulmen, Bossarte and Swahn2012). An understanding of the relation between violence and unintentional injury and suicide is critical to clinicians who deal with children and adolescents as well as to those designing educational and public health prevention programmes for schools (Finan, Swierzbiolek, Priest, Warren, & Yap, Reference Finan, Swierzbiolek, Priest, Warren and Yap2018; Kwon, Kim, & Lee, Reference Kwon, Kim and Lee2018; Waid & Uhrich, Reference Waid and Uhrich2020). Adolescents who are frequently involved in violence and unintentional injury concerns (e.g. being physically attacked, involved in physical fighting, seriously injured, and bullied) should be actively screened for psychiatric problems. School-based screening could be implemented simply by using parent and teacher symptom checklists. This reiterates the need for national and global authorities to implement interventions and strengthen existing ones that support victims of physical violence and unintentional injury-related issues to ensure the achievement of SDG Goal 3.4 by the year 2030.
Our results show that psychosocial factors, such as higher anxiety levels, were significantly associated with suicidal behaviours (e.g. SI, SP and SA) among school-based adolescents. Specifically, adolescents who experienced higher anxiety levels were more likely to be at risk of suicidal behaviours compared to adolescents who had not experienced anxiety. This association has been confirmed in other studies (Mahfoud et al., Reference Mahfoud, Rema, Haddad and Dejong2011; Randall et al., Reference Randall, Doku, Wilson and Peltzer2014), whereby adolescents who experienced higher levels of anxiety were more likely to engage in suicidal behaviours compared to those without anxiety (Mahfoud et al., Reference Mahfoud, Rema, Haddad and Dejong2011; Randall et al., Reference Randall, Doku, Wilson and Peltzer2014). Furthermore, high levels of anxiety in adolescents were commonly related to higher proportions of school dropout and poor school performance (De Beurs et al., Reference De Beurs, ten Have, Cuijpers and De Graaf2019; Thompson, Mazza, Herting, Randell, & Eggert, Reference Thompson, Mazza, Herting, Randell and Eggert2005), which consequently led to decreased personal control (De Beurs et al., Reference De Beurs, ten Have, Cuijpers and De Graaf2019). Co-occurring problem behaviours, common among high-risk youth, are thought to lead directly or indirectly to other mental health problems, such as depression and suicidal behaviours (Pillai, Andrews, & Patel, Reference Pillai, Andrews and Patel2009). However, in a previous study, the authors argued that anxiety did not directly influence suicidal behaviours, but rather indirectly through strong effects on feelings of hopelessness and depression (Thompson et al., Reference Thompson, Mazza, Herting, Randell and Eggert2005) that associate with perceived burdensomeness as the risk of suicidal behaviour (Christensen, Batterham, Mackinnon, Donker, & Soubelet, Reference Christensen, Batterham, Mackinnon, Donker and Soubelet2014; Donker et al., Reference Donker, Batterham, Van Orden and Christensen2014). Although the relationship between anxiety and suicidal behaviours has been a subject of debate in the literature (De Beurs et al., Reference De Beurs, ten Have, Cuijpers and De Graaf2019; Thompson et al., Reference Thompson, Mazza, Herting, Randell and Eggert2005), further exploration is required in the form of a longitudinal or cohort study to confirm this association.
This study revealed that school-based adolescents who felt loneliness most of the time or always had a greater risk of suicidal behaviours than those who did not experience loneliness. Findings concerning the association of loneliness with suicidal behaviours are largely consistent in prior cross-sectional and longitudinal studies (Asante et al., Reference Asante, Kugbey, Osafo, Quarshie and Sarfo2017; Chang et al., Reference Chang, Wan, Li, Guo, He, Gu and Hirsch2017; Dema et al., Reference Dema, Tripathy, Thinley, Rani, Dhendup and Laxmeshwar2019; Pandey et al., Reference Pandey, Bista, Dhungana, Aryal, Chalise and Dhimal2019; Schinka et al., Reference Schinka, VanDulmen, Bossarte and Swahn2012). A recent meta-analytic review showed that suicidal behaviours were more than two times higher among adults experiencing loneliness (Chang et al., Reference Chang, Wan, Li, Guo, He, Gu and Hirsch2017). Lonely adolescents may not be able to share their problems with others to help alleviate their distress, which can exacerbate the negative effect of other issues (e.g. coping with stress, depressive symptoms, alcohol, abuse, poorer sleep quality, personality disorders and Alzheimer's disease) that are associated with suicidal behaviours (Mushtaq, Shoib, Shah, & Mushtaq, Reference Mushtaq, Shoib, Shah and Mushtaq2014). Adolescents who experienced higher levels of loneliness also experienced an extreme comorbidity burden and poor health status (Mushtaq et al., Reference Mushtaq, Shoib, Shah and Mushtaq2014). In adolescence, friendship is a crucial social relationship that can stimulate and encourage adolescents positively by constructing social skills and providing feedback; however, its absence can be directly associated with loneliness and social isolation (Endo et al., Reference Endo, Ando, Shimodera, Yamasaki, Sami, Okazaki and Nishida2017). This proposition is further supported by the evidence that having three (or more) close friends has a protective effect against suicidal behaviours (Dema et al., Reference Dema, Tripathy, Thinley, Rani, Dhendup and Laxmeshwar2019; Pandey et al., Reference Pandey, Bista, Dhungana, Aryal, Chalise and Dhimal2019). Perceived loneliness is associated with higher levels of suicidal behaviours, as it has a strong linkage with other correlates of suicidal behaviours, such as depression. This reinforces the significance of social and peer support in the role of maintaining physical and mental wellbeing and preventing loneliness.
Parental support has been found to be a protective predictor for reducing school-based adolescents' suicidal behaviours. The present study has reported that lack of parental supports increased the risk of SI, SP and SA among adolescents. This association is also consistent with prior studies in different settings, which claimed that high levels of parental supports (i.e. checking homework, understanding problems and monitoring leisure activities) were significantly associated with reducing the risk of suicidal behaviours (De Beurs et al., Reference De Beurs, ten Have, Cuijpers and De Graaf2019; Davison, Marshall-Fabien, & Tecson, Reference Davison, Marshall-Fabien and Tecson2015; Khan et al., Reference Khan, Rahman, Islam, Karim, Hasan and Jesmin2020; Shayo & Lawala, Reference Shayo and Lawala2019; Swahn & Bossarte, Reference Swahn and Bossarte2007; Thompson et al., Reference Thompson, Mazza, Herting, Randell and Eggert2005). Another study conducted in the United States found that strong parental and family supports were associated with a lower incidence of SI among African American students (Harris & Molock, Reference Harris and Molock2000). Similarly, a Taiwanese cross-sectional study conducted in 2008 reported a positive association between adolescent's increased suicidal tendency and parenting with low affection levels (Gau et al., Reference Gau, Chen, Tsai, Lee, Chiu and Hwu2008). The possible reason might be that socio-emotional difficulties, different forms of stress and academic pressure among adolescents abate when they receive parental support. Some studies have also shown that a lack of social and family support was significantly associated with an increased risk of suicide or SI among adolescents aged 12–18 years (Gau et al., Reference Gau, Chen, Tsai, Lee, Chiu and Hwu2008; Harris & Molock, Reference Harris and Molock2000; Miller, Esposito-Smythers, & Leichtweis, Reference Miller, Esposito-Smythers and Leichtweis2015). An earlier study also found that each one-point increase in parental support was associated with a 54% lower incidence in adolescents' suicidal plans (Klaus, Mobilio, & King, Reference Klaus, Mobilio and King2009). By contrast, a longitudinal study piloted among adolescents exhibited contradictory results. Parental support was predictive of lower levels of depression but was not significantly correlated with the outcomes associated with suicidal behaviours (LeCloux, Maramaldi, Thomas, & Wharff, Reference LeCloux, Maramaldi, Thomas and Wharff2017). Negative interactions from family and friends increased perceived burdensomeness and lack of belongingness that leads to an increase in the risk of suicide behaviours (Christensen, Batterham, Soubelet, & MacKinnon, Reference Christensen, Batterham, Soubelet and MacKinnon2013; Joiner et al., Reference Joiner, van Orden, Witte, Selby, Ribero and Rudd2009; Van Orden, Witte, Gordon, Bender, & Joiner, Reference Van Orden, Witte, Gordon, Bender and Joiner2008). Briefly, lack of belongingness and perceived burdensomeness are theorised to comprise suicidal desire (Florence et al., Reference Florence, Bergen, Atherly, Burns, Stevens and Drake2017), and the transition from passive to active suicidal desire occurs when individuals feel hopeless about both these interpersonal and intrapersonal states. Suicidal behaviours are theorised to emerge when active suicidal desire (i.e. the confluence of belongingness and perceived burdensomeness, and hopelessness about these feelings' tractability) interacts with an elevated capability for suicide (Florence et al., Reference Florence, Bergen, Atherly, Burns, Stevens and Drake2017). The interpersonal theory predicts that these constructs represent proximal predictors of suicidal behaviour and as such, may account for the relationship between various suicide risk factors and suicidal thoughts and behaviours. One overarching goal of the interpersonal theory is to aid risk detection and suicide prevention efforts. If the interpersonal theory is able to identify at-risk individuals based on elevated levels of each of its three primary constructs, one might expect that therapeutic intervention aimed at reducing the severity of these constructs may reduce suicide risk (Florence et al., 2017; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). If further work indicates that this theory is a valid predictor of suicide risk, it will be critical to develop and empirically test the efficacy and effectiveness of interventions designed to target its constructs. Such treatments may focus on the bolstering of interpersonal effectiveness skills to enhance social support [e.g. Dialectical Behavior Therapy (Linehan, Reference Linehan2015); Cognitive Behavioural Analysis System of Psychotherapy (McCullough, Reference McCullough2003)], restructuring of negative automatic thoughts surrounding beliefs that one is a burden on others or on society (e.g. Cognitive Behavioral Therapy) (Beck, Reference Beck, Clayton and Barett1983), improving engagement in social activities to build meaningful social connections, and social functioning. Future research should seek to examine the malleability of the interpersonal theory constructs and the effect of manipulating belongingness and perceived burdensomeness on suicidal outcomes.
The main strength of the present study lies in its large sample size and sample selection method. This is one of the first studies that has used a large data set across 77 countries to advance the existing knowledge on the risk and protective factors of young people suicidal behaviours in a global context. This makes the study's findings more precise, reliable and generalizable for school-going young people in countries. Moreover, this study has incorporated several psychological confounders to precisely estimate the risk and protective factors of suicidal behaviours among adolescents. However, the authors acknowledge some limitations with this study design. For example, the study results were derived based on cross-sectional quantitative survey data. The study results cannot infer causality between the various risk and protective factors related to young people suicidal behaviours as the utilised data are cross-sectional. Another limitation of the present study is that the findings may be vulnerable to a level of bias (e.g. responder) as data on outcomes and the main variables of interests were self-reported. Although the data on risk factors and outcomes were obtained using objective measures and adopted standardised and validated methods in terms of cultural and social contexts, the main sources of bias were self-report, instrument bias (e.g. one item to measure suicide) and respondent bias especially in collectivist cultures where respondent might be motivated to answer mental health, and food insecurity issues in any way other than the real situation. These biases have been discussed. In this study, the population-weighted 12-month prevalence of SI, SP and SA amongst school-based young people aged 11–17 years was 18% (95% CI 16–19%), 18% (95% CI 15–21%) and 16% (95% CI 14–18%), respectively. These estimates are consistent with those reported in a previous prevalence-based global study using the same dataset across regional, global and country-income groups in the 12 months preceding survey completion amongst adolescents aged 13–17 years (Uddin et al., Reference Uddin, Burton, Maple, Khan and Khan2019). The prevalence may depend on various environments. The possible reasons accounting for the variations in study findings could be the differences in the measurement of suicidal behaviours as well as differences in time and study settings. In this study, the participant's level of anxiety was defined using the item ‘During the past 12 months, how often have you been so worried about something that you could not sleep at night?’ This item indicates ‘loss of sleep due to worry’ and was used as a proxy for anxiety (Biswas et al., Reference Biswas, Scott, Munir, Renzaho, Rawal and Mamun2020), although the authors acknowledge this is a ‘blunt’ instrument. Interpreting findings about anxiety/worry or the prevalence of suicidal behaviours using data from different settings is a serious challenge in mental health research, making comparisons of findings across studies very difficult. Studies on cross-cultural aspects of anxiety disorders have noted the prevalence is strongly associated with culturally-mediated variations in beliefs about the underlying physiology of mental illness including social norms and cultural rules that govern how mental health is conceptualised and the social contexts in which studied people are exposed to adverse events (Hinton, Reference Hinton2012; Hofmann & Hinton, Reference Hofmann and Hinton2014; Hofmann, Asnaani, & Hinton, Reference Hofmann, Asnaani and Hinton2010). These factors are particularly important in our study because the sample came from 77 LMICs, making a direct comparison within and between regions as well as the literature, very difficult. Such difficulty stems from dealing with data from different cultures, different linguistic backgrounds (e.g. no standardised instruments or surveys), as well as political, geographic and sociodemographic contexts (Hofmann & Hinton, Reference Hofmann and Hinton2014). The net result may overestimate or underestimate anxiety and suicidal behaviours depending on the cultural background and contexts (Asnaani, Richey, Dimaite, Hinton, & Hofmann, Reference Asnaani, Richey, Dimaite, Hinton and Hofmann2010), thereby producing non-compatible findings. Furthermore, due to the lack of specificity and inexistent semantic validity of some mental health constructs, it is possible that, conceptually, the assessment of anxiety in this current study could very well be subsumed under depressive symptoms or more broadly mental health problems. Despite these limitations, the present study might serve as a basis for further studies on predicting suicidal behaviour of young people globally.
Implications for policy and practice
The present study revealed a high level of suicidal behaviour and identified several risk and protective factors among school-based adolescents. Our study presents insight into the development of effective national and global policies to prevent adolescent suicide. Considering the substantial variation across regions and countries, the study results suggest that health policymakers should focus on providing mental health promotion for school-based adolescents. This should emphasise broad multi-sectoral health prevention and promotion strategies (Catalano et al., Reference Catalano, Skinner, Alvarado, Kapungu, Reavley and Petroni2019; Waid & Uhrich, Reference Waid and Uhrich2020) across education, health and community services, including healthy lifestyle and positive adolescent development programmes (Anderson, Gallagher, & Ritchie, Reference Anderson, Gallagher and Ritchie2018; Kwon et al., Reference Kwon, Kim and Lee2018; Metwally et al., Reference Metwally, El-Sonbaty, El Etreby, El-Din, Hamid and Monir2020), and creating links between families and schools. Furthermore, policymakers should ensure that general education about suicide is included in the school curriculum and introduce a school meal programme that may improve adolescent happiness, behaviours and academic performance. School authorities can play a key role in preventing violence and unintentional injury (e.g. being physically attacked, participating in physical fighting, being seriously injured and being bullied victimisation by peers) by positive youth development programmes (Bonell et al., Reference Bonell, Hinds, Dickson, Thomas, Fletcher and Campbell2016) that aim to provide youth with effective relationships and diverse experiences that enable their development of intentional self-regulation and multiple positive assets. These, in turn, may protect against involvement in substance use and violence. Strategies to enhance parental engagement can also protect against suicidal behaviours (Finan et al., Reference Finan, Swierzbiolek, Priest, Warren and Yap2018). Parents should be responsible for building a protective, caring and loving home environment to improve social responsibility, positive awareness and behaviours and enhance social-interpersonal relationships. Schools and communities need to be supported to build a safe and child-friendly environment outside the adolescent's home under the interpersonal theory of suicide (Christensen et al., Reference Christensen, Batterham, Soubelet and MacKinnon2013).
Conclusions
Suicidal burdens are prevailing among school-based adolescents globally. Adolescents in these settings are susceptible to many inducing conditions that mediate their health and wellbeing. Such countries might be euphemised by political tensions, poverty, scarcity of resources and burden of disease. Several psychosocial, risky health behaviours and socio-environmental factors influence suicide burden among adolescents in countries. These findings underscore the importance of early screening to inform the interpersonal theory of suicide (Christensen et al., Reference Christensen, Batterham, Soubelet and MacKinnon2013), policy and require actions to address suicide prevention across countries that are focused on all adolescents attending schools. Universal targeted suicide prevention initiatives are profoundly warranted and should consider the array of cultural and socio-economic backgrounds of the countries, which can then decrease this global burden of suicide. Considering the significant variation among regions and countries, more evidence is needed to explore and understand the sociocultural context of the antecedents of adolescents' suicidal burden and related behaviours globally.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721002774
Data
The latest global school-based student health survey data are publicly available, de-identified cross-sectional dataset. Data can be potentially obtained subject to receive approval from the World Health Organization.
Conflict of interest
None.
Ethical standards
The present study was conducted based on a secondary data source using a cross-sectional data set from the cross-sectional nature in 77 countries that participate in the latest global school-based student health survey. The data are publicly available, de-identified cross-sectional dataset. Ethical approval was not required from an institutional review board because the patient information was de-identified.
Consent for publication
Not applicable.







