Introduction
Chronic otitis media of the mucosal variety is one of the most common clinical conditions managed by an otologist. Surgical management in the form of mastoidectomy is still widely performed by otologists, despite studies demonstrating no potential additional benefit.Reference Trinidade, Page and Dornhoffer1 Advancements in endoscopic ear surgery have led to better understanding of the intricate middle-ear mucosal folds and their significant role in the pathophysiology of middle-ear disease.Reference Marchioni, Mattioli, Alicandri-Ciufelli and Presutti2 Addressing the pathology in the ventilation pathways and preserving the normal transmucosal gas exchange in the mastoid cavity, which is often disrupted in mastoidectomy, logically appears to be the ideal management.
This study aimed to explore endoscopic epitympanic exploration of the ventilation pathways as a modality for managing mucosal chronic otitis media, and to compare it with conventional canal wall up (cortical) mastoidectomy in terms of post-operative outcomes.
Materials and methods
Patient selection, and inclusion and exclusion criteria
Seventy-six patients diagnosed with chronic otitis media (mucosal variety) were included in this randomised controlled trial conducted at a tertiary care hospital between June 2017 and March 2019. The inclusion criteria were: age of 18–55 years, clinical diagnosis of chronic otitis media of the active mucosal variety, and pure conductive hearing loss on pre-operative audiometry.
Patients with history of smoking, known contralateral ear disease, cholesteatoma, or sensorineural or mixed hearing loss, and revision cases, were excluded from our study. All patients underwent pre-operative otoendoscopy, pure tone audiometry, tympanometry and high-resolution computed tomography of the temporal bone. Four patients required ossicular chain reconstruction intra-operatively and were excluded from further statistical analysis.
The patients were randomly assigned to one of two treatment groups: endoscopic epitympanic exploration or conventional canal wall up (cortical) mastoidectomy. The randomisation sequence was generated by a table of random numbers, and allocation was concealed using sealed opaque envelopes. In order to maintain uniformity, all surgical procedures were carried out by the same authors (AD and SM).
Surgical technique
All the cases were performed under general anaesthesia using 2 per cent lidocaine with adrenaline (1:100 000) via local infiltration. A Zeiss operating microscope or Karl Storz (4 mm and 2.7 mm diameter, 18 cm length, 0- or 30-degree) rigid endoscopes with light-emitting diode source were used in the respective groups.
In the endoscopic group, after freshening of the tympanic membrane perforation margins, a superior canal incision was made anterior to the lateral process of the malleus, and an inferior incision was made at the 6 o'clock position. The tympanomeatal flap was elevated. The diagnosis and status of the ossicular chain were confirmed. Depending on the anatomical configuration and extent of mucosal disease, the posterosuperior canal wall was curetted out. This exposes the area around the incudostapedial complex. Optimal exposure was considered to be visualisation of the base of the process pyramidalis and the tympanic segment of the facial nerve (Figure 1). The chorda tympani nerve was gently decompressed to further facilitate exposure. Thereafter, a 2.7 mm, 30-degree endoscope was used to visualise the key ventilation pathways such as the anterior isthmus, posterior isthmus, tensor fold and anterior epitympanic space. Gelfoam® absorbable gelatine sponge, cut into tiny pieces, was used to gently dissect the hypertrophied mucosal folds blocking the aforesaid pathways under direct visualisation, until the ventilation pathways were completely clear. In cases of complete tensor fold, the endoscope was positioned anterior to the malleus handle, and curved dissector and suction instruments were passed to create an additional anterior pathway. The area of bony defect in the canal wall was reconstructed with optimally sized tragal cartilage, to prevent a future retraction pocket. Temporalis fascia was utilised for tympanic membrane reconstruction by the underlay technique. Gelfoam was used to pack the middle ear and external canal.
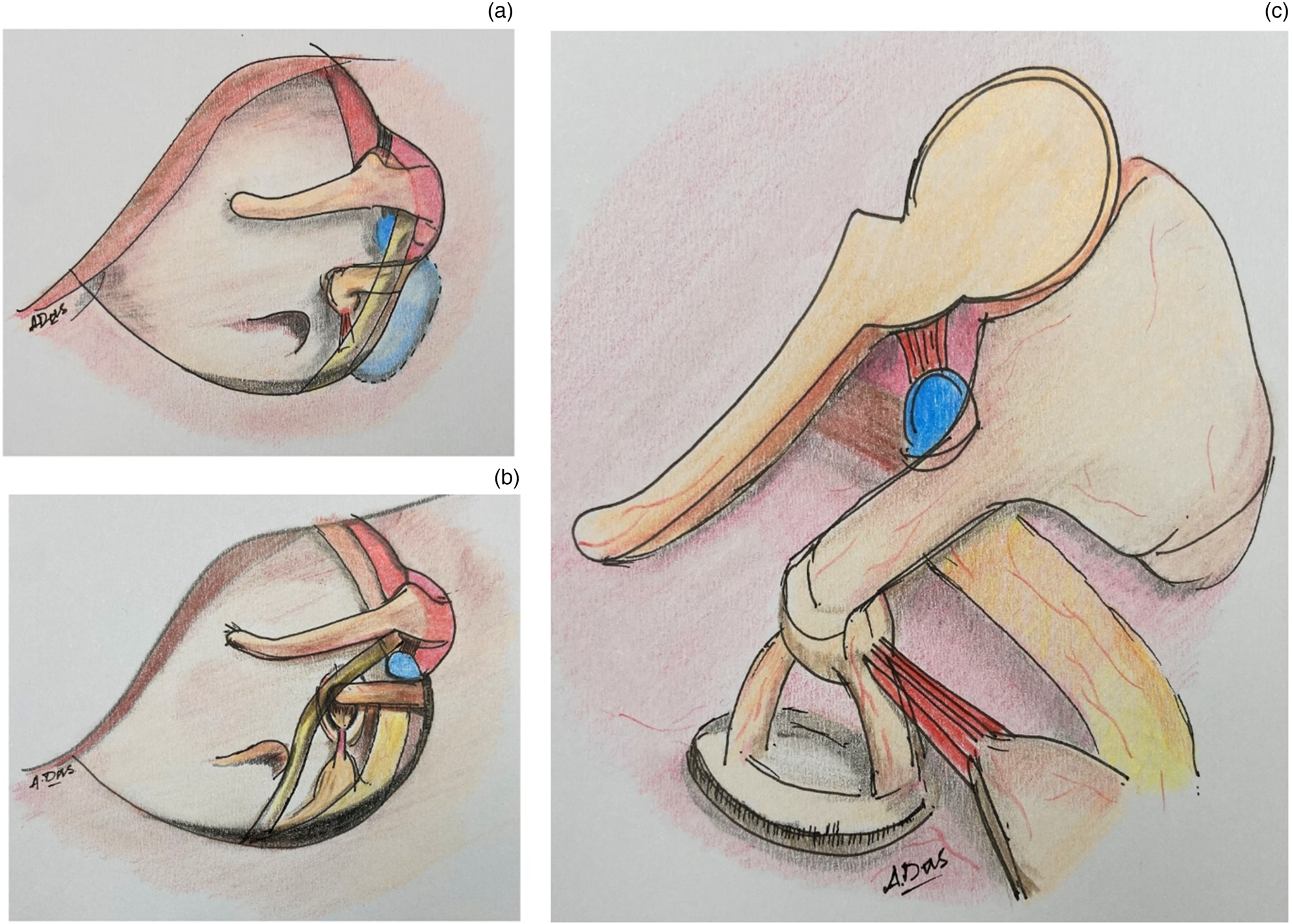
Fig. 1. Endoscopic epitympanic exploration surgical technique: (a) shaded area in blue depicts area of bone curettage; (b) exposure attained after curettage (using a 0-degree endoscope); and (c) visualisation of the ventilation pathways following exposure (using a 30-degree endoscope).
In the microscopic mastoidectomy group, a post-aural incision was made. Temporalis fascia was harvested. The perforation margins were freshened. Canal incisions and exposure of key areas were carried out as in the endoscopic group. A wide cortical mastoidectomy was performed, delineating the dural plate, sigmoid plate, lateral semi-circular canal and short process of the incus. Diseased mucosa was cleared, preserving the normal mucosa, until a clear flow of saline was seen into the middle ear from the mastoid cavity via the antrum and auditus. Temporalis fascia grafting was conducted using the underlay technique. Gelfoam was placed and the wound was closed in layers.
Study parameters and results analysis
The two groups were compared in terms of: surgical time, graft uptake at 1, 3, 6 and 12 months post-operatively, tympanometry and audiological outcomes at 3, 6 and 12 months post-operatively, pain at 6 hours post-operatively, vertigo at 1 week post-operatively, and long-term complications such as retraction pocket or re-perforation at 12 months post-operatively.
For statistical analysis, data were analysed using SPSS (version 24.0; SPSS, Chicago, Illinois, USA) and GraphPad Prism (version 5; GraphPad Software, San Diego, California, USA) statistical software. The data were summarised as mean and standard deviation for numerical variables, and count and percentage for categorical variables. The paired t-test was used for paired samples. Unpaired proportions were compared using the chi-square test or Fisher's exact test, as appropriate. A p-value of less than 0.05 was considered statistically significant.
Results
Demographic distribution
The mean age of patients was 32.5 ± 9.7 years in the endoscopic group and 32.4 ± 9.6 years in the microscopic group. There was no statistically significant difference between the two groups in terms of age. Fifty-five per cent and 54 per cent of the patients were male in the endoscopic and the microscopic groups, respectively. There was no statistical difference between the two groups in terms of sex distribution.
Graft uptake
In the endoscopic group, out of 36 patients, 33 (91.6 per cent), 33 (91.6 per cent), 32 (88.8 per cent) and 32 (88.8 per cent) had graft uptake at 1, 3, 6 and 12 months’ follow up, respectively. In the microscopic group, out of 36 patients, 30 (83.3 per cent), 29 (80.5 per cent), 29 (80.5 per cent) and 28 (77.7 per cent) had graft uptake at 1, 3, 6 and 12 months’ follow up, respectively. No statistically significant differences were noted between the two groups in terms of graft uptake (p = 0.5, 0.3, 0.5 and 0.3, respectively).
Post-operative air–bone gap
The mean post-operative air–bone gap in the endoscopic group at 3, 6 and 12 months’ follow up was 19.9 ± 4.5 dB, 16 ± 5.9 dB and 12.5 ± 6.3 dB, respectively. In the microscopic group, the post-operative air–bone gap at 3, 6 and 12 months’ follow up was 22 ± 5 dB, 18.2 ± 6.7 dB and 18.2 ± 11 dB, respectively (Figure 2). There were no statistically significant differences between the two groups at three and six months’ follow up (p = 0.07 and 0.1, respectively). However, at 12 months’ follow up, the difference in air–bone gap between the groups was statistically significant, with a p-value of 0.01. There were no significant differences between the two groups in terms of pre-operative air–bone gap (p = 0.3) (Table 1).

Fig. 2. Air–bone gaps in the endoscopic and microscopic groups at 3, 6 and 12 months post-operatively. Pre-op = pre-operative; mth = months; post-op = post-operative; EEE = endoscopic epitympanic exploration; CM = cortical mastoidectomy
Table 1. Summary of demographic, pre-operative audiometric and post-operative outcome parameters

* Indicates statistical significance. SD = standard deviation; pre-op = pre-operative; ABG = air–bone gap; post-op = post-operative
Post-operative tympanometry
The post-operative tympanometry conducted at 3, 6 and 12 months’ follow up in the endoscopic group (n = 36) showed an A-type curve in 16 (44.4 per cent), 24 (66.6 per cent) and 27 (75 per cent) patients, respectively. In the microscopic group (n = 36), initial follow-up appointments at 3 and 6 months showed an A-type curve in 14 (38.8 per cent) and 20 (55.5 per cent) patients, respectively; at 12 months, 18 patients (50 per cent) had an A-type curve (Figure 3). No statistically significant difference was found between the groups in this respect (p = 0.8, 0.4 and 0.05, respectively).

Fig. 3. Tympanometry findings (curve type) at 3, 6 and 12 months post-operatively. Note the trendline for the tympanometry type ‘A’ curve in the endoscopic group with increasing duration of follow up. EEE = endoscopic epitympanic exploration; CM = cortical mastoidectomy
Surgical duration
The mean surgical time was 80.9 ± 14 minutes for endoscopic epitympanic exploration and 132 ± 12.5 minutes for the microscope-assisted mastoidectomy group. A statistically significant difference was found between the two groups (p < 0.0001).
Post-operative pain
Post-operative pain was recorded at 6 hours following surgery in terms of a numerical rating scale. In the endoscopic group, the median (range) pain score was 4 (2–7). In the microscopic group, it was found to be 6 (4–8). The difference between groups was statistically significant (p < 0.05).
Post-operative vertigo
Subjective vertigo was assessed at the end of the first week post-operatively. The findings revealed no statistically significant difference between the two groups (p > 0.05).
Long-term complications
The patients were followed up for one year. Long-term complications in the endoscopic group (n = 36) included two cases (5.5 per cent) of re-perforation and one case (2.7 per cent) of retraction pocket formation. In the microscopic group (n = 36), five patients (13.8 per cent) had re-perforation and one patient (2.7 per cent) had retraction pocket formation at one year of follow up. No statistical significance was found between the groups (p = 0.4).
Discussion
The attic or epitympanum communicates with the mesotympanum and is ventilated via two major routes: the isthmus anticus and posticus.Reference Marchioni, Molteni and Presutti3 In the presence of a complete tensor fold, the epitympanum relies solely on the isthmi for its ventilation.Reference Marchioni, Alicandri-Ciufelli, Molteni, Artioli, Genovese and Presutti4 Herein lies the importance of addressing the pathology at these critical sites. The ability to visualise and hence precisely address the disease affecting these areas, which were difficult to approach with the help of conventional microscopes, can be achieved with the help of endoscopes. Endoscopes, by virtue of their wide field of view and angulation (angled scopes), have made it possible to access even remote corners such as the anterior epitympanic space, which were left unattended or necessitated extensive bone drilling and soft tissue disruption when approached via mastoidectomy (Figure 4).Reference Tarabichi5 Moreover, with the advent of specialised curved dissectors and suction instruments designed exclusively for endoscopic ear surgery, it is possible to address the disease in the far anterior epitympanic space or clear a hypertrophied complete tensor fold to make way for an additional anterior ventilation route.
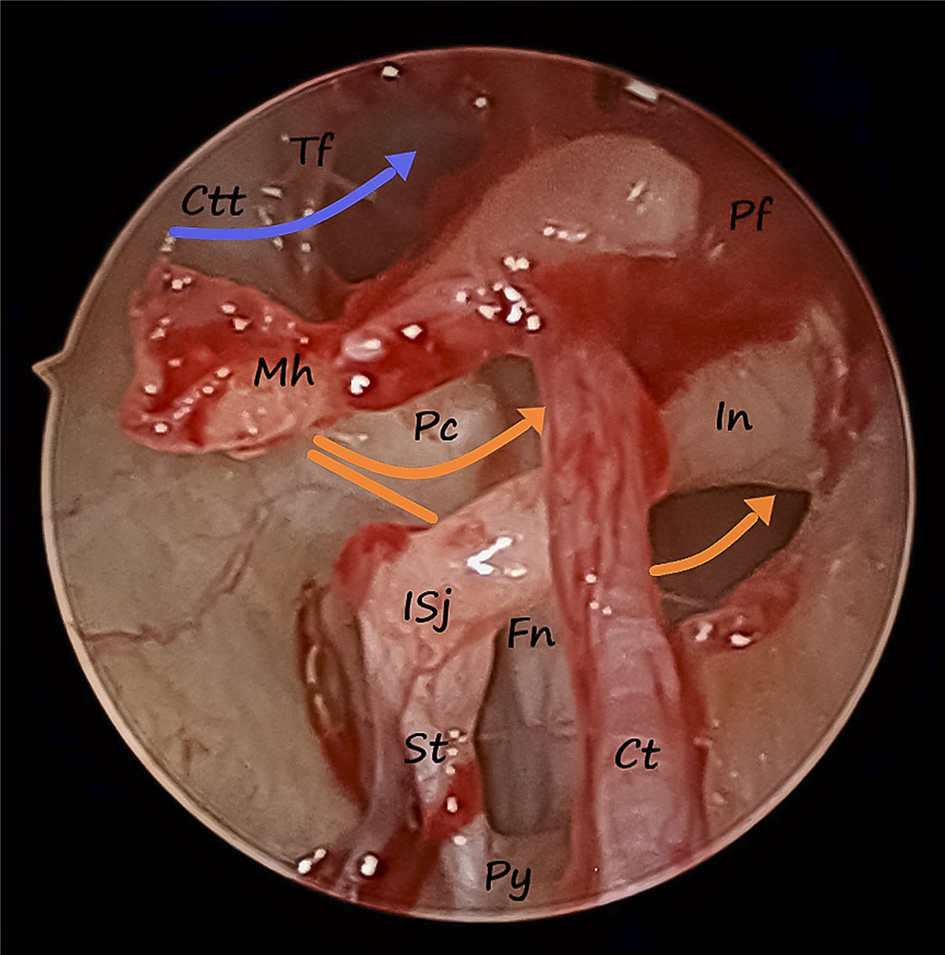
Fig. 4. Left ear endoscopic epitympanic exploration with 2.7 mm 30-degree endoscope. Blue arrow depicts the anterior-most ventilation pathway through the tensor fold; orange arrows depict the isthmi anticus and posticus. Tf = tensor fold; Ctt = canal for tensor tympani; Pf = pars flaccida; Mh = malleus handle; Pc = processus cochleariformis; In = incus; ISj = incudo-stapedial joint; Fn = facial nerve; St = stapedial tendon; Ct = chorda tympani; Py = processus pyramidalis
The tympanic isthmus represents one of the upstream areas of the ventilation system, which also consists of the isthmus of the Eustachian tube, the protympanum and the anterior mesotympanum. Kapadiya and Tarabichi have shown that mastoid exploration, being a posteroanterior approach, is contrary to the natural alignment of the ventilation route.Reference Kapadiya and Tarabichi6 Thus, with the major pathology being located elsewhere, the rationale for adopting a posterior mastoid based approach in mucosal disease appears questionable.
The unintentional yet inevitable consequence of mastoidectomy is disruption of some amount of normal mucosa and architecture of the mastoid cell system. Yet, mucosal gas exchange and the mastoid buffer system are imperative for normal ventilation to resume following surgery.Reference Cinamon and Sadé7,Reference Takahashi, Honjo, Naito, Miura, Tanabe and Hasebe8 Takahashi et al. found that normal capillary-rich mucosa of mastoidectomy cavities was replaced by scar tissue with scanty capillaries. This compromised the gas exchange that is essential to maintain the pressure balance in the middle-ear cleft.
Considering the mucosal variety of chronic otitis media, the literature suggests that concomitant cortical mastoidectomy provides no additional benefit over tympanoplasty alone.Reference Trinidade, Page and Dornhoffer1,Reference Huang, Li, Wu and Wang9,Reference Bhat, Naseeruddin, Nagalotimath, Kumar and Hegde10 This has been found to hold true even when there is radiological evidence of soft tissue opacity in the antrum and mastoid air cells.Reference He, Shou, Hsieh, Wang, Wang and Han11 However, in spite of existing evidence, mastoidectomy for mucosal disease is a common practice among otologists even today.
Endoscopic epitympanic exploration, on the other hand, is a mucosa-preserving, minimally invasive approach. It involves minimal bone curettage for exposure of the isthmi, and use of a soft atraumatic dissection technique with Gelfoam for disease clearance (Figure 5). This technique of ventilation pathway clearance has been devised by the authors and has not to the authors’ knowledge been documented previously. The technique ensures re-establishment of the critical ventilation pathways, and thus prevents long-term complications such as re-perforation or retraction pocket formation. This is further supported by the long-term audiometric and tympanometric results. Eventual necrosis of the ossicular chain caused by ongoing mucosal inflammation around the incudostapedial complex is another concern. This is directly and much more precisely addressed endoscopically, compared with a mastoidectomy for which we follow a completely different approach.

Fig. 5. Left ear endoscopic epitympanic exploration with a 0-degree endoscope showing hypertrophied mucosa blocking isthmi anticus (grey arrow) and posticus (blue arrow), and Gelfoam being used to dissect away chorda tympani. Pf = pars flaccida; Ctt = canal for tensor tympani; Tf = tensor fold; Mh = malleus handle; Pr = promontory; Ct = chorda tympani; St = stapedial tendon; Gf = Gelfoam; Rwn = round window niche
Endoscopes have opened up a new horizon in the domain of otology, facilitating visualisation of structures that were only vaguely understood before. This has dramatically shaped new concepts and helped us to understand the pathophysiology of some of the most common ear pathologies. Any new surgical technique is devised in order to overcome the shortcomings of a practised method based on established concepts. Likewise, endoscopic epitympanic exploration has its own pros and cons. It is minimally invasive, conservative and focused on the site of pathology. However, it demands precision with gentle dissection techniques, and beginners in particular need to exercise extreme caution while working single-handedly between the ossicles.
• Canal wall up mastoidectomy is still widely practised for mucosal chronic otitis media
• Literature suggests no additional benefits of canal wall up mastoidectomy over tympanoplasty alone for mucosal chronic otitis media
• Mucosal disease affecting major ventilation pathways is not addressed by conventional canal wall up mastoidectomy
• Endoscopic epitympanic exploration is a minimally invasive, conservative approach focused on the site of pathology
• The endoscopic technique resulted in better long-term audiological outcomes, shorter operating time and less pain compared to conventional canal wall up mastoidectomy
• Endoscopic epitympanic exploration appears to be a more functional approach than conventional canal wall up mastoidectomy
We do acknowledge that certain differences between the compared techniques may not be significant because of the limited sample size and follow-up period, and this calls for larger multi-centric trials with longer follow-up times.
Conclusion
In this study, with a level of evidence of 1, endoscopic epitympanic exploration resulted in significantly better long-term audiological outcomes, a shorter operating time and less pain compared with conventional canal wall up mastoidectomy for treatment of mucosal chronic otitis media. It is precise, guided by the physiology of the middle-ear ventilation system, and aims to restore normal aeration of the middle-ear cleft with minimal mucosal disruption.
Competing interests
None declared








