Introduction
An organised haematoma is a non-neoplastic, haemorrhagic lesion. When present in the maxillary sinus and nasal cavity, such lesions can cause bone thinning. Maxillary sinus haematoma was first reported in the Japanese literature by Tadokoro in 1917, and described as a ‘blood boil of the maxillary sinus’.Reference Tadokoro1 In the English language literature, this type of maxillary sinus lesion is variously referred to as a haematoma, organised haematoma, haematoma-like mass, or organised haematoma mimicking a tumour; it is also sometimes incorrectly referred to as a haemangioma.
On computed tomography (CT), maxillary sinus organised haematoma often appears as a large, well-defined, homogeneous mass causing considerable expansion of the maxillary sinus wall with resultant bony thinning or destruction.Reference Lee, Park and Heo2 On magnetic resonance imaging (MRI), these lesions contain regions of differing intensity. The basal portion shows the highest intensity on T2-weighted images, and also exhibits contrast enhancement; on histopathological examination, this region shows vascular dilatation. The peripheral portion shows low to moderate intensity on T1-weighted images and moderate to high intensity on T2-weighted images; on histopathological examination, this region shows mucosal swelling with inflammation, and contains a characteristic combination of dilated vessels, haemorrhage and fibrin exudation.Reference Nagato, Sugahara, Watanuki, Tanaka, Mikuriya and Hashimoto3, Reference Yagisawa, Ishitoya and Tsukuda4
The most common treatment modality for maxillary sinus haematoma is endoscopic sinus surgery.
Here, we describe the successful resection of three maxillary sinus organised haematomas. We also describe the differences in histological findings for the basal and peripheral portions of these lesions. The purpose of this article is to clarify the aetiology of maxillary sinus organised haematoma.
Materials and methods
In our institution, the diagnosis of an organised haematoma of the maxillary sinus is based on the following four criteria: (1) clinical findings of nasal bleeding or nasal obstruction and a unilateral, polypoid mass in the nasal cavity; (2) CT scans showing an expanding, unilateral, maxillary lesion with thinning or destruction of the surrounding bony wall; (3) MRI showing a heterogeneous mass; and (4) histopathological examination of the mass showing dilated vessels, haemorrhage and fibrin exudation.
This study examined the clinical records of three patients with proven organised haematoma of the maxillary sinus, who were referred to our institution between January 1997 and May 2011.
Results and analysis
The study included two men and one woman, aged 18, 89 and 18 years, respectively.
The patients' clinical findings are summarised in Table I. The chief complaints of each patient were recurrent nasal bleeding and nasal obstruction. None of the patients had a history of nasal or paranasal sinus surgery.
Table I Patients' clinical findings

Pt no = patient number; Intra-op = intra-operative; Op = operative; min = minutes; M = male; R = right; F = female; ESS = endoscopic sinus surgery
Pre-operative endoscopic nasal examinations in all three patients revealed polypoid masses extending from the maxillary sinus into the nasal cavity (Figure 1).

Fig. 1 Rhinoscopic view in patient one, showing a polypoid mass (asterisk) filling the right nasal cavity.
Computed tomography revealed a well-defined, expansile mass in a unilateral sinus, with destruction or thinning of the bony wall of the maxillary sinus (Figures 2a and 2b). Patients one and two demonstrated thinning of the anterior and posterior walls of the maxillary sinus, accompanied by destruction of the posterior wall. In patient three, only the lateral wall of the maxillary sinus was eroded.
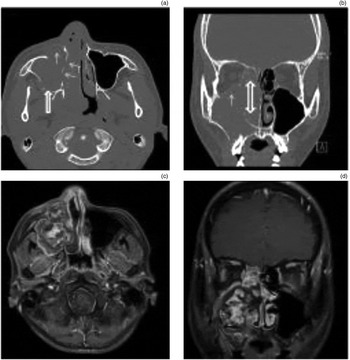
Fig. 2 Radiological findings in patient two. (a) Pre-operative, axial, unenhanced computed tomography (CT) scan showing an expansile lesion in the right maxillary sinus, with bony erosion of the anterior and lateral nasal walls (thin arrows) and destruction of the posterior wall (thick arrow). (b) Coronal CT scan showing erosion of the orbital floor (thin arrow) and enlargement of the natural ostium of the maxillary sinus (double-headed arrow). (c) Axial, T1-weighted, gadolinium-enhanced magnetic resonance imaging (MRI) scan, showing a mass occupying the right maxillary sinus and expanding into the nasal cavity; the basal portion of the mass shows heterogeneous enhancement which is stronger than in the peripheral portion. (d) Coronal, T1-weighted, gadolinium-enhanced MRI scan showing a heterogeneously enhancing mass filling the maxillary sinus and nasal cavity, in the same location as the mass seen in the coronal CT scan.
On MRI, the basal portion of the organised haematomas showed low intensity on T1-weighted imaging and high intensity on T2-weighted imaging; heterogeneous enhancement was observed with gadolinium-diethylenetriamine-penta-acetic acid. In contrast, the peripheral portion of the haematoma showed low to iso-intensity on T1-weighted images and iso- to high intensity on T2-weighted images; gadolinium-diethylenetriamine-penta-acetic acid enhancement was much weaker than that observed within the basal portion (Figures 2c and 2d). In all patients, the mass filled the maxillary sinus and enlarged the natural ostium, with medial displacement of the lateral nasal wall.
Surgical treatment consisted of endoscopic sinus surgery for patient three and a Caldwell–Luc procedure for patients one and two. The clinical and radiological features of these latter two patients raised suspicion of a potentially neoplastic lesion or an organised haematoma with the risk of profuse bleeding, so a Caldwell–Luc procedure was chosen to enable better exposure during removal of the mass.
In patient one, a biopsy had been conducted in the out-patient clinic which had resulted in significant bleeding. This had eventually required ligation of the right maxillary artery, prior to the Caldwell–Luc procedure, to control intra-operative bleeding. A dark-reddish, crumbly mass composed of blood clots and fibrous tissue was found to fill the entire maxillary sinus.
In patients one and two, the basal portions of the mass occupied the natural ostium of the maxillary sinus and tended to bleed. The stem of the basal portion arose from a posterosuperior location within the natural ostium of the maxillary sinus. The mass was friable but bleeding was not serious during surgery, and the mass was completely removed. The natural ostium of the maxillary sinus was found to be enlarged in both patients. After complete removal of the mass, the sinus mucosa appeared to be intact.
Although patient three was similar to the others with respect to pre-operative clinical and radiological features, endoscopic sinus surgery was performed as this young patient was eager for a conservative procedure as the initial approach. The mass was broadly based on the lateral wall near the natural ostium of the maxillary sinus. The maxillary sinus was filled with a friable, dark-red blood clot, fibrous tissue and inflammatory discharge. The basal portion of the mass was located on the posterior aspect of the natural ostium. The basal portion was removed completely together with the surrounding lateral nasal wall. Part of the peripheral portion crumbled easily and could not be removed intact. Bleeding was not serious during the endoscopic sinus surgery procedure, and the mucosa of the maxillary sinus remained intact.
Intra-operative blood loss in these three patients ranged from 30 to 330 ml. No patient required blood transfusion.
Operation times ranged from 30 to 100 minutes.
All the patients' maxillary sinus haematomas were successfully resected. None recurred after surgery.
The histopathological features of the basal and peripheral portions of the resected haematomas were quite different (Figure 3a, 3b). The peripheral portion showed an absence of cellular components and the presence of pseudovessels, necrotic tissue and a fibrin mass (Figures 3c). In contrast, the basal portion showed an aggregation of dilated vessels together with haemorrhage and fibrin exudation around the dilated vessels (Figure 3d). In retrospect, the first patient's pre-operative biopsy specimen demonstrated similar histological features to that of the peripheral portion of the haematoma (Figure 3a).

Fig. 3 Photomicrographs showing histopathological findings for patient one. (a) Biopsy taken at first out-patient clinic visit, showing no epithelial components; only exudative fibrin and red blood cells are seen (H&E; ×100). (b) Second biopsy, showing neutrophils, lymphocytes and red blood cells surrounding necrotic tissue (H&E; ×100). (c) Peripheral portion of the mass, showing that almost the entire mass is composed of necrotic tissue and fibrin. Pseudovessels (with no endocapillary cells) appear to have formed, in which red blood cells are pooled (asterisks). Red blood cells, fibrin and necrotic tissue (arrows) are present around the pseudovessels (H&E; ×40). (d) Basal portion of the mass showing aggregated, dilated vessels (arrows) which appear to be newly formed (as new vessel endothelial cells are present and fibroelastic tissue is absent). There is evidence of fibrotic changes and hyalinisation around the dilated vessels (asterisks) (H&E; ×40).
Discussion
An organised haematoma is a non-neoplastic, haemorrhagic lesion.Reference Kusunoki, Tokuno, Toshikawa and Murata5 The nomenclature of these rare lesions is still not consistent or clear in the English language literature.Reference Omura, Watanabe, Fujishiro, Ebihara, Nakao and Asakage6 A literature review using the Medline database demonstrated that a variety of terms are regularly used to refer to what in this paper is termed a maxillary sinus organised haematoma, including haematoma (75 previously reported cases identified), haemangioma (82 cases), haematoma-like mass of the maxillary sinus (1 case), organised haematoma (10 cases) and organised haematoma mimicking tumour (2 cases).
In a separate search of the Japanese language literature, we identified 75 previously reported cases of maxillary sinus organised haematoma. Although all these patients had similar clinical histories and radiological features, the histological features of their masses were reported differently. The most common diagnostic presenting complaints were recurrent nasal bleeding (32 of 61 cases) and nasal obstruction (17 of 61 cases). Computed tomography showed unilateral and expansile lesions, maxillary opacification, heterogeneous enhancement, and destruction or thinning of bony walls (64 of 71 cases). Most reported masses were localised to only one nasal cavity and the maxillary sinus (64 of 71 cases). Surgical procedures typically consisted of endoscopic sinus surgery alone (38 of 52 cases), the Caldwell–Luc procedure in conjunction with endoscopic sinus surgery (5 of 52 cases) or the Caldwell–Luc procedure alone (6 of 52 cases). There were no reports of recurrence following any of these surgical procedures.
In the present study, patients one and two had no confirmed pre-operative pathological diagnosis, so we chose a Caldwell–Luc procedure in order to provide better intra-operative exposure and bleeding control. Haemorrhage appeared to have occurred around the natural ostium of the maxillary sinus, consistent with the histology of the basal portion of the mass. The surgical time and extent of bleeding were influenced by the degree of destruction around the natural ostium of the maxillary sinus, by the size of the mass, and by its adhesion to surrounding tissue.
Endoscopic sinus surgery was found to permit easier management of the basal portion of the maxillary sinus haematoma; moreover, it is less invasive. In our experience, endoscopic sinus surgery also reduced the amount of bleeding and the duration of surgery, compared with the Caldwell–Luc procedure; we would thus recommend it for similar cases.Reference Song, Jang, Chung and Lee7, Reference Lee, Smoker, Lee, Kim and Cho8 However, use of the sublabial approach (Caldwell–Luc procedure) in combination with endoscopic sinus surgery is preferred when uncontrollable bleeding is encountered or anticipated.Reference Song, Jang, Chung and Lee7–Reference Suzuki, Inaba, Hiraki, Hashida, Wakasugi and Kadokawa9 Regardless of the approach, organised haematomas can be completely removed, resulting in clinical cure.
The aetiology of organised haematoma development within the maxillary sinus has not been elucidated, but a hypothesis has been proposed. The underlying mechanism is thought to be a ‘vicious cycle’ of inflammation and bleeding due to trauma.Reference Kusunoki, Tokuno, Toshikawa and Murata5 The formation of an organised haematoma is believed to begin with a bleeding diathesis, trauma, nasal surgery or haemorrhagic lesion(s) in the maxillary sinus, which may predispose the individual to haematoma formation. A ruptured aneurysm or inflammatory erosion of the arterial branches supplying the maxillary sinus may then result in a collection of blood in the maxillary sinus. Finally, irrespective of the initial processes, the formation of a fibrous capsule around the haematoma prevents its resorption and results in neovascularisation with recurrent intracapsular bleeding (Figure 4).Reference Yoon, Kim and Cho10, Reference Ozaki, Sakai and Ikeda11 However, a review of the literature revealed many case reports, not all of which supported this hypothesis.

Fig. 4 Schematic representation of the ‘vicious circle’ of organised haematoma formation. First, vessels are dilated due to trauma and/or inflammation, followed by haemorrhage. Then, ecchymoma and blood clots form in the dilated vessels. Finally, necrosis, fibrosis, hyalinisation, neovascularisation and vascular dilatation occur in turn. Based on Ozaki and colleagues' proposal.Reference Ozaki, Sakai and Ikeda11
The observations from the current study, in conjunction with a literature review, led us to propose a revised hypothesis for the aetiology of organised haematoma of the maxillary sinus. Initially, inflammation, trauma, and/or an anomalous venous return in the vicinity of the maxillary sinus natural ostium result in dilated vessels, which may aggregate. Subsequently, red blood cells and fibrin leak out of the dilated vessels through gaps between endocapillary cells, allowing clots and necrotic tissue to collect at the periphery of the developing haematoma, around the natural ostium. Next, pseudovessels extend from endocapillary vessels into the peripheral necrotic tissue. These pseudovessels mimic a vascular pathway without endothelial cells, and contain red blood cells that are easier to exude. Therefore, fibrin and necrotic tissue gradually develop around the pseudovessels. Repetition of these processes results in the progressive development of an organised haematoma (Figure 5).
• Three cases of surgically resected maxillary sinus organised haematoma are presented
• The histopathology of the basal and peripheral haematoma parts differed
• The basal part comprised aggregated, dilated vessels (around the sinus ostium), blood coagulum, necrotic tissue and pseudovessels arising from endocapillary vessels
• Organised haematoma may propagate from blood component exudation, initially via leaky endothelial cells and later from in-growing pseudovessels

Fig. 5 Schematic representation of a modified proposal for the generation of organised haematoma of the maxillary sinus. In the basal portion of the haematoma, vessels around the natural ostium of the maxillary sinus are dilated by inflammation and trauma. These dilated vessels then aggregate. Red blood cells and fibrin seep out through the gaps between endothelial cells, producing a mass of fibrin and necrotic tissue. Subsequently, pseudovessels grow from endocapillary cells into the necrotic tissue, giving rise to further exudation of blood components.
The hypothesis advocated by Ozaki et al. appears to be consistent with the first stage of the above, new hypothesis.Reference Ozaki, Sakai and Ikeda11 Our revised theory appears to fit reported cases with respect to clinical features, CT and MRI appearances, pathological findings, and surgical treatments.Reference Lee, Park and Heo2, Reference Nagato, Sugahara, Watanuki, Tanaka, Mikuriya and Hashimoto3, Reference Song, Jang, Chung and Lee7–Reference Suzuki, Inaba, Hiraki, Hashida, Wakasugi and Kadokawa9, Reference Unlu, Mutlu, Ayhan and Tarhan12
Conclusion
This paper presents three cases of organised haematoma of the maxillary sinus.
It also proposes a new hypothesis that such organised haematomas originate from abnormal vessels around the natural ostium of the maxillary sinus. Gaps between vascular endothelial cells enlarge due to dilatation of vessels, enabling red blood cells and fibrin to seep out and form necrotic coagulum that gradually expands peripherally. In addition, pseudovessels grow through the fibrin and necrotic tissue and deliver exudate, including additional fibrin and necrotic tissue, resulting in expansion of the organised haematoma.
Acknowledgements
The authors gratefully acknowledge the contribution of Drs Junichi Ishikawa, Yuka Baba, Atsushi Tahara, Sunao Tanaka and Atsushi Ohata to this paper.








